1/Hate it when one radiologist called the stenosis mild, the next one said moderate--but it was unchanged?!
Here’s a #tweetorial of a lumbar grading system that’s easy, reproducible & evidence-based
#medtwitter #spine #neurosurgery #radres #neurorad #meded #FOAMed #FOAMrad
Here’s a #tweetorial of a lumbar grading system that’s easy, reproducible & evidence-based
#medtwitter #spine #neurosurgery #radres #neurorad #meded #FOAMed #FOAMrad
2/Lumbar stenosis has always been controversial. In 2012, they tried to survey spine experts to come to a consensus as to what are the most important criteria for canal & foraminal stenosis. And the consensus was…that there was no consensus. So what should you use to call it? 

3/Well, you don’t want just gestalt it—that is a recipe for inconsistency & disagreement. But you don’t want to measure everything either—measurements are not only cumbersome, they introduce reader variability & absolute measurements don’t mean the same thing in every patient. 

4/Think of it functionally. Nerves need to fit in their space, like you fit in clothing. Mild stenosis is like comfy clothes—no squeezing. Moderate stenosis clothing isn’t loose, but there isn’t extra room either. Severe stenosis is like too tight jeans, your body gets compressed 

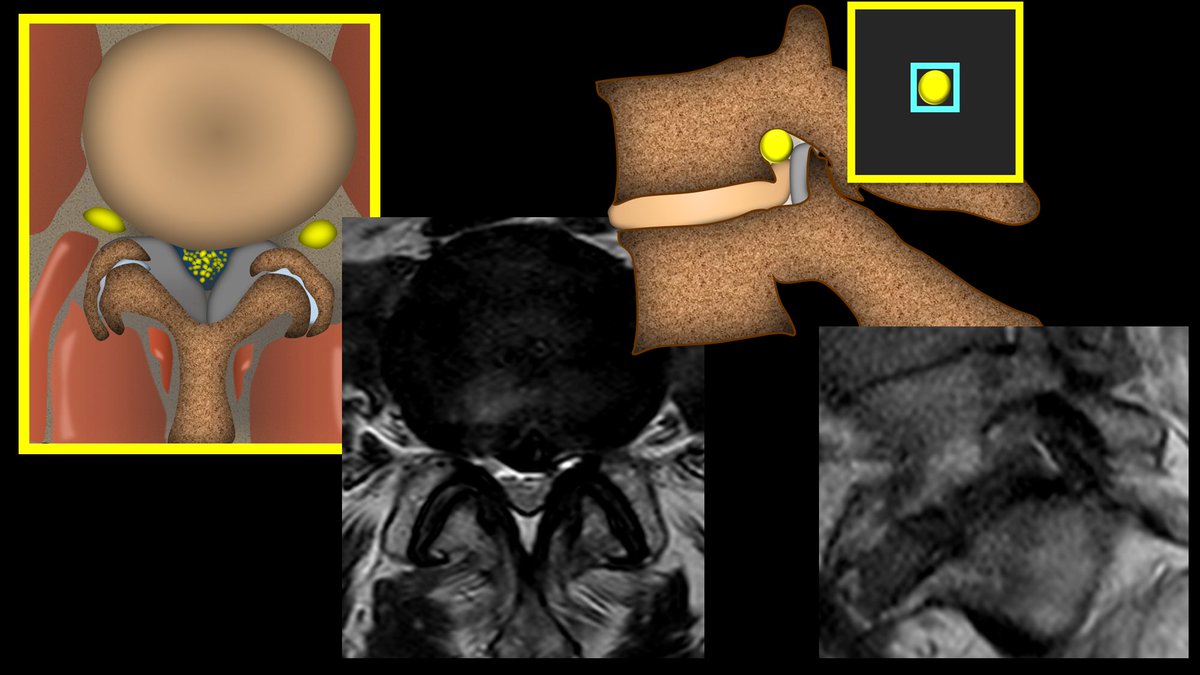
5/So how do we tell if the nerves have enough room—if the clothing fits loosely, tight, or too tightly? We look at the space around them. For the canal, it is CSF—if there's enough room, extra space will be filled by CSF. For foramina, it is fat—extra room is filled by fat. 

6/For mild canal stenosis, there is mild attenuation of the CSF space, but there is still plenty of CSF around, just like there is plenty of room in your comfy sweat pants 

7/For moderate canal stenosis, the canal starts closing in, so there is less CSF around and the nerve roots appear aggregated. It’s like the clothes you wear to the club, there isn’t much room between your skin & the clothing, but you can still fit into them (hopefully) 

8/Severe canal stenosis is the too tight jeans. The canal doesn’t just hug up to the nerve roots, it compresses them. Like your belly after a big meal trying to get into tight jeans, they get squished and deformed in order to fit, so they can’t be separated from each other. 

9/This classification isn’t just easy to remember, it’s also evidence based. This is the Lee classification that has excellent reproducibility not just among radiologists, but among everyone. And it does correlate w/increasing symptoms. 

10/For foraminal narrowing, the nerve inside the foramen has fat around it on four sides that can be attenuated as the space gets tighter. How many sides are attenuated determines how severe the stenosis is. 

11/Mild stenosis is where you have loss of the fat on 2 sides. So it is still comfy clothing bc the fat is preserved on the other two sides, so you still have lots of space. 

12/For moderate stenosis, you lose the space on all four sides, but the nerve itself is not compressed or deformed. Like a sleek outfit, it shows your curves, but doesn’t deform them. It’s not a comfy outfit, per se, & I wouldn’t eat a lot while wearing it, but it’s not too small 

13/For severe stenosis, we are trying to fit into those jeans from high school and it isn’t going well. You are squishing in everything you can to get it to fit. Same with the foramen—the fat isn’t just gone, the nerve is compressed and deformed. 

14/This is also named the Lee system. It fits well with the Lee classification for canal stenosis. It also is extremely reproducible and correlates with findings at surgery.
So you don’t have to remember a complicated system—just ask yourself, how does the clothing fit?
So you don’t have to remember a complicated system—just ask yourself, how does the clothing fit?

15/So put away your measuring calipers! You can end the inter-observer variability. These systems are easy to remember, make sense, and are based in evidence. As they say, if it fits—wear it! 

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















