#AKIConsultSeries:👨w T2DM➡️🏥 for fever, dysuria and CVA tenderness. On arrival: ⬇️BP, ⬆️Glucose, ⬆️AGMA. Dx UTI + DKA. Tx: Abx + Insulin Pump + 4 L Crystalloid + NE
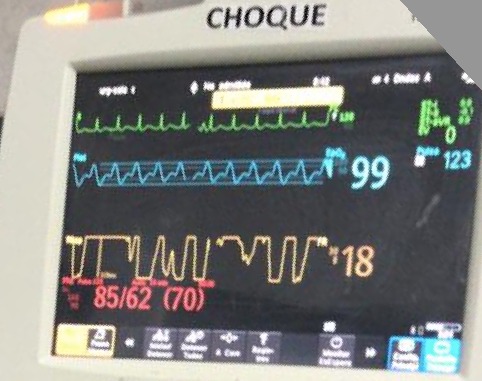
After resus, pt still oliguric, Cr 3.2. NE 0.7 ug/kg/min,🧠confused, BP 85/62, HR 123, 2L O2. CRT 4 sec
1/12
After resus, pt still oliguric, Cr 3.2. NE 0.7 ug/kg/min,🧠confused, BP 85/62, HR 123, 2L O2. CRT 4 sec
1/12
Given DKA, giving additional fluids is tempting. But before we do this, its easy to do a quick assessment of fluid tolerance #POCUS
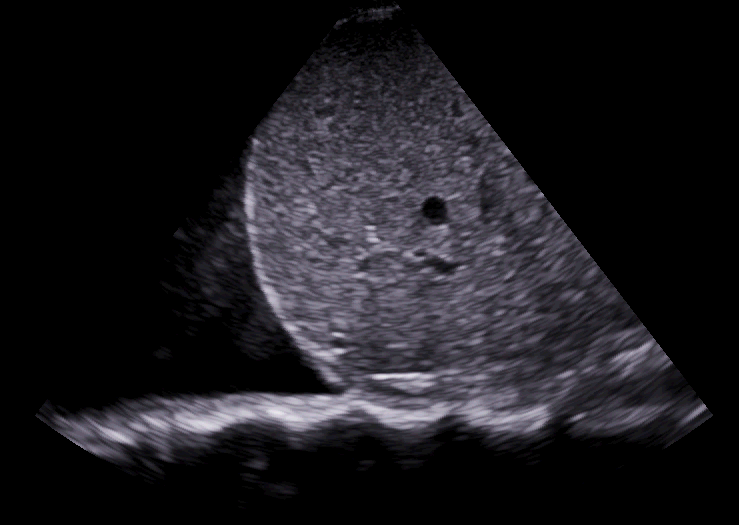
#LUS shows some B-lines (bilat)
#IVC plethoric w no respiratory collapse
#VExUS shows very pulsatile portal vein 🚨🤔
2/12
#LUS shows some B-lines (bilat)
#IVC plethoric w no respiratory collapse
#VExUS shows very pulsatile portal vein 🚨🤔
2/12
Pulse pressure is low (23!): This suggest a low cardiac output state!
Also, there are signs of fluid intolerance!
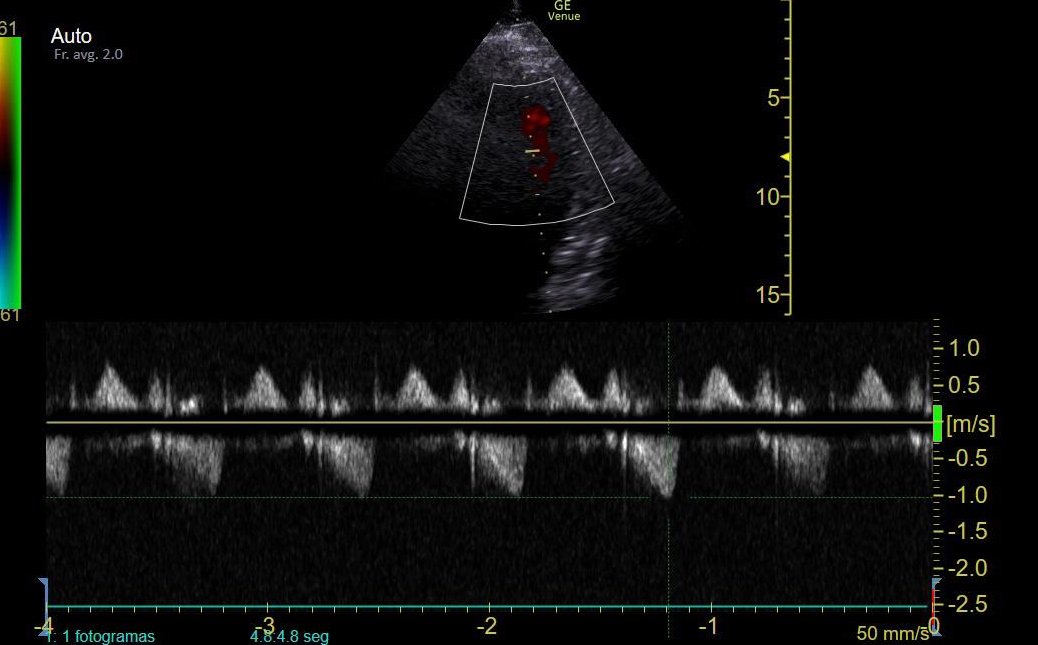
#EchoFirst: Window is suboptimal, but we see a Hyper-dynamic LV w small cavity and a turbulent flow (green color). There was no systolic RV failure
3/12
Also, there are signs of fluid intolerance!
#EchoFirst: Window is suboptimal, but we see a Hyper-dynamic LV w small cavity and a turbulent flow (green color). There was no systolic RV failure
3/12
The combination of sepsis, hyper-dynamic LV, small LV cavity w turbulent flow and LOW Pulse Pressure suggests the possibility of LV obstruction!
How to assess this?
Obstruction leads to increased blood velocity (think of thumb on a hose)...
4/12
How to assess this?
Obstruction leads to increased blood velocity (think of thumb on a hose)...
4/12

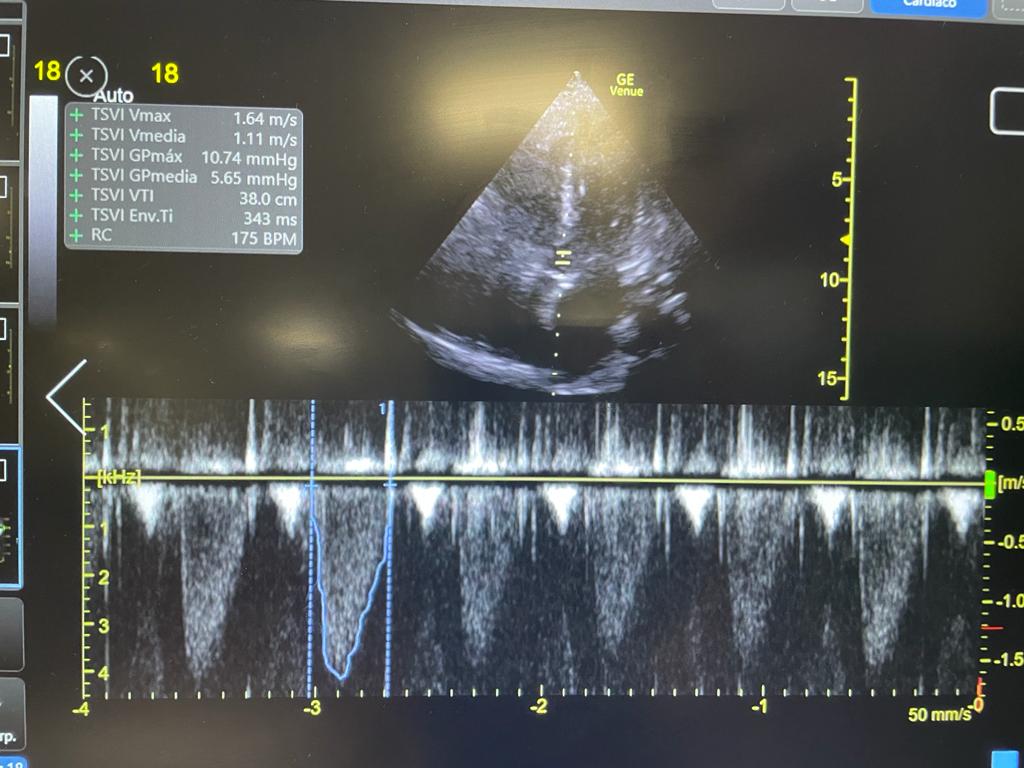
CW Doppler allows us to assess flow velocity and look for signs of obstruction
CW Doppler was performed with gate at LVOT and mid-cavity: Flow velocity > 5 m/s! (Velocity > 2.7 m/s is considered significantly elevated)
¿What could be causing this obstruction?
5/12

CW Doppler was performed with gate at LVOT and mid-cavity: Flow velocity > 5 m/s! (Velocity > 2.7 m/s is considered significantly elevated)
¿What could be causing this obstruction?
5/12


In a hyper-dynamic state, decreased LV filling can lead to systolic anterior motion of the mitral valve (SAM) and obstruct the outflow tract, there may also be mid-cavitary obliteration.
Sepsis and very high NE doses can create the ideal conditions for this to happen!
6/12

Sepsis and very high NE doses can create the ideal conditions for this to happen!
6/12


In this case, such a high velocity (>5 m/s) suggests I might be sampling a component of mitral regurgitation, so SAM might be happening here!
Since catecholamines worsen obstruction, a reasonable strategy is to switch to a vasopressor with no inotropism/chronotropism
7/12
Since catecholamines worsen obstruction, a reasonable strategy is to switch to a vasopressor with no inotropism/chronotropism
7/12

In this case we did not give any additional fluid. Stopped NE and started High Dose Vasopressin (0.2 U/min). On reassessment 2 hrs later this worked!
HR down to 111, and most significantly Pulse Pressure now 67!!!
Increased PP strongly suggests improved stroke volume!
8/12

HR down to 111, and most significantly Pulse Pressure now 67!!!
Increased PP strongly suggests improved stroke volume!
8/12


Also intra-ventricular gradient significantly improved and portal vein showed decongestion! (probably from improved cardiac output)!
**Shape suggests mid-ventricular gradient is still present (but definitely better than before)
9/12

**Shape suggests mid-ventricular gradient is still present (but definitely better than before)
9/12


48 hours later, as sepsis improved, pt was off pressors.
Both LVOT and Mid-Ventricular gradients disappeared (Velocity = 1 m/s) and Portal Vein was completely normal!
10/12


Both LVOT and Mid-Ventricular gradients disappeared (Velocity = 1 m/s) and Portal Vein was completely normal!
10/12


I found this case really interesting as this patient was likely fluid responsive even though he was NOT fluid tolerant!
More on Fluid Tolerance assessment here:
doi.org/10.1093/ehjacc…
11/12
More on Fluid Tolerance assessment here:
doi.org/10.1093/ehjacc…
11/12

A similar case that goes into more detail into the physiology of LV obstruction here:
12/12
12/12
https://twitter.com/ArgaizR/status/1389010137772400641?s=20&t=YlGROJ3PeG_ReuMyZl3Yzg
• • •
Missing some Tweet in this thread? You can try to
force a refresh