1/”I LOVE spinal cord syndromes!” is a phrase that has NEVER, EVER been said by anyone.
Never fear—here is a #tweetorial on all the incomplete #spinalcord syndromes!
#medtwitter #neurotwitter #neurology #neurosurgery #neurorad #radres #meded #FOAMed #FOAMrad #radtwitter #spine
Never fear—here is a #tweetorial on all the incomplete #spinalcord syndromes!
#medtwitter #neurotwitter #neurology #neurosurgery #neurorad #radres #meded #FOAMed #FOAMrad #radtwitter #spine

2/Spinal cord anatomy can be complex. On imaging, we can see the ant & post nerve roots. We can also see the gray & white matter. Hidden w/in the white matter, however, are numerous efferent & afferent tracts—enough to make your head spin. 

3/Lucky for you, for the incomplete cord syndromes, all you need to know is gray matter & 3 main tracts. Anterolaterally, spinothalamic tract (pain & temp). Posteriorly, dorsal columns (vibration, proprioception, & light touch), & next to it, corticospinal tracts—providing motor 

4/I think the layout looks like a guy doing jumping jacks. Gray matter centrally is the head. Spinothalamic tracts coming forward & anterior are the arms, while posteriorly, corticospinal tracts are the legs. Finally, all the way back, at the bottom, dorsal columns are the feet 

5/This way of remembering spinal anatomy makes sense. The gray matter should be the head—because where most of all your gray matter stored? In your head! So gray matter is the head of the jumping jacks guy. 

6/Extremities are the sensory tracts—makes sense, most sensation comes from the extremities. Arms/hands give you the most sensation (pain, burning=spinothalamic tract). Feet can feel big things, but mostly, they are there to help you balance (mainly proprioception=dorsal columns) 

7/Corticospinal tracts look like the legs, and this makes sense—legs are what propel you forward and move you. So the legs are for motion = motor = corticospinal tract 

8/An important point: The spinothalamic tract actually crosses in the gray matter to supply the OPPOSITE side.
So it does a fancy jumping jack. After tracts come together in the middle, they switch sides—like someone turning around 180 when they do jumping jacks
So it does a fancy jumping jack. After tracts come together in the middle, they switch sides—like someone turning around 180 when they do jumping jacks

9/First and most important cord syndrome is anterior or ventral cord syndrome. On imaging, you get a classic “owl eye” appearance.
I remember this is anterior cord syndrome bc someone w/owl eyes would be your lookout—and look outs are always in front or ANTERIOR.
I remember this is anterior cord syndrome bc someone w/owl eyes would be your lookout—and look outs are always in front or ANTERIOR.

10/Anterior cord syndrome is usually from anterior spinal artery occlusion, which supplies the anterior 2/3rds of the cord.
Usually it is from embolism/atherosclerosis, but can also be from occlusion of the feeder of the ASA that come from the aorta (aortic dissection/surgery)
Usually it is from embolism/atherosclerosis, but can also be from occlusion of the feeder of the ASA that come from the aorta (aortic dissection/surgery)

11/In anterior cord syndrome, you’ve lost 2rds of your body! Only the feet remain (dorsal columns).
What do feet do? Mainly feel the ground (proprioception, vibration) and a little sensation (light touch). That is all that is left w/anterior cord syndrome.
What do feet do? Mainly feel the ground (proprioception, vibration) and a little sensation (light touch). That is all that is left w/anterior cord syndrome.

12/Central cord syndrome is usually from trauma. Either true trauma or chronic trauma related to compression of the cord from degenerative changes/canal stenosis
(see my tweetorial on degenerative compression here:
(see my tweetorial on degenerative compression here:
https://twitter.com/teachplaygrub/status/1600511887460171778)

13/What is effected? Getting hit centrally is like getting punched centrally—in the stomach. Immediately your arms cross to protect your stomach & they get hit.
This is what happens in central cord syndrome, the crossing tracts of the arms (spinothalamic tracts) get hit.
This is what happens in central cord syndrome, the crossing tracts of the arms (spinothalamic tracts) get hit.

14/Hitting the crossing spinothalamic tracts gives you the classic cape distribution of pain in central cord syndrome.
This is easy to remember bc the spinothalamic tracts are the arms/hands—so it makes sense that if they get hit, you have pain along both arms/hands!
This is easy to remember bc the spinothalamic tracts are the arms/hands—so it makes sense that if they get hit, you have pain along both arms/hands!

15/Dorsal cord syndrome is where only the dorsal columns are involved. It looks like a little white mountain on imaging. Differential is extensive—and contains some real zebras.
I just remember that if I see a mountain in the cord, there is a mountain of differentials!
I just remember that if I see a mountain in the cord, there is a mountain of differentials!

16/Going back to our jumping jack guy—dorsal cord syndrome is having your feet cut off. You can still walk if you want—you have legs that you can fit into peg legs. But w/o feet to feel the ground, you will never quite have the same balance (loss of proprioception) 

17/Finally is hemi cord syndrome or Brown Sequard to the cool kids. Half of the cord is injured—usually from a penetrating trauma (knife, gunshot) that severs the cord in half. 

18/Now it gets complicated--this is the only unilateral syndrome. You have lost both your leg & your foot on that side. So you can’t move your leg on that side—it’s gone. Not even a stump to put a peg leg on. And w/o your foot, it is hard to feel the ground & balance on that side 
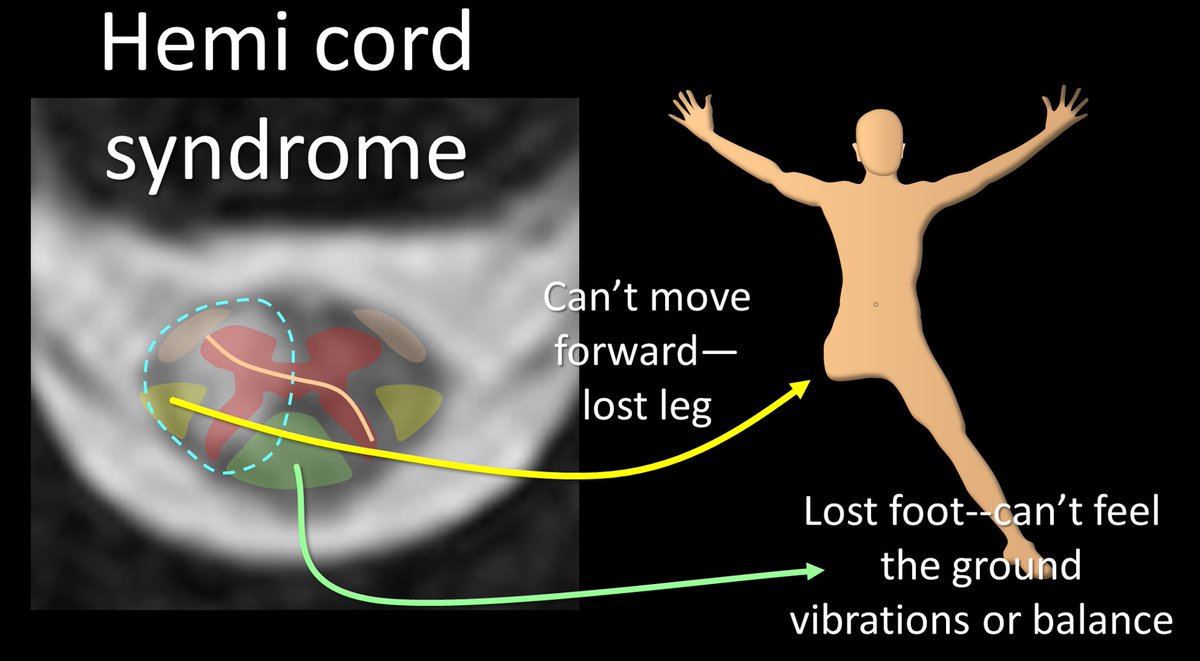
19/But you lose your PAIN sensation on the OPPOSITE side, b/c the spinothalamic tracts does its own 180 jumping jack & actually innervates the other side.
I remember this bc Spino Thalamic = Slip Through to the other side.
I remember this bc Spino Thalamic = Slip Through to the other side.

20/Now you know all the incomplete spinal cord syndromes and the jumping jack man anatomy behind them. So while you may never love them—at least you will always remember them! 

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















