1/
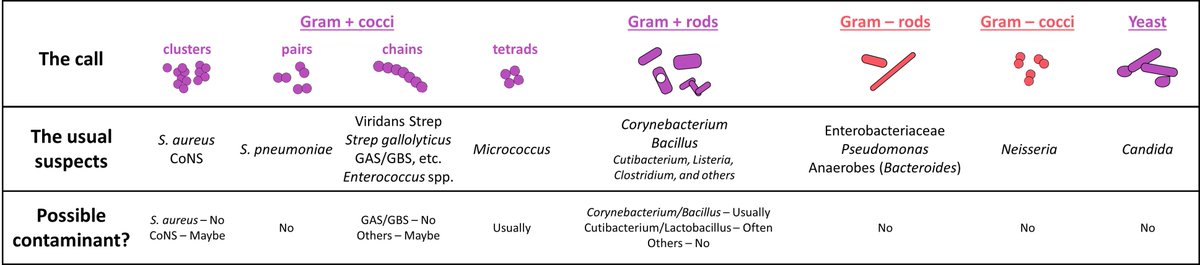
5pm. ID consults.
On 📞 giving recs re: culture growing Serratia.
Them: TY for seeing our patient!
You: Of course! BTW do you know the hx of Serratia? No? Well let me tell you about Operation Sea-Spray…
⌛️
Them: ...So should we start abx? Which one?
You: 😳
This week:
5pm. ID consults.
On 📞 giving recs re: culture growing Serratia.
Them: TY for seeing our patient!
You: Of course! BTW do you know the hx of Serratia? No? Well let me tell you about Operation Sea-Spray…
⌛️
Them: ...So should we start abx? Which one?
You: 😳
This week:
2/
So far @JenniferSpicer4 & I have explored consultant skills pertaining to the consult "ask".
We'll now focus on how to respond to the ask, verbally & through notes.
Let's start w/ a poll of those of you who CALL consults:
What is your PREFERRED way to receive consult recs?
So far @JenniferSpicer4 & I have explored consultant skills pertaining to the consult "ask".
We'll now focus on how to respond to the ask, verbally & through notes.
Let's start w/ a poll of those of you who CALL consults:
What is your PREFERRED way to receive consult recs?
3/
Previous studies suggest that verbal communication of consultant recs – especially initial recs - is preferred by most clinicians.
Additionally, lack of in-person interaction w/ consultants is one factor hospitalists identify as negatively impacting learning & patient care.
Previous studies suggest that verbal communication of consultant recs – especially initial recs - is preferred by most clinicians.
Additionally, lack of in-person interaction w/ consultants is one factor hospitalists identify as negatively impacting learning & patient care.

4/
Clearly, verbal communication is key. But I’m certain that we’ve all had experiences when verbal communication of recs went poorly.
(Don’t worry, #IDTwitter, I still love talking about Operation Sea-Spray! 🌉 🛥️ 🎈 🦠)
So, how can we get better at this skill intentionally?
Clearly, verbal communication is key. But I’m certain that we’ve all had experiences when verbal communication of recs went poorly.
(Don’t worry, #IDTwitter, I still love talking about Operation Sea-Spray! 🌉 🛥️ 🎈 🦠)
So, how can we get better at this skill intentionally?
5/
Let’s approach this w/ the frame of that tried-and-true #MedEd question: Where is the learner? (the person receiving the recs)
Think about WHERE in 3 domains:
1⃣ Where…in time/space (aka context)
2⃣ Where…in terms of prior knowledge
3⃣ Where…regarding the consult "ask"
Let’s approach this w/ the frame of that tried-and-true #MedEd question: Where is the learner? (the person receiving the recs)
Think about WHERE in 3 domains:
1⃣ Where…in time/space (aka context)
2⃣ Where…in terms of prior knowledge
3⃣ Where…regarding the consult "ask"

6/
Each domain influences HOW to deliver verbal recommendations.
1⃣ THEIR context shapes the CONCISENESS of your recs.
Keep it brief & to the point if the listener is:
🕟 At the end of their day/shift
📞 On the phone
🧠 Rounding, prepping for the OR, multitasking, etc.
Each domain influences HOW to deliver verbal recommendations.
1⃣ THEIR context shapes the CONCISENESS of your recs.
Keep it brief & to the point if the listener is:
🕟 At the end of their day/shift
📞 On the phone
🧠 Rounding, prepping for the OR, multitasking, etc.
7/
Establishing their context may seem obvious, but is often overshadowed by OUR agenda as consultants.
Sometimes this means…
🌟 Deferring the less urgent recommendations to another time or day
🌟 Saving the waxing poetic for the note
🌟 Making a plan to teach later
Establishing their context may seem obvious, but is often overshadowed by OUR agenda as consultants.
Sometimes this means…
🌟 Deferring the less urgent recommendations to another time or day
🌟 Saving the waxing poetic for the note
🌟 Making a plan to teach later
8/
2⃣ THEIR prior knowledge shapes how you FRAME the discussion & recs.
If what they know is limited:
☑️ Restate the "ask" (orient them)
☑️ PROVIDE a thought process
If what they know is rich:
✅ Clarify the "ask" (orient yourself)
✅ ADD to their thought process
2⃣ THEIR prior knowledge shapes how you FRAME the discussion & recs.
If what they know is limited:
☑️ Restate the "ask" (orient them)
☑️ PROVIDE a thought process
If what they know is rich:
✅ Clarify the "ask" (orient yourself)
✅ ADD to their thought process
9/
Here are some ways to establish the learner’s level of knowledge about the problem & patient.
Guiding principles:
💡 Don’t make assumptions (don’t we grumble when we hear “this patient is known to your service”?)
💡 Don’t probe the learner, probe their learning environment
Here are some ways to establish the learner’s level of knowledge about the problem & patient.
Guiding principles:
💡 Don’t make assumptions (don’t we grumble when we hear “this patient is known to your service”?)
💡 Don’t probe the learner, probe their learning environment

10/
Finally, 3⃣ THEIR perspective on the consult “ask” shapes your PITCH.
If you sense that they...
🤝 Are already thinking what you recommend ➡️ be empathic & affirming
🤷 Are deferring to what you think ➡️ be directive
🤔 Will disagree with you ➡️ be curious & collaborative
Finally, 3⃣ THEIR perspective on the consult “ask” shapes your PITCH.
If you sense that they...
🤝 Are already thinking what you recommend ➡️ be empathic & affirming
🤷 Are deferring to what you think ➡️ be directive
🤔 Will disagree with you ➡️ be curious & collaborative
11/
We'll explore this last element more fully in a future thread on navigating consult conflict.
For now, let's introduce a basic strategy for initiating & calibrating the "pitch".
I always lead w/ some version of “Tell us what your team thinks about…[the case, the dilemma]"
We'll explore this last element more fully in a future thread on navigating consult conflict.
For now, let's introduce a basic strategy for initiating & calibrating the "pitch".
I always lead w/ some version of “Tell us what your team thinks about…[the case, the dilemma]"
12/
This simple question helps set up the “emotional valence” of the recommendations as you deliver them.
Here’s an example from a common encounter between ID and primary teams.
This simple question helps set up the “emotional valence” of the recommendations as you deliver them.
Here’s an example from a common encounter between ID and primary teams.

13/
With experience, recognizing the primary team’s perspective on the consult “ask” becomes easier.
This may be based on:
*⃣ The consult "type" requested
*⃣ The "ask" itself
*⃣ The team/person making the "ask"
*⃣ The interpersonal dynamic when delivering recs
With experience, recognizing the primary team’s perspective on the consult “ask” becomes easier.
This may be based on:
*⃣ The consult "type" requested
*⃣ The "ask" itself
*⃣ The team/person making the "ask"
*⃣ The interpersonal dynamic when delivering recs
14/
This means experienced consultants adjust their communication style intuitively and on-the-fly.
But this may NOT be intuitive to learners on consult teams whose only previous perspective was that OF a primary team.
So how do we teach this?
This means experienced consultants adjust their communication style intuitively and on-the-fly.
But this may NOT be intuitive to learners on consult teams whose only previous perspective was that OF a primary team.
So how do we teach this?
15/
In this figure I've summarized strategies I've found helpful.
Big picture goals:
1⃣ Reinforce communication skills that build trust & cultivate a positive consult culture
2⃣ Develop skills in the “art of persuasion”
3⃣ Empower learners to be the team representative
In this figure I've summarized strategies I've found helpful.
Big picture goals:
1⃣ Reinforce communication skills that build trust & cultivate a positive consult culture
2⃣ Develop skills in the “art of persuasion”
3⃣ Empower learners to be the team representative

16/
A recap.
In this 🧵 we learned:
🌟 Verbal recs are 🗝️ to better teaching/engagement by & w/ consultants
🌟 A “Where is the learner?” framework helps us think through HOW to give verbal recs
🌟 We can build consult communication skills intentionally w/ specific strategies
A recap.
In this 🧵 we learned:
🌟 Verbal recs are 🗝️ to better teaching/engagement by & w/ consultants
🌟 A “Where is the learner?” framework helps us think through HOW to give verbal recs
🌟 We can build consult communication skills intentionally w/ specific strategies

17/
Next week @JenniferSpicer4 will continue this series on “Teaching Consultant Skills,” w/ “Writing Notes.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to keep up with all our threads in one place!
See you next week!
Next week @JenniferSpicer4 will continue this series on “Teaching Consultant Skills,” w/ “Writing Notes.”
Remember to check out #SubspecialtyTeaching @MedEdTwagTeam to keep up with all our threads in one place!
See you next week!

• • •
Missing some Tweet in this thread? You can try to
force a refresh