
ICU stories: You get a call from outside 🏥 to accept a middle-aged pt w DM2/HTN/HLD/some type of solid Ca on chemo/obesity who presented to their ED w weakness/anxiety/"feeling cold". Vitals: BP 80-100, HR 130s (sinus tach), afebrile, Sat 100% on room air. Labs: WBC 13K, ...
... Lactate 5.2, creat 1.3. UA w some WBCs/bacteria. CXR clear. Norepi drip ordered but cancelled after BP improved to mid-90s, HR fell to 120s, & lactate ⬇️ to 2.5. What's your next step?
The discussion went like this:
Me: I will be happy to accept but I have no idea what we are treating. If it is sepsis, the source is unclear. And what about PE? Can you pls get a CT before sending?
ED: Sure, will do it. Thanks.
You go home & next am you learn that the CT showed:
Me: I will be happy to accept but I have no idea what we are treating. If it is sepsis, the source is unclear. And what about PE? Can you pls get a CT before sending?
ED: Sure, will do it. Thanks.
You go home & next am you learn that the CT showed:
👆saddle PE w clot extending to the R+L pulmonary artery & segmental arteries w concern of RV dilation. Patient was given tPA & was transferred to our ICU. Never required supplemental O2. BP stabilized & HR ⬇️ to 100-110. I reviewed the ECGs pre- & post-tPA during our am rounds: 



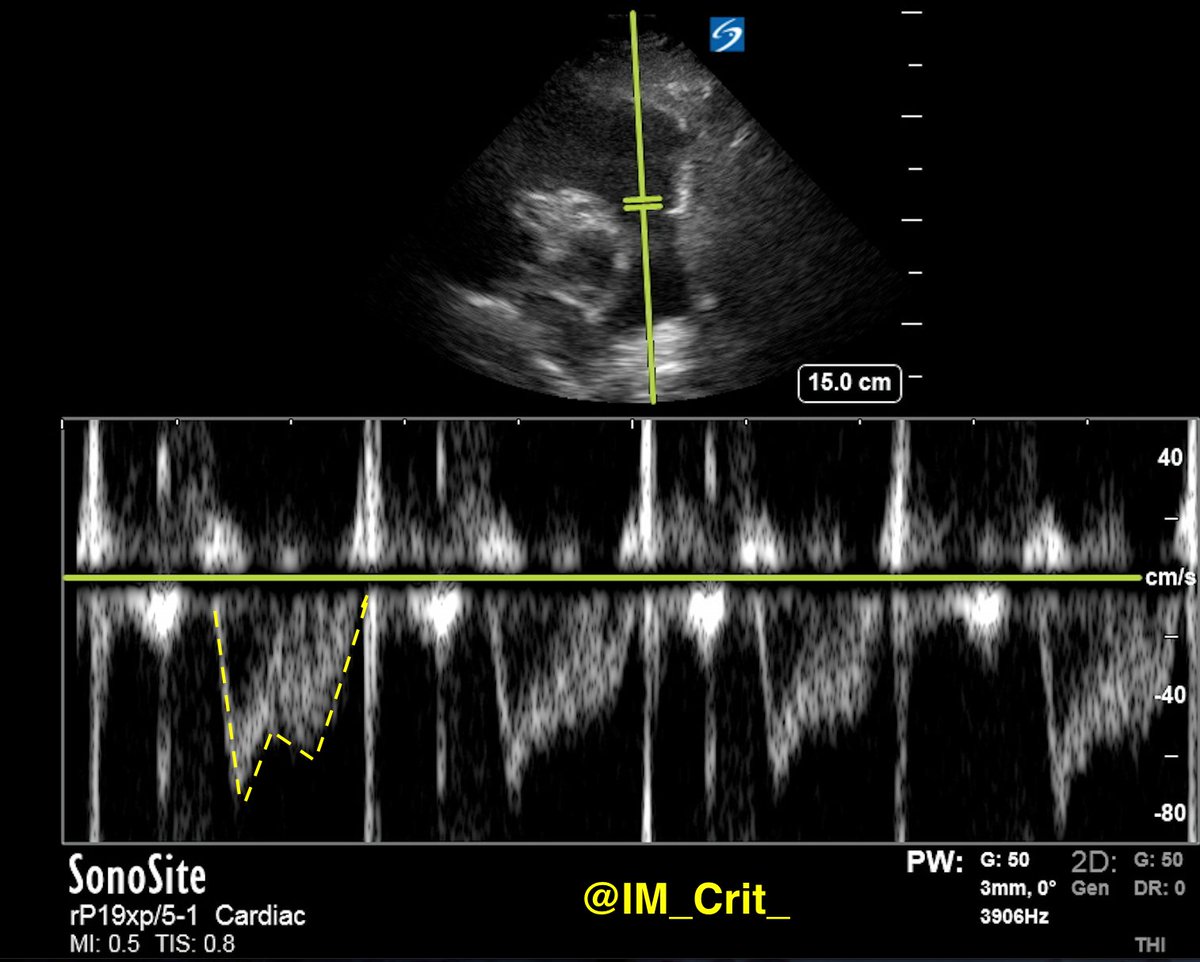
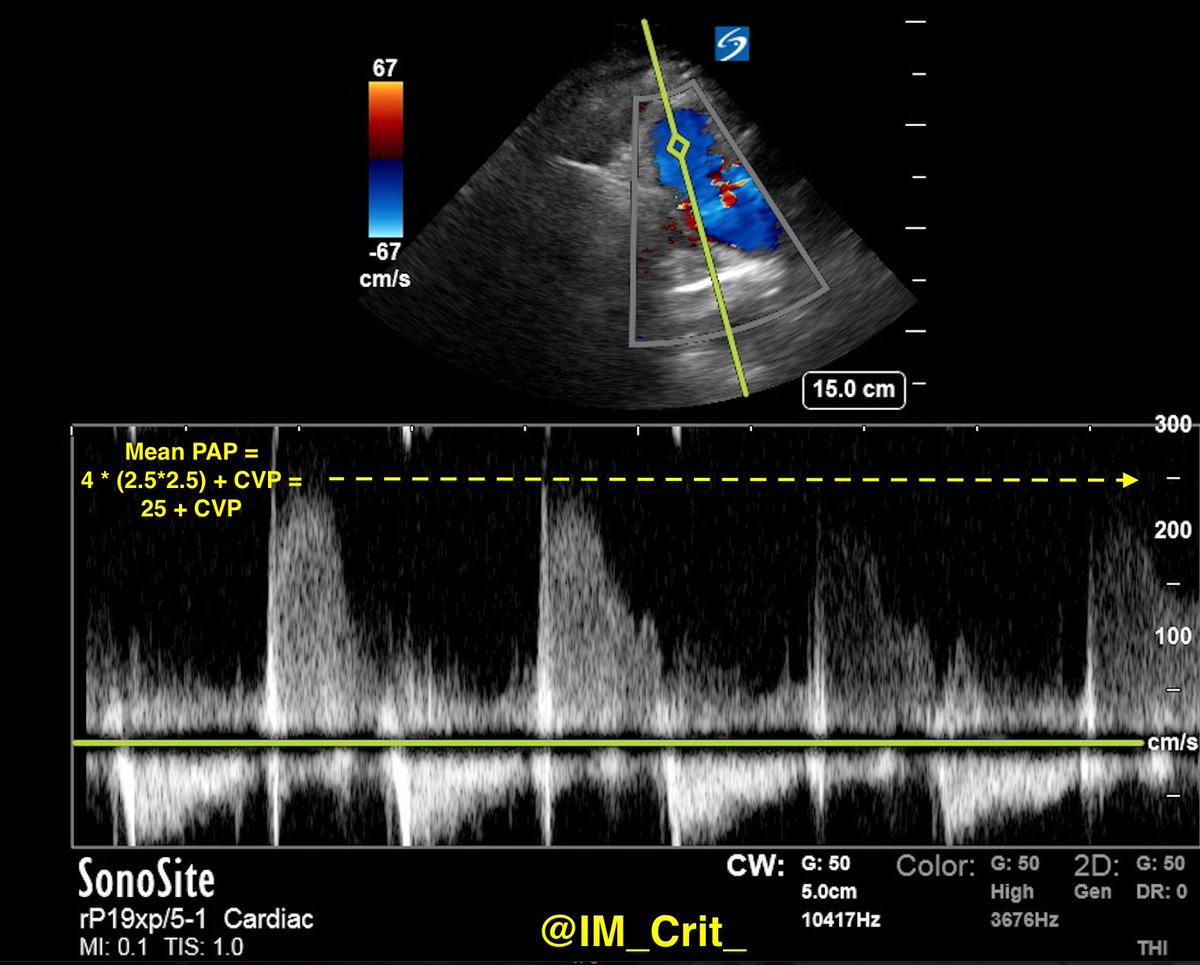
👆Obviously in a busy ED, some worrisome ECG findings were missed. Twelve hours post-tPA infusion & with the patient in our ICU, I did POCUS:
RV was still "suffering" (LV suffering too...; please notice D-shaped LV), probably still McConnell's sign. Can you guess what the IVC looked like? Tip: patient was breathing easily
What do you think now?
The IVC looks surprisingly "thin", right? Could I trick myself and you? Yes. I can almost hear my #VEXUS friends... With the "cylinder effect", if I cut the IVC in an oblique, off-axis plane, I can falsely narrow its diameter (image from: radiologykey.com/inferior-vena-…): 

Only, I didn't... 🤷♂️ Let's see the transverse view:
IVC was not dilated... Formal TTE confirmed POCUS findings & a formal lower extremity venous Doppler ruled out DVT. But it does NOT hurt if the intensivist performs venous POCUS, right?
What do you think for this 👆 left popliteal vein (artery in the left side, vein in the right side of the image)?
My interpretation is that there was DVT. The L popliteal vein was not just non-compressible; the clot itself could be seen... 🤷♂️
Take-home messages:
1. PE is a very sneaky diagnosis. We, as intensivists, have a terrible bad record and we miss the diagnosis quite often
2. Requring no supplemental O2 does not rule out PE, even a massive one!
3. Decreasing lactate should not make you feel better, especially
1. PE is a very sneaky diagnosis. We, as intensivists, have a terrible bad record and we miss the diagnosis quite often
2. Requring no supplemental O2 does not rule out PE, even a massive one!
3. Decreasing lactate should not make you feel better, especially
if the diagnosis is unclear
4. When you accept a patient for transfer to the ICU, you have to start thinking/working from that moment. We can all agree that it would not be fun if the patient had coded in the ambulance (or upon ICU arrival)
5. The more you use POCUS, the more
4. When you accept a patient for transfer to the ICU, you have to start thinking/working from that moment. We can all agree that it would not be fun if the patient had coded in the ambulance (or upon ICU arrival)
5. The more you use POCUS, the more
you will find yourself "disagreeing" with formal studies. That's OK. Use it as a learning opportunity (for all).
Thanks for reading!
Thanks for reading!
If you made it so far and you are a #POCUS fan, you deserve bonus spectral Doppler images from the RVOT/pulmonary artery (including mid-systolic notching): 

Thanks again!
#POCUS #ECHOFIRST #POCUSpeeps #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedTwitter #MedEd #EMBound @ACEP_EUS @MetroHealth_EM @MH_EMultrasound @jminardi21 @ThinkingCC @RJonesSonoEM @jaffa_md @katiewiskar @kyliebaker888 @TomJelic @msiuba @siddharth_dugar @thepocusatlas
#POCUS #ECHOFIRST #POCUSpeeps #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedTwitter #MedEd #EMBound @ACEP_EUS @MetroHealth_EM @MH_EMultrasound @jminardi21 @ThinkingCC @RJonesSonoEM @jaffa_md @katiewiskar @kyliebaker888 @TomJelic @msiuba @siddharth_dugar @thepocusatlas
@NephroP @HeyDrNik @ICUltrasonica @khaycock2 @NickjohnsonMD @EmergenxyPhysic @DraHuerta09 @pocusmeded @POCUSClub @thepocusatlas @AmbrizMau @ecocritic_es @TaotePOCUS @NephroGuy @pocusfoamed @interconsulta @EmergencyEcho @echotalk @cianmcdermott @ImagenCardiaca
@apenarEM @PorrosE @chileanestesia @vaszochios @nickmmark @cjosephy @pdsalinas @GUH_ICU_Anaesth @KalagaraHari @UAlberta_Sono @EMUGs_ @UAlberta_ICU @UAB_Sono @MDBeni @MonaresTI @EMUGs_ @MedCriticaMex @critconcepts @pablitorf @MediCasos @EM_Resus @ultra2ente @ACEP_EUS
@ImagenCardiaca @RosenelliEM @FisioPocus @MegriMohammed @emily_fri @icmteaching @curromir @iceman_ex @ThinkingCC @Wilkinsonjonny @Thind888 @smuramed @FSotoMD #MedStudentTwitter
Clarification: the reason for transfer was “severe sepsis/septic shock”
• • •
Missing some Tweet in this thread? You can try to
force a refresh







