🚨 NEW! Lean Mass Hyper-Responder Editorial🚨
👉 10 MD & PhD authors from 4 countries🌍coming together for 1st of it's kind Consensus Statement on #LMHR
👉 Published in official Journal of the National Lipid Association @LipidJournal
A thread 🧵👇
authors.elsevier.com/a/1g22A6tb2E2O…
👉 10 MD & PhD authors from 4 countries🌍coming together for 1st of it's kind Consensus Statement on #LMHR
👉 Published in official Journal of the National Lipid Association @LipidJournal
A thread 🧵👇
authors.elsevier.com/a/1g22A6tb2E2O…

2/ A bit of background to catch some of you up
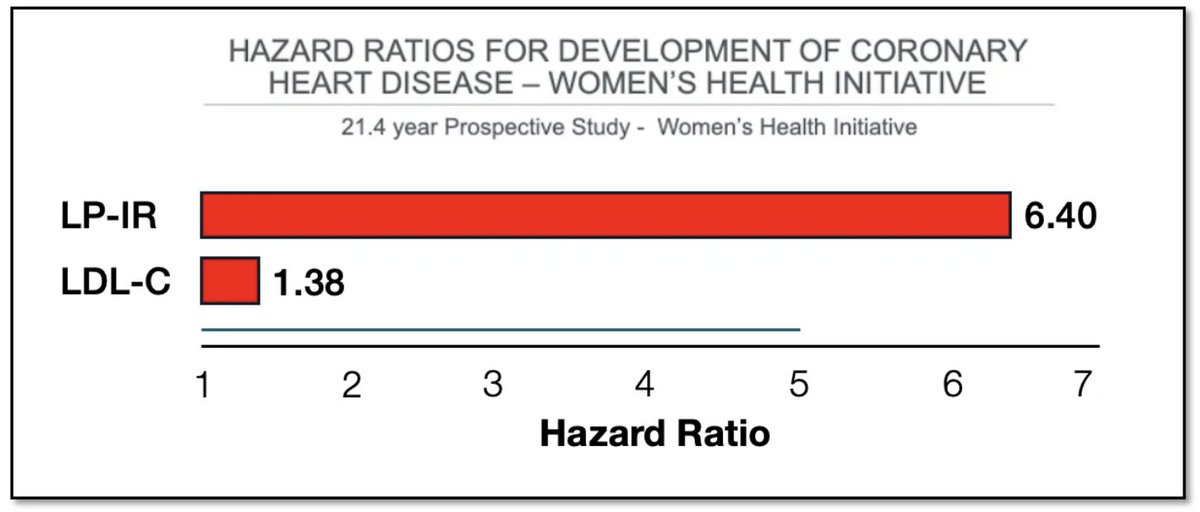
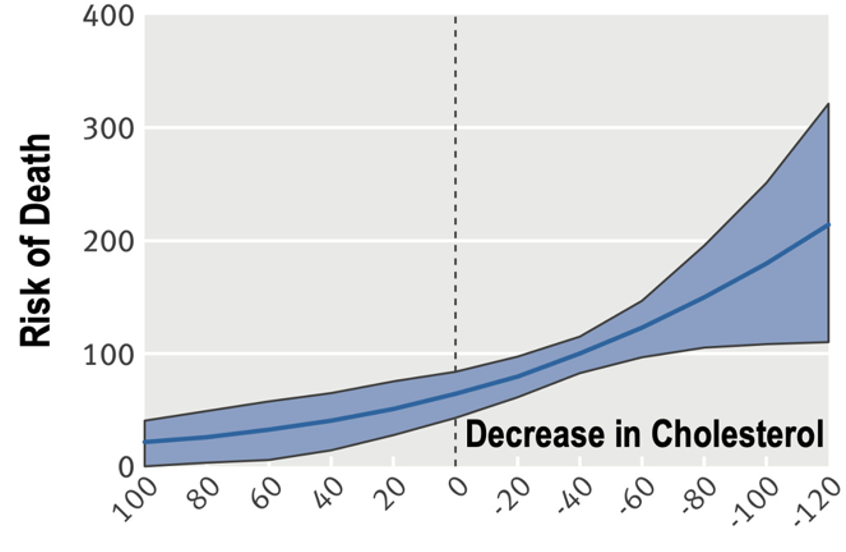
Over the past 6 years a population of people has emerged who demonstrate ⬆️ LDL on a #ketogenic diet in the context of ⬇️TG +⬆️HDL
Phenotype was first observed by @realDaveFeldman and (historically) named Lean Mass Hyper-Responders
Over the past 6 years a population of people has emerged who demonstrate ⬆️ LDL on a #ketogenic diet in the context of ⬇️TG +⬆️HDL
Phenotype was first observed by @realDaveFeldman and (historically) named Lean Mass Hyper-Responders

3/ 1 year ago, we started researching #LMHR more formally, and in this year, we've published 4 prior papers
Cohort Study
pubmed.ncbi.nlm.nih.gov/35106434/
Case Report
pubmed.ncbi.nlm.nih.gov/35498420/
Cholesterol drop protocol
pubmed.ncbi.nlm.nih.gov/35938774/
Lipid Energy Model
pubmed.ncbi.nlm.nih.gov/35629964/
Cohort Study
pubmed.ncbi.nlm.nih.gov/35106434/
Case Report
pubmed.ncbi.nlm.nih.gov/35498420/
Cholesterol drop protocol
pubmed.ncbi.nlm.nih.gov/35938774/
Lipid Energy Model
pubmed.ncbi.nlm.nih.gov/35629964/
4/ With this editorial we take the NEXT STEP in providing an expert consensus of 10 MD + PhD authors on topic of #LDL in #LMHR on a #ketodiet, including incredibly highly respected members of the Lipidology community
authors.elsevier.com/a/1g22A6tb2E2O…
authors.elsevier.com/a/1g22A6tb2E2O…
5/ Major take-aways:
A prudent PATIENT-CENTERED clinical approach is required for managing #LMHR patients
The #LMHR phenomenon deserves FURTHER RESEARCH, both on mechanism and risk, and has potential to teach us much about human lipid metabolism and ASCVD
A prudent PATIENT-CENTERED clinical approach is required for managing #LMHR patients
The #LMHR phenomenon deserves FURTHER RESEARCH, both on mechanism and risk, and has potential to teach us much about human lipid metabolism and ASCVD
6/ Some of my favorite linesare as follows 👇
"LMHR provide[s] a unique opportunity to understand LDL-c dynamics beyond what has previously been possible”
“where there are competing medical conditions, weighing of treatment options should be an individual matter”



"LMHR provide[s] a unique opportunity to understand LDL-c dynamics beyond what has previously been possible”
“where there are competing medical conditions, weighing of treatment options should be an individual matter”




7/ It was a true pleasure to put together this editorial with my coauthors @MichaelMindrum, Dr. Giral, Professor Anatol Kontush, @AdrianSotoMota, @DrRagnar (Tommy Wood), @DominicDAgosti2, Dr. Manubolu, @BudoffMd, and Dr. Ronald Krauss. I cannot speak highly enough of this team 

8/ I also want to give a HUGE shout out to the LMHR Facebook group + @realDaveFeldman who collectively helped to fund the open access fee despite being blinded to article itself and purely out of a devotion to open-access science and in moving this particular discussion forward
9/ Also, check out Dave's 2:29 min video here. Always high production quality!
10/ I will have more to say on this editorial in the coming days and weeks, but for now I encourage you to read it for yourself (it's concise!) and help to amplify this important discussion! 🙏🙏🙏
authors.elsevier.com/a/1g22A6tb2E2O…
authors.elsevier.com/a/1g22A6tb2E2O…
• • •
Missing some Tweet in this thread? You can try to
force a refresh