Second story of today is of a middle aged poor man who was in a nearby big district hospital for 3 days and referred to a big city for treatment.
He came to us hearing we have a good set up and having no money to even travel to Varanasi BHU.
He came to us hearing we have a good set up and having no money to even travel to Varanasi BHU.
He was emaciated and breathing hard 😮💨.
My 🩺 told me has a big pleural effusion and on asking history I was convinced he probably has TB with effusion.
My 🩺 told me has a big pleural effusion and on asking history I was convinced he probably has TB with effusion.
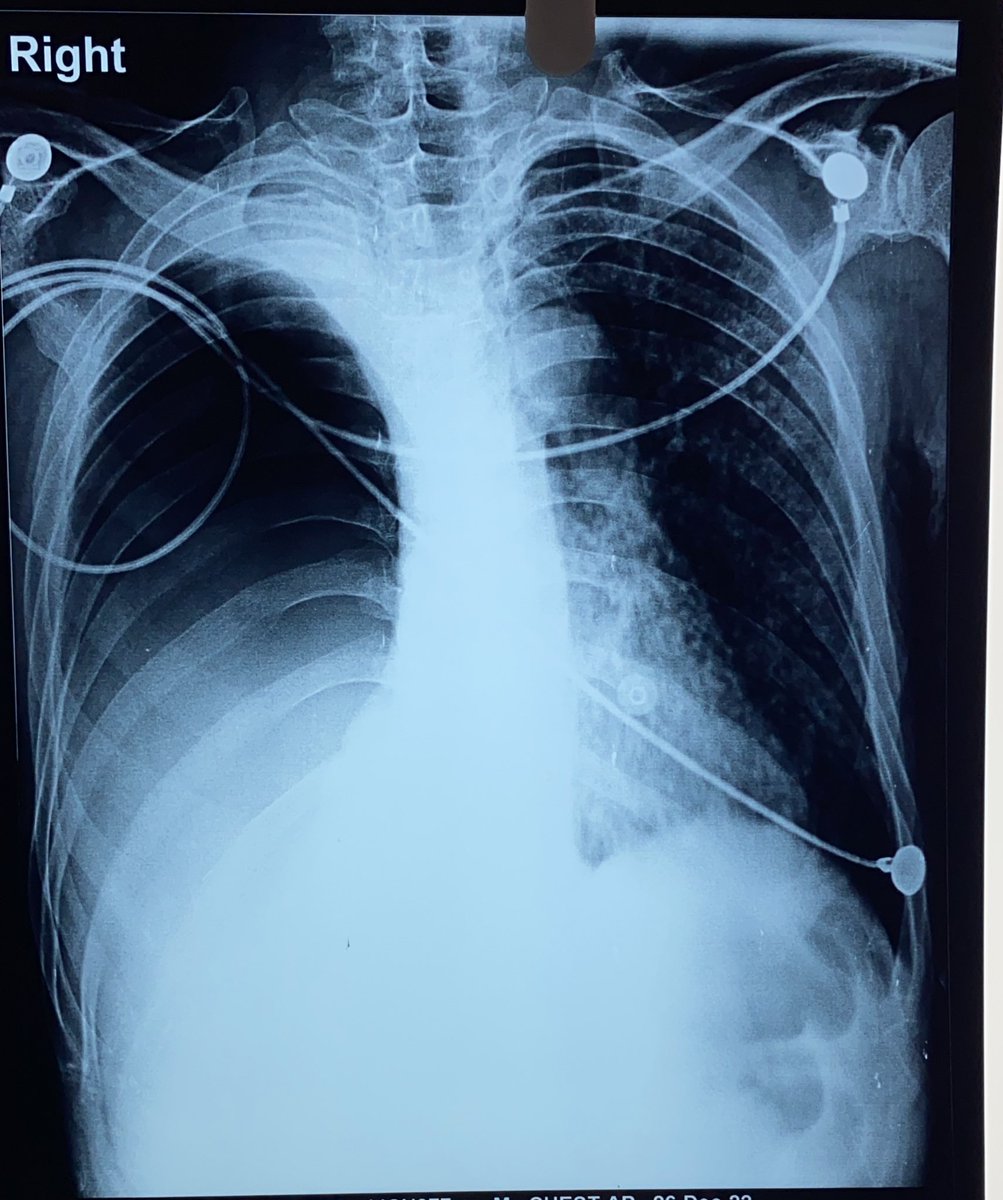
On probing and asking many times is when the poor relatives told me that they were driven away from the govt hospital without any treatment or diagnosis, after doing a 🩻 showing this 
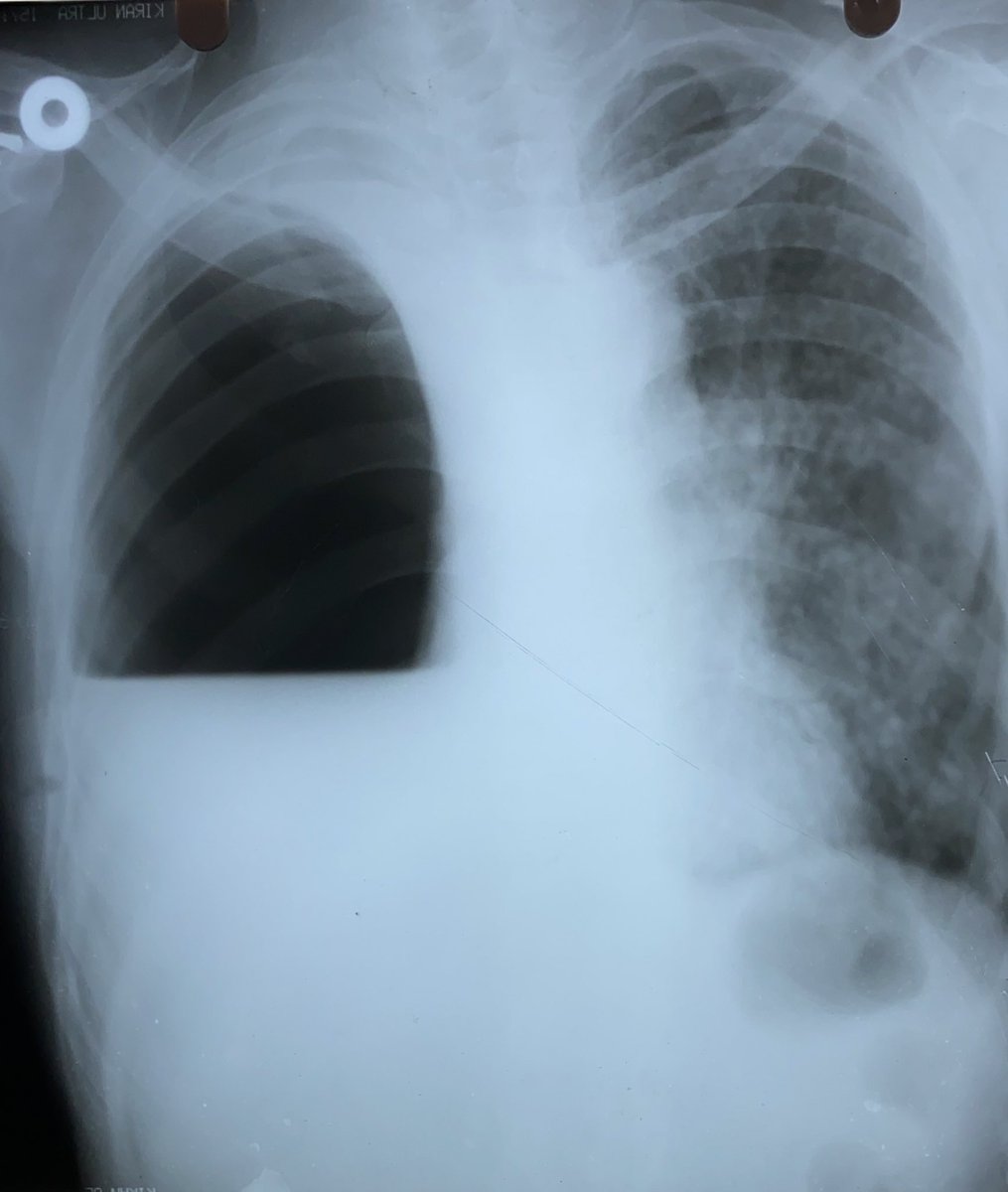
My smart surgeon friend was involved and he promptly put an ICD seeing the hydropneumothorax.
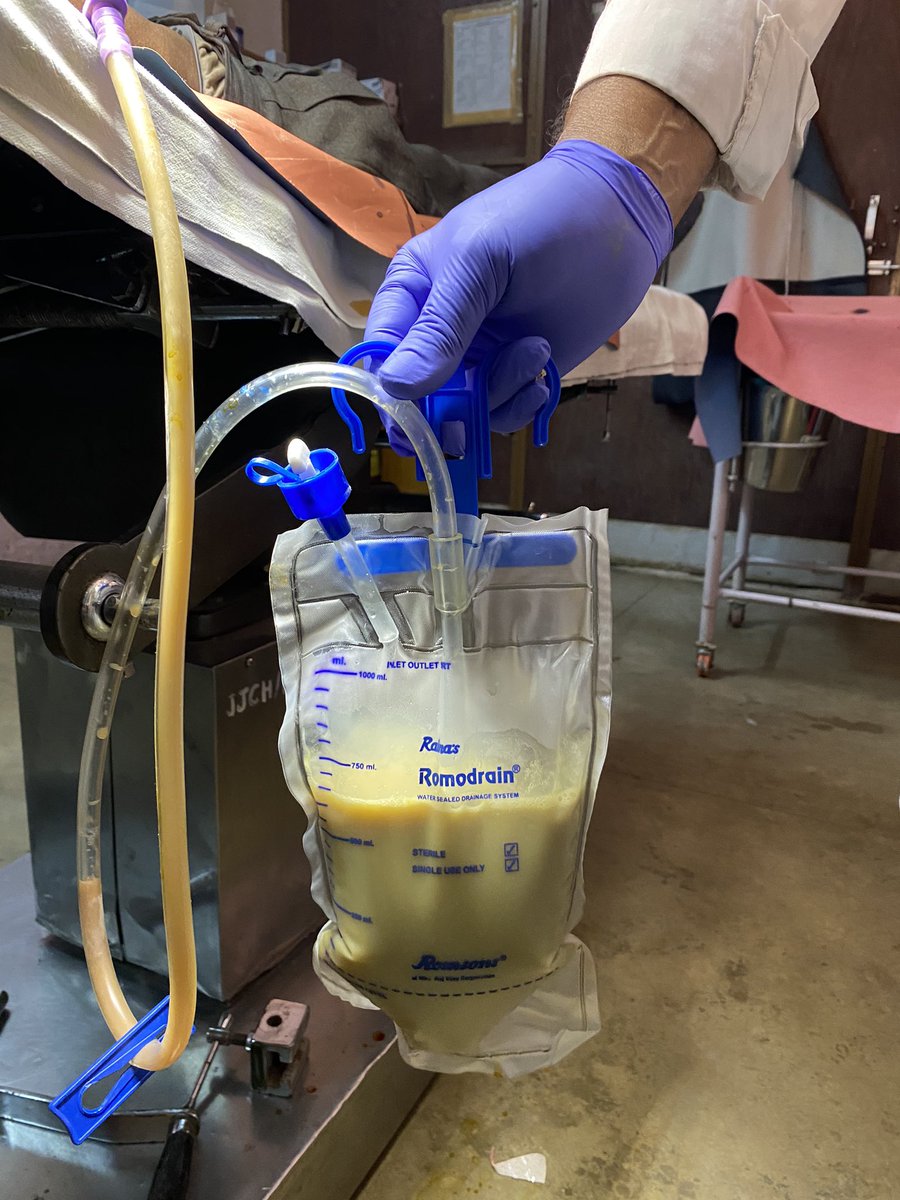
What came out was air, which bubbled under water but after a while when we connected the drain, it was 😲
What came out was air, which bubbled under water but after a while when we connected the drain, it was 😲

We can’t eliminate TB if we don’t take responsibility and do the needful.
It was quite 😔 to witness big govt hospitals shooing away patients with treatable illnesses like TB. ICD was life saving for this poor man and we were able to do the needful thanks to our training & team.
It was quite 😔 to witness big govt hospitals shooing away patients with treatable illnesses like TB. ICD was life saving for this poor man and we were able to do the needful thanks to our training & team.
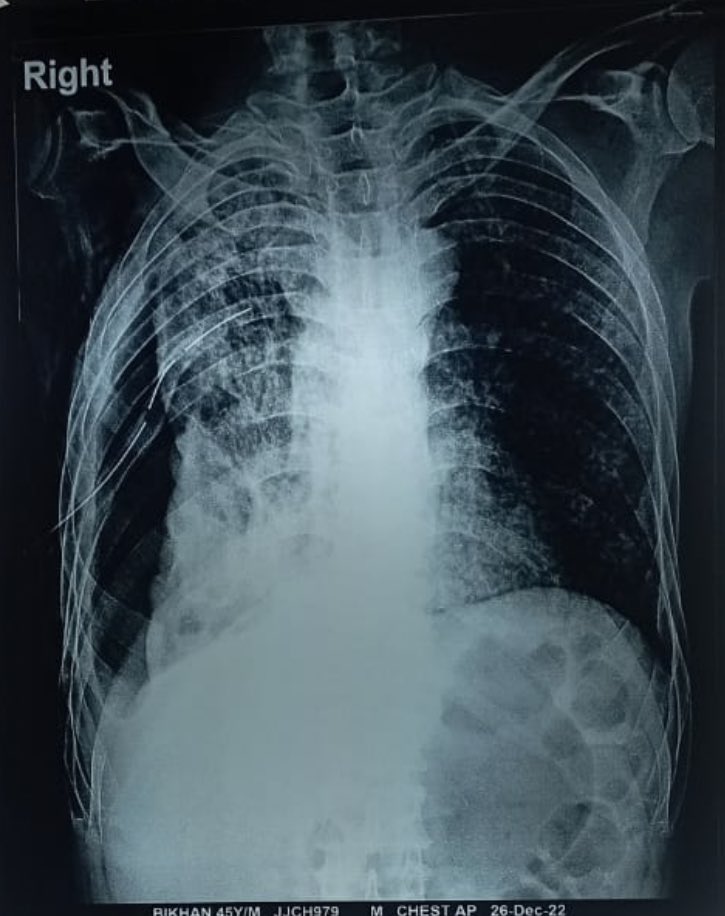
The lung has expanded now post ICD 🤗.
Waiting for sputum AFB tmrw morning to start ATT.
This is quite bad disease and right lung look half fibrosed 🫠
Waiting for sputum AFB tmrw morning to start ATT.
This is quite bad disease and right lung look half fibrosed 🫠
* Final diagnosis: Chronic suppurative lung disease-Right lung Pyo-pneumothorax.
* Probable etiology: Mycobacterium Tuberculosis/Aneeobic bacteria.
* Ix: Sputum and Pus AFB/CBNNAT: negative
HIV: neg
* Rx: Emperical ATT+ Amoxycillin/Clavulonic acid
* Probable etiology: Mycobacterium Tuberculosis/Aneeobic bacteria.
* Ix: Sputum and Pus AFB/CBNNAT: negative
HIV: neg
* Rx: Emperical ATT+ Amoxycillin/Clavulonic acid
Some of u remember this patient story, who had R sided empyema in whom we had started empirical ATT+Amoxycillin-clavulonic acid for MTB and anaerobic cover along with putting an ICD.
He was dischargd after a while for continuation of antibiotics waiting for clinical improvement
He was dischargd after a while for continuation of antibiotics waiting for clinical improvement
This poor man came back all 🤮 and not able to eat with a DILI prob due to the ATT/AmoxyClav we started 😥
His ALT/AST were in 200s and I stopped the meds due to the hepatitis.
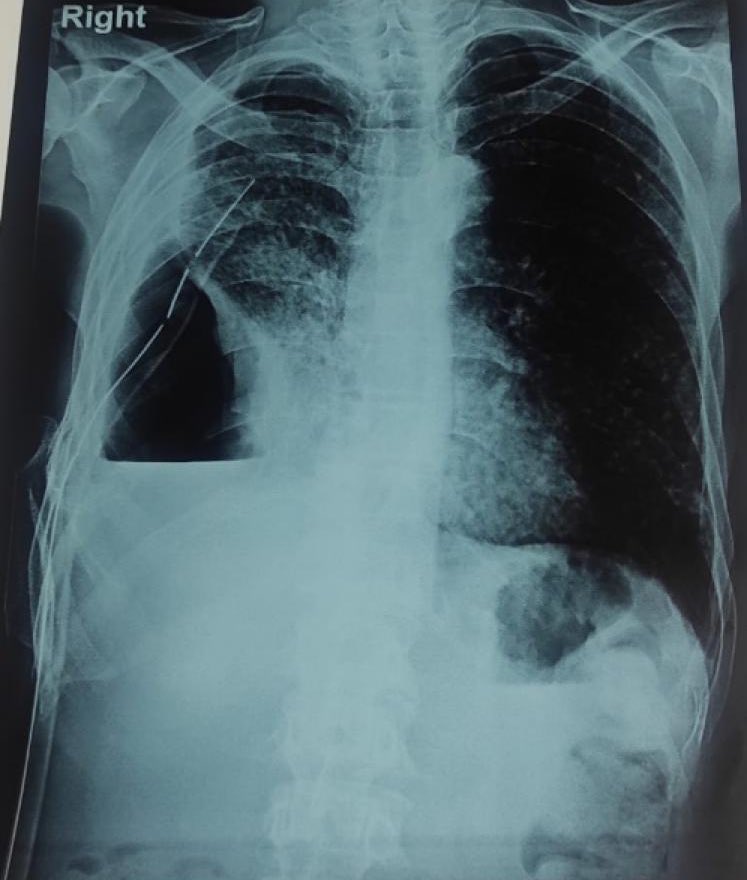
On repeating 🩻 it was even 😞 with poor 🫁 expansion and the drain still showing dark pus🫢
His ALT/AST were in 200s and I stopped the meds due to the hepatitis.
On repeating 🩻 it was even 😞 with poor 🫁 expansion and the drain still showing dark pus🫢
We decided to explore the Dx aggressively 👊(as cultures from the pus couldn’t be sent last time due to resource constraints) this time and my surgeon friend came to the rescue to aspirate pus.
We got good amount of pus and sent to a local pvt lab for bacterial/TB cultures.
We got good amount of pus and sent to a local pvt lab for bacterial/TB cultures.

You can do all the gimmicks u want 🕺with the best intentions by making fantastic efforts 🦾, but without a confirming microbiological dx 🫵🏽 you’re never sure if you’re hitting the right target 🎯
I learned it the hard way 🥴
I learned it the hard way 🥴
We gave him symptomatic Rx for his nausea and dyspepsia + gave an antibiotic break.
He slowly recovered and we waited patiently for the culture 🤞
In the meantime, we learned a lot abt how to improve ICD working to optimise lung expansion and reduce the alveolo-pleural fistula.
He slowly recovered and we waited patiently for the culture 🤞
In the meantime, we learned a lot abt how to improve ICD working to optimise lung expansion and reduce the alveolo-pleural fistula.
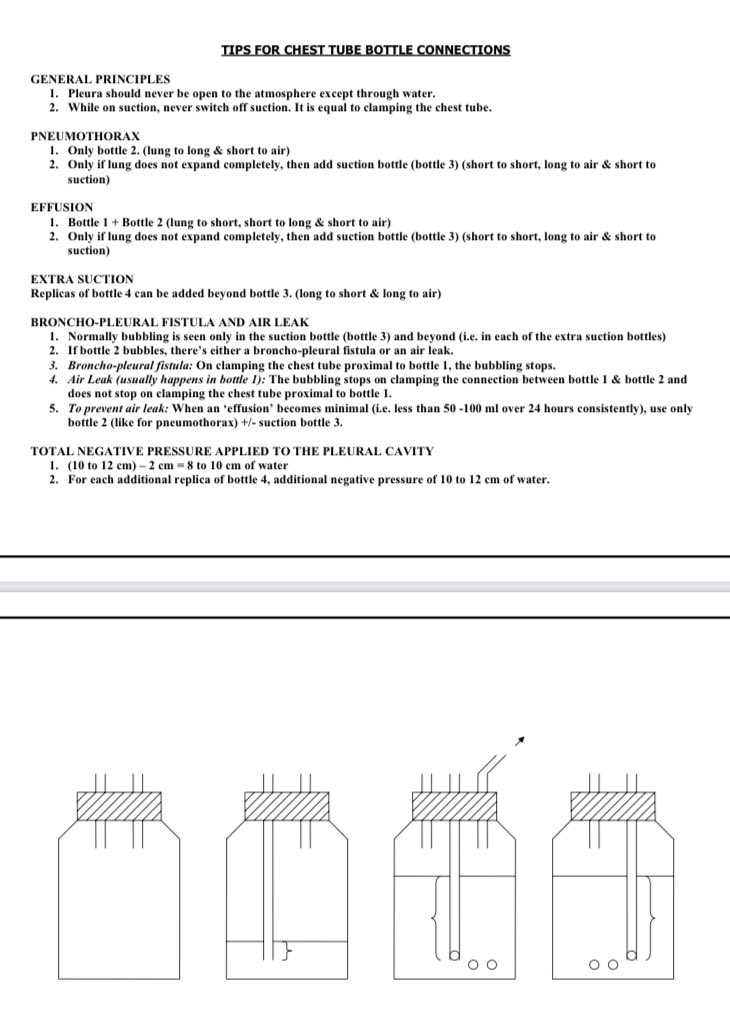
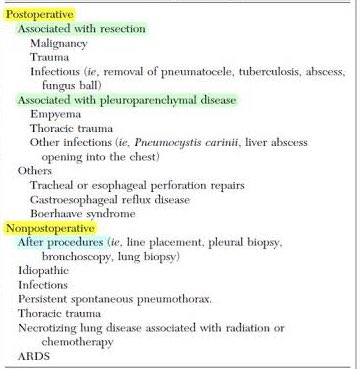
He had developed alveolopleural fistula probably iatrogenically-can occur after thoracentesis or chest tube insertion (ie, pleural drainage procedure) or due to the necrotising lung infection.
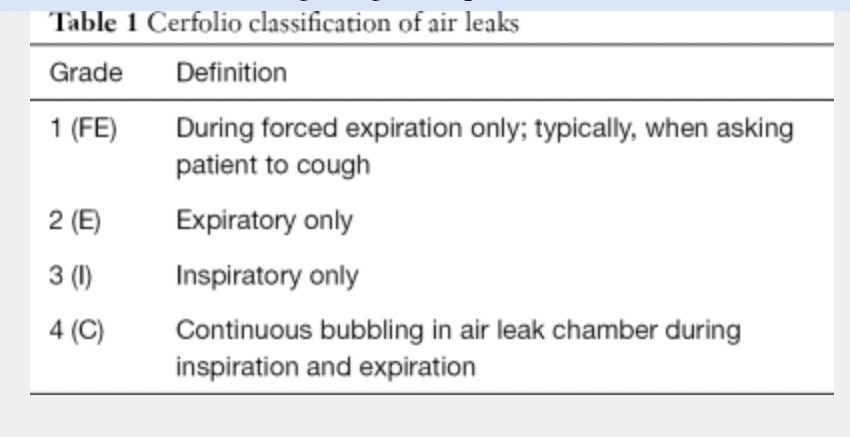
He had bubbling of the fluid in the drain bottle during forced expiration (grade 1)😮💨

He had bubbling of the fluid in the drain bottle during forced expiration (grade 1)😮💨
We also did a crossectional imaging to rule out malignancy or endobronchial lesions and other parenchyma path.
CT ruled out cancer looking lesions but showed miliary pattern in the left 🫁 along with a thick walled R middle lobe cavity with a communication to the pleural space.
CT ruled out cancer looking lesions but showed miliary pattern in the left 🫁 along with a thick walled R middle lobe cavity with a communication to the pleural space.

Military TB can be notoriously sputum negative, as in this case.
But he showed no improvement with ATT and even the pus which is supposed to teem with AFB was negative 3 times on CBNAAT.
If the empyema is due to TB, both sputum and pleural fluid should be CBNAAT ➕
But he showed no improvement with ATT and even the pus which is supposed to teem with AFB was negative 3 times on CBNAAT.
If the empyema is due to TB, both sputum and pleural fluid should be CBNAAT ➕
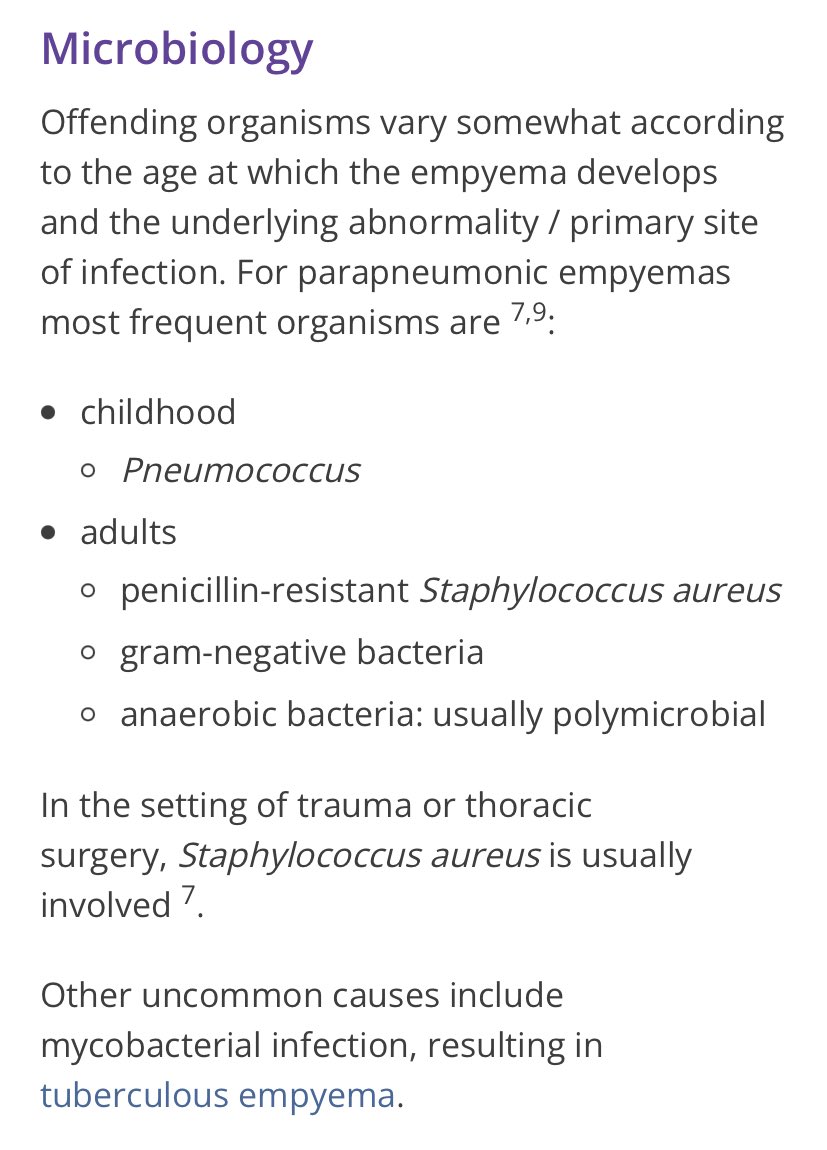
Tuberculous effusions r different from tuberculous empyema
TB empyema is due to a caseous focus in the 🫁 rupturing into the pleural space-via a broncho-pleural fistula
Effusions r due to a hypersensitivity reaction of the pleura
This explains the diff in bacterological yield
TB empyema is due to a caseous focus in the 🫁 rupturing into the pleural space-via a broncho-pleural fistula
Effusions r due to a hypersensitivity reaction of the pleura
This explains the diff in bacterological yield
Air along with pus indicates rupture of subpleural tuberculous caseous focus.
Not only CBNAAT positivity, it will also be AFB positive as the empyema will be teeming with TB bacilli.
pubmed.ncbi.nlm.nih.gov/10197400/#:~:t….
Not only CBNAAT positivity, it will also be AFB positive as the empyema will be teeming with TB bacilli.
pubmed.ncbi.nlm.nih.gov/10197400/#:~:t….
Another 🙇 point:
Whenever you place/manage an ICD, always ensure that it has a vent open (in chest tube bottle system or bag like romodrain) to the atmosphere or connected to suction.
This is particularly important while dealing with a pneumothorax or hydro/pyopneumothorax.
Whenever you place/manage an ICD, always ensure that it has a vent open (in chest tube bottle system or bag like romodrain) to the atmosphere or connected to suction.
This is particularly important while dealing with a pneumothorax or hydro/pyopneumothorax.

While all this was happening, the bacterial culture on the pus came and gave us all a ⚡️🧐
He had grown CRO Klebsiella pneumoniae, yes, the notorious one 🔴
Now I didn’t know how to proceed with such an antibiogram 🤯
I heard of hypervirulent KP in hepatic abscess, but this ⚠️
He had grown CRO Klebsiella pneumoniae, yes, the notorious one 🔴
Now I didn’t know how to proceed with such an antibiogram 🤯
I heard of hypervirulent KP in hepatic abscess, but this ⚠️

On reading up on Empyema after the bacteriological dx, Mr KP showed me it’s real face. This fellow is bad, like killer bad 🚷
Klebsiella Empyema is described as old as 1960s
Klebsiella Empyema is described as old as 1960s
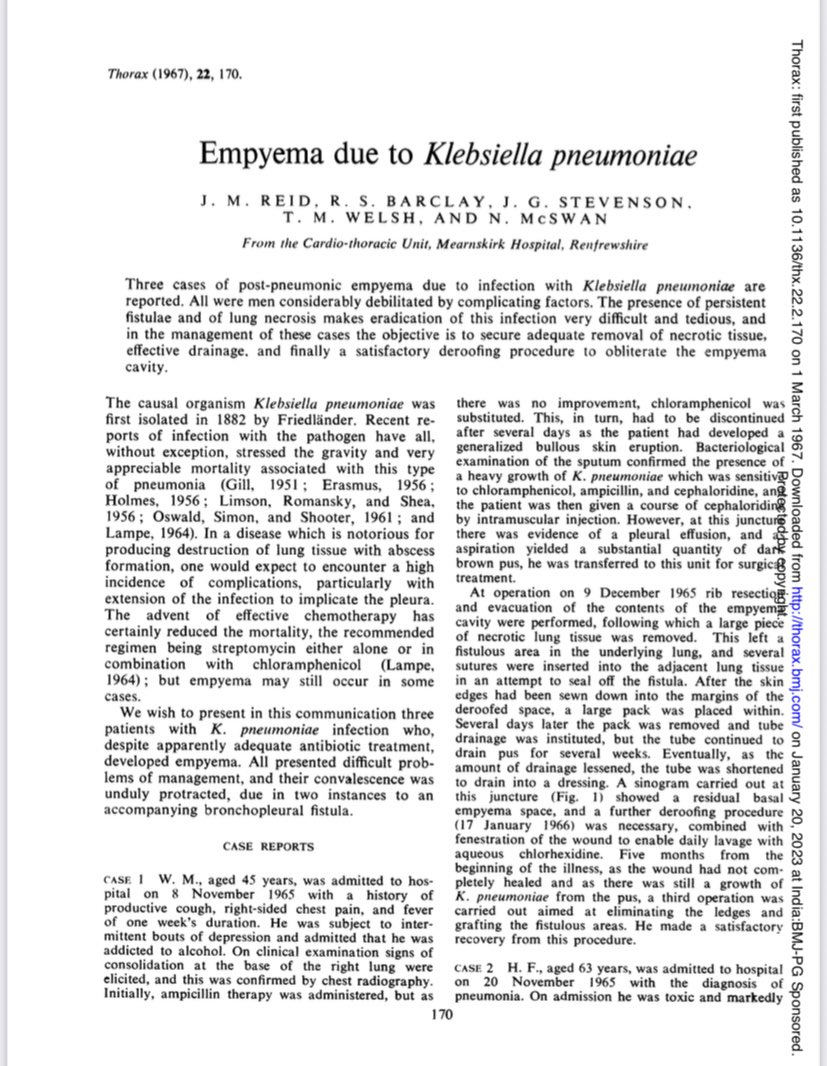
In 👆 case series, all presented with diff probs of management, and their convalescence was unduly protracted, due in two instances to an accompanying BPF.
Though Klebsiella causes a small % of pneumonias, 50% had abscesses and of these 1/3rd developed empyema 🔥
Though Klebsiella causes a small % of pneumonias, 50% had abscesses and of these 1/3rd developed empyema 🔥
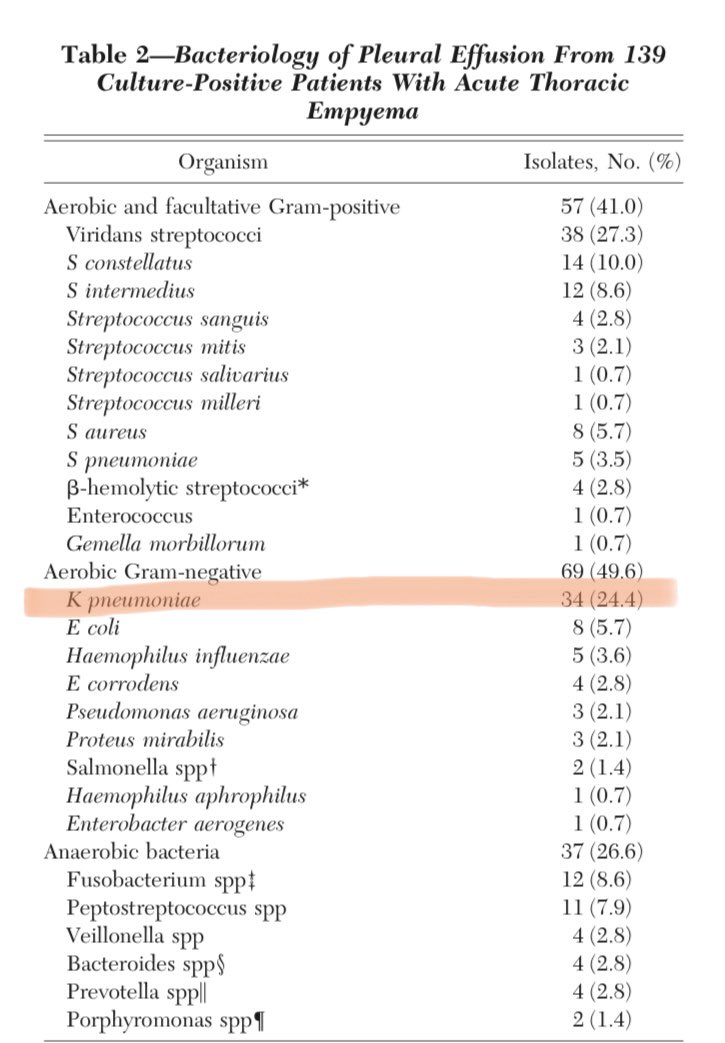
There are also 2 large case series from Taiwan on thoracic empyema from 2 decades and both showed similar findings.
K pneumoniae was the most frequently isolated sole pathogen in this study.
About 44% of the patients with Klebsiella empyema had diabetes mellitus.

K pneumoniae was the most frequently isolated sole pathogen in this study.
About 44% of the patients with Klebsiella empyema had diabetes mellitus.
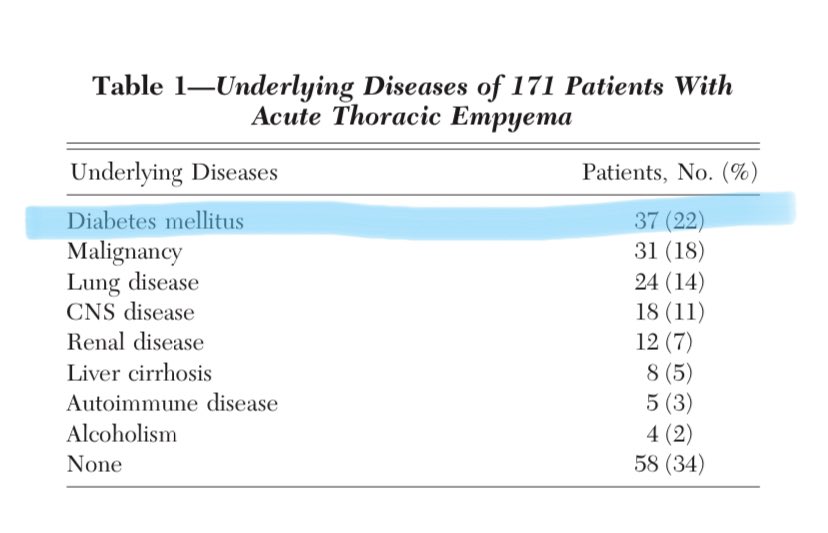
But our pt had no DM/HIV
On 🙇 further, we got the prob reason why he got this tough 🦠
It’s been reported-K.pneumonia and empyema may occur in alcoholic 💁♂️ with multiple host-defense defects that impair the containment of or the perception of disease until it is well-advanced.
On 🙇 further, we got the prob reason why he got this tough 🦠
It’s been reported-K.pneumonia and empyema may occur in alcoholic 💁♂️ with multiple host-defense defects that impair the containment of or the perception of disease until it is well-advanced.
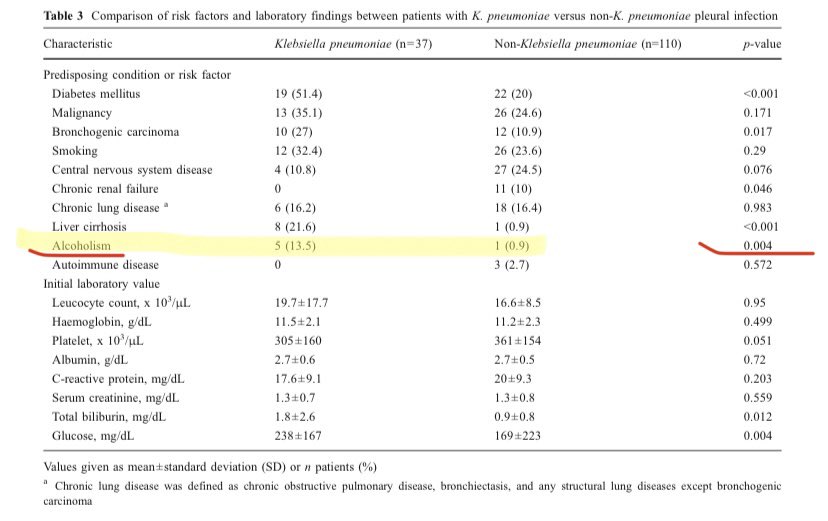
Our patient was a daily consumer of alcohol🍾
He worked hard and drank local toddy 🍶
Here’s ⬇️ another sad story of a local toddy abuser.
He worked hard and drank local toddy 🍶
Here’s ⬇️ another sad story of a local toddy abuser.
https://twitter.com/dawnkuruvilla04/status/1612492187815784448
There’s no time to dwell in the past or feel hopeless at the bad situation 😩, it’s time for action and work 🏋️ towards healing.
The story may not have a great ending but the battles need to be fought 🤺as the enemy lines have been now delineated.
The story may not have a great ending but the battles need to be fought 🤺as the enemy lines have been now delineated.
Now to the plan on management and the road ahead for planning treatment.
When I consulted my professor in CMC Vellore with this patient and the 🦠 causing such a bad empyema, his straight answer was-“He needs a thoracotomy”
Now that’s a big 🔪
When I consulted my professor in CMC Vellore with this patient and the 🦠 causing such a bad empyema, his straight answer was-“He needs a thoracotomy”
Now that’s a big 🔪
Antibiotics alone unlikely to benefit.
⏫️ Resistance + inadequate source control ⏸️
As we are planning antibiotic therapy and surgery, I welcome comments and inputs from #IDtwitter #MedTwitter
⏫️ Resistance + inadequate source control ⏸️
As we are planning antibiotic therapy and surgery, I welcome comments and inputs from #IDtwitter #MedTwitter
@threadreaderapp unroll pls
• • •
Missing some Tweet in this thread? You can try to
force a refresh