Like to present a case seen in 2017. We were not aware of the entity then. 17F, 15D vomiting, headache. No deficit. Evaluated at institute. Extensive blood/CSF/tropical diseases workup -ve. CSF: P81, G57, cell 30 (all L). IVMPS x 5gm. Discharged with Dx of ADEM. 1st CEMR. (1/8) 

8D later readmitted there w/ headache x 3D w/ mild rt ptosis. Again IVMPS x 3gm. Better. Again recurrence of headaches. Both times followup oral steroids not given. Came to us.
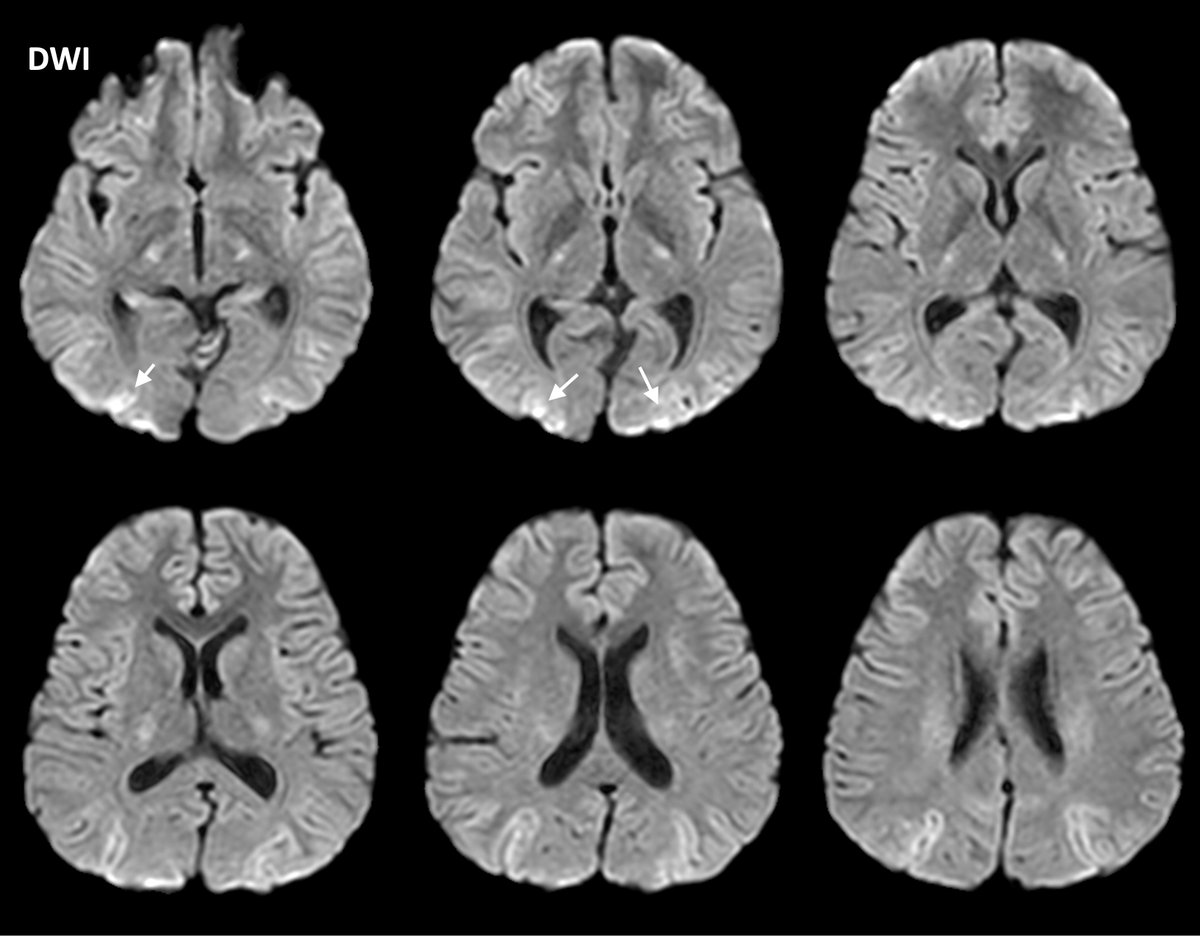
2nd CEMR. Similar findings. Slight increase in lesion burden. (2/8)
2nd CEMR. Similar findings. Slight increase in lesion burden. (2/8)

MR looked odd. We had never seen before. Googled. This paper surfaced. (3/8) pubmed.ncbi.nlm.nih.gov/20639547/ 

It talked about biopsy to confirm the Dx. Pt did not agree. We followed the suggestion of this article. Oral steroids + AZT. Developed steroids s/e, tapered to 10mg OD. 3rd CEMR (month4): lesions almost same. We had lost it we thought. (4/8) 

We remembered @sjauhar quote. (5/8) 

We followed his advice. IVMPS x 5gm. 1gm IVMPS x week. 20 mg MTX weekly. Continued 5mg oral prednisolone. 4th CEMR after 3 months: NORMAL. We tapered weekly IVMPS gradually, continued MTX & 5mg OD steroids. 5th CEMR also normal done after another 3 months (M10). (7/8) 

Later after we had been through this came this paper where he stressed about MTX in the Rx of CLIPPERS. Had we not sought help at that point of time, we would not have gained this knowledge ahead of times. (8/8)
academic.oup.com/brain/article/…
academic.oup.com/brain/article/…

@Sthanu5 @Brandon_Beaber @EMiddlebrooksMD @LyellJ @TylerAllisonMD @thecortexclub @MohitAgNeurorad @marignierro @DrCindyCooper @a_charidimou @Jagan1234 @HuttoSpencer @VMSilvera @drSurjthVattoth @PavanBhargavaMD #NeuroTwitter #MedTwitter #neurorad #neuroscience @LorenzoPinelli
@bobvarkey @theneuroradguy @rkchoi @Divyani_Garg @learnneurorad @caseyalbin @Narenmbbs @sudhir_kothari @hyderabaddoctor @GraceGombolayMD @OligoclonalBand @StaceyLClardy @mdsebaslopez #clippers
courtesy @drharunyildiz that is too good 

• • •
Missing some Tweet in this thread? You can try to
force a refresh