Had the opportunity to be part of a fascinating work. Americas Poison Center Annual report.
A comprehensive poisoning epidemiology study compiled of data from all 55 U.S. Poison Centers
Free 🔗➡️bit.ly/3wbIwWS
Pubmed🔗➡️bit.ly/3wdgeLP
A🧵on emerging trends
A comprehensive poisoning epidemiology study compiled of data from all 55 U.S. Poison Centers
Free 🔗➡️bit.ly/3wbIwWS
Pubmed🔗➡️bit.ly/3wdgeLP
A🧵on emerging trends
This year we highlighted two important trends in addition to baseline poisoning data.
Firstly, THC product exposures have been increasing since 2016, and the demographics are changing. In 2021, edible products (red line) eclipsed plant based marijuana (blue line) for products
Firstly, THC product exposures have been increasing since 2016, and the demographics are changing. In 2021, edible products (red line) eclipsed plant based marijuana (blue line) for products

The change in products also represents changing demographics. While Adults (gold) comprise the majority of exposures, pediatric<6 (green) is taking an ever increasing share of the THC exposure calls since 2016. 

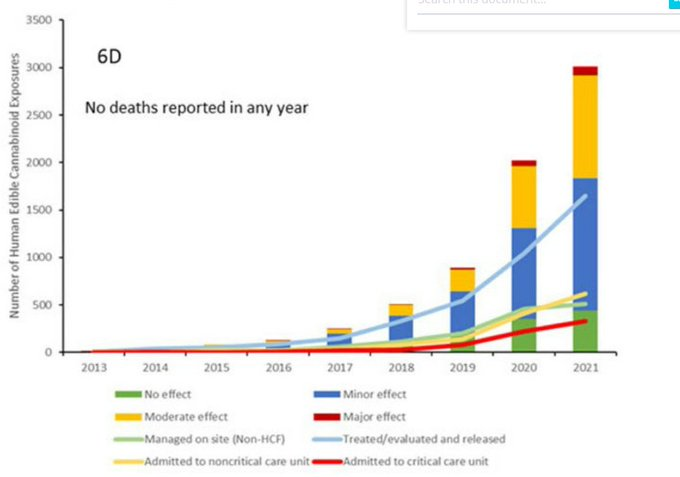
With increasing exposures largely due to an increase in pediatric edible exposures, we see more of all clinical outcomes, minor symptoms, as well as moderate and major clinical effects. 

For those unfamiliar with poison center coding.
“Minor effects”=symptoms w/ no disability (skin irritation, drowsiness, GI symptoms).
“Moderate effects” = more pronounced (e.g.,
disorientation, tachycardia).
“Major effects” = life-threatening or result in disability (i.e., sz)
“Minor effects”=symptoms w/ no disability (skin irritation, drowsiness, GI symptoms).
“Moderate effects” = more pronounced (e.g.,
disorientation, tachycardia).
“Major effects” = life-threatening or result in disability (i.e., sz)
As you would imagine, with increased medical effects occurring we are also seeing increased healthcare utilization and cost.
Evaluation at a hospital for exposure (light blue line), admission to ICUs (red line) and acute care admission (yellow line) are also increasing.
Evaluation at a hospital for exposure (light blue line), admission to ICUs (red line) and acute care admission (yellow line) are also increasing.
This data is the very same data used in the recent publication on pediatric cannabis exposure and is just another example of how poison center data can be utilized to monitor trends.
publications.aap.org/pediatrics/art…
What other trends can we see?
publications.aap.org/pediatrics/art…
What other trends can we see?
The next concerning trend to talk about is bupropion (dark blue line), quickly out pacing all other antidepressants for antidepressant with most severe adverse effects in OD (seizure, arrhythmia, cardiac arrest etc...). 

While bupropion has the highest prevalence, the attack rate of major effects is still higher with TCA and lithium PER overdose.
The overall high prevalence of severe effects with bupropion is likely due to the sheer quantity of overdoses we now see each year.
The overall high prevalence of severe effects with bupropion is likely due to the sheer quantity of overdoses we now see each year.
In summary
1. THC exposures & healthcare utilization ⬆️ annually, largely d/t pediatric edible exposure
2. Serious effects from Bupropion OD continue to ⬆️, likely d/t ⬆️exposure overall
3. Poison Center data is invaluable in monitoring emerging trends in poisoning and OD
#MedED
1. THC exposures & healthcare utilization ⬆️ annually, largely d/t pediatric edible exposure
2. Serious effects from Bupropion OD continue to ⬆️, likely d/t ⬆️exposure overall
3. Poison Center data is invaluable in monitoring emerging trends in poisoning and OD
#MedED
If you found this data useful, please RT the tweet below to help share trends in poisoning and overdose from the free annual report of Americas Poison Centers.
#MedEd #FOAMed #Toxtweets #Toxthursday #MedTwitter #Twitterx #EMRx #Medicine #Poison #Toxic
#MedEd #FOAMed #Toxtweets #Toxthursday #MedTwitter #Twitterx #EMRx #Medicine #Poison #Toxic
https://twitter.com/EMPoisonPharmD/status/1615426527499325475?s=20&t=vJxzlkdiYmG0bUAUe1ztTQ
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh










