Extra-corporeal therapies in Resp Failure
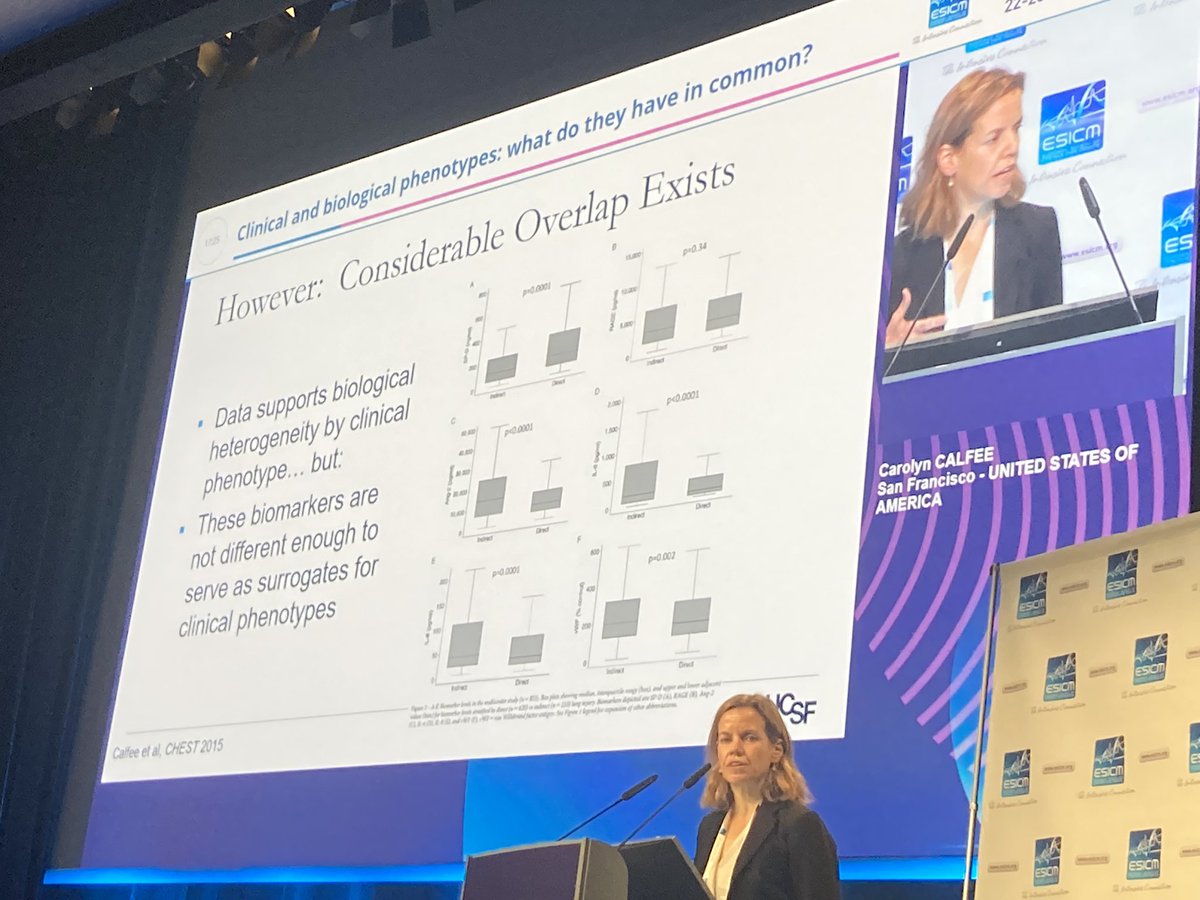
@CarolynCalfee
- Phenotypes in ARDS
Many phenotypes in ARDS: severity of ARDS, aetiology,
- physiologic
- does any of this response to differently to ECMO?
#LIVES2022
#ventilation
#extracorpreal @ESICM
@CarolynCalfee
- Phenotypes in ARDS
Many phenotypes in ARDS: severity of ARDS, aetiology,
- physiologic
- does any of this response to differently to ECMO?
#LIVES2022
#ventilation
#extracorpreal @ESICM
@CarolynCalfee @ESICM Severe ARDS phenotypes EOLIA using P/F ratio
- within 1st 7 days
- within this, which pt benefits most.
Meta-analysis on ECMO patients
- multiple subgroups but none of them statistically significant
- only key difference is No of organ failure . >2 ecmo less likely to work
- within 1st 7 days
- within this, which pt benefits most.
Meta-analysis on ECMO patients
- multiple subgroups but none of them statistically significant
- only key difference is No of organ failure . >2 ecmo less likely to work
@CarolynCalfee @ESICM so how about ECCO2R?
- if benefit drives from decreasing lung injury
- then high dead space or low compliance patients could be benficial
- Goligher AJRCCM 2017
pubmed.ncbi.nlm.nih.gov/28636403/
- physiologic modelling seems to work
- what about in trial : SUPERNOVA trial.
- if benefit drives from decreasing lung injury
- then high dead space or low compliance patients could be benficial
- Goligher AJRCCM 2017
pubmed.ncbi.nlm.nih.gov/28636403/
- physiologic modelling seems to work
- what about in trial : SUPERNOVA trial.
@CarolynCalfee @ESICM patient with lowest compliance associated with largest change in delta P on ECCOR
pubmed.ncbi.nlm.nih.gov/30790030/
pubmed.ncbi.nlm.nih.gov/30790030/
Then comes REST trial
- low TV + ECCOR vs. conventional low TV
-early acute resp failure
stopped early for futility
- no difference based on ARDS, severity
- ECCOR has higher mortality. no effects in subgroups based on compliance.
pubmed.ncbi.nlm.nih.gov/34463700/
- low TV + ECCOR vs. conventional low TV
-early acute resp failure
stopped early for futility
- no difference based on ARDS, severity
- ECCOR has higher mortality. no effects in subgroups based on compliance.
pubmed.ncbi.nlm.nih.gov/34463700/
Why does REST trial not work ?
- not sure
- may be off-target effects and risks
- patient not all ARDS , P/F <150.
So now what about COVID 19 ards?
- repeatedly asked this questions at many icm meetings.
- older age, later stage of pandemic, steroids ~ poor outcomes.
- not sure
- may be off-target effects and risks
- patient not all ARDS , P/F <150.
So now what about COVID 19 ards?
- repeatedly asked this questions at many icm meetings.
- older age, later stage of pandemic, steroids ~ poor outcomes.
Target Trial Emulation n = 7345 , observation data "emulated" as RCT
- 1': ECMO for all pts with PF<80
would have reduced mortality
- 1': ECMO for all pts with PF<80
would have reduced mortality
What about if we use delta P as indication for ECMO
- if delta p > 15 + ECMO, then likely significant benefit.
ECMO most effective in young, obese, when started early.
NOTE : not an RCT data and emulation data.
- if delta p > 15 + ECMO, then likely significant benefit.
ECMO most effective in young, obese, when started early.
NOTE : not an RCT data and emulation data.
On this note re:COVID 19 phenotypes
work by @drjzhn and Luigi C's team
pubmed.ncbi.nlm.nih.gov/33487454/
3 phenotypes : hypoinflammatory has lowest mortality
- need external validation but potential biological heterogeneity
work by @drjzhn and Luigi C's team
pubmed.ncbi.nlm.nih.gov/33487454/
3 phenotypes : hypoinflammatory has lowest mortality
- need external validation but potential biological heterogeneity
@drjzhn Biological phenotypes
- v little data on biological phenotypes
- biological phenotypes defined in "typical " ARDS
- e.g., hyper v hypoinflammatory phenotypes
- have differential responses to steroids, fluids, simvastatin
- what about ECMO ?
thelancet.com/series/ARDS-20…
- v little data on biological phenotypes
- biological phenotypes defined in "typical " ARDS
- e.g., hyper v hypoinflammatory phenotypes
- have differential responses to steroids, fluids, simvastatin
- what about ECMO ?
thelancet.com/series/ARDS-20…
@drjzhn pubmed.ncbi.nlm.nih.gov/31385880/
- observational tudy of 16 pts severe ARDS on ECMO
- switch from LTVV to ultra protective ventilation at 3ml/kg
- biomarkers change
-jury is still out but fascinating
- observational tudy of 16 pts severe ARDS on ECMO
- switch from LTVV to ultra protective ventilation at 3ml/kg
- biomarkers change
-jury is still out but fascinating
@drjzhn Now 2' analysis of ARMA trial
- HIGH plasma RAGE
- LTVV most effective in high sRAGE patients.
pubmed.ncbi.nlm.nih.gov/31385880/
- HIGH plasma RAGE
- LTVV most effective in high sRAGE patients.
pubmed.ncbi.nlm.nih.gov/31385880/
@drjzhn Might hyper-inflammatory phenotype benefit from ECMO/ECCO2R
- MIGHT is key word.
- need larger studies with extensive clinical data set and bio-repositories.
- what we know definitively : early very severe ARDS benefits most in younger, high driving pressure, obese pts
- MIGHT is key word.
- need larger studies with extensive clinical data set and bio-repositories.
- what we know definitively : early very severe ARDS benefits most in younger, high driving pressure, obese pts
@drjzhn Essentially we would need a prospectively collected bio-marker repository and a large sample to answer this questions -- aka likely difficult. Private sector working on biomarekers but not sure performance in bedside.
@drjzhn @threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh