DERMATOMYOSITIS (DM)
Let’s spend some time in this #tweetorial on the dermatologic manifestations of this potentially paraneoplastic disease!
First, a question: What is necessary to make a diagnosis of DM?
1/
Let’s spend some time in this #tweetorial on the dermatologic manifestations of this potentially paraneoplastic disease!
First, a question: What is necessary to make a diagnosis of DM?
1/
None of the above! DM is a clinical diagnosis, which is why getting the exam right is super important! That said a biopsy CAN help with getting to a diagnosis, but it’s not necessary.
So let’s start! Heliotrope rash! This poikilodermatous erythema occurs around the eyes.
2/
So let’s start! Heliotrope rash! This poikilodermatous erythema occurs around the eyes.
2/

Remember though that exams are different across skin tone. Heliotrope can look a lot more subtle in someone with more melanated skin. That rash can also include the rest of the face!
3/
3/

Shawl sign (back) and V sign (upper chest) is another one we all learn in medical school. What’s the deal with all these physical exam findings?
Well, they are all in photodistributed patterns. Additionally, they are generally poikilodermatous!
4/

Well, they are all in photodistributed patterns. Additionally, they are generally poikilodermatous!
4/


Poikilodermatous? Say what? It’s just a fancy way we refer to skin that has 4 changes: Hyperpigmentation, hypopigmentation, erythema, and atrophy. The point is heliotrope, shawl sign, v-sign, other findings, are usually all similarly “poikilodermatous” changes in the skin.
5/
5/
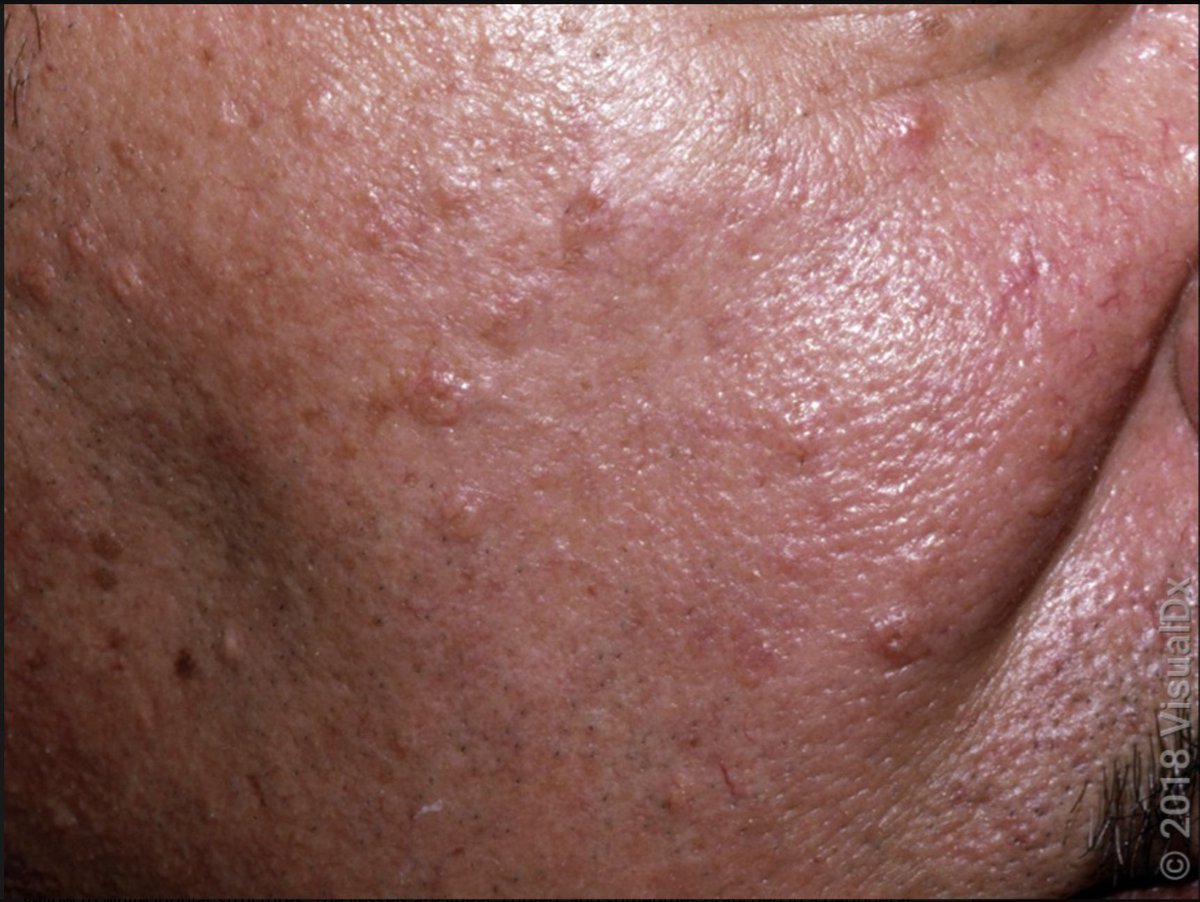
All right, what else did you learn about DM? I’m guessing…. Gottron! These are now called Atrophic dermal papules of DM (ADPDM). Importantly, even if you don’t have papules and just have the erythema, that’s still c/w DM!
6/

6/


Since we’re on the hands, let’s zoom in on the fingers & look for the other telltale signs you’re looking for. Specifically, the ragged cuticles and dilated periungual capillary loops! Notice how those blood vessels are plump & super noticeable compared to your own (I hope!).
7/

7/


This is where most people stop thinking about skin findings. But did you know there are more? You can see calcinosis cutis in DM (not just in systemic sclerosis!). It’s much more common in Juvenile DM, but adults can get it too.
8/
8/

DM can also present with flagellate erythema! Check out my other brief thread on this. 4 things classically cause this:
DM
Bleomycin
Shiitake mushrooms
Still’s Disease
9/
DM
Bleomycin
Shiitake mushrooms
Still’s Disease
https://twitter.com/DrStevenTChen/status/1558087072644091905?s=20&t=GB96Vni4q4-MaUf6fe7jMg
9/
And you can also get that poikilodermatous change on your lateral thighs. This is called holster sign (pic 1)! You can also get keratodermatous changes to your hands called “mechanic’s hands (pic 2).
10/

10/


Not only are these exam findings important for the diagnosis of DM, but also because different findings can be associated with different risk. Mechanic’s hands + holster sign make me concerned for anti-synthetase syndrome!
Which Autoantibody is linked with this?
11/
Which Autoantibody is linked with this?
11/
Jo-1 Is associated with anti-synthetase syndrome.
TIF-1 and NXP-2 are associated with increased risk of malignancy!
OMG-7 is just silly.
12/
TIF-1 and NXP-2 are associated with increased risk of malignancy!
OMG-7 is just silly.
12/
While we’re on the topic, let’s discuss malignancy risk. It’s been reported in up to 40% of ADULT patients with DM (not really a concern in juvenile DM). Most commonly reported associations are ovarian, lung, colon, breast, GI, and lymphoma.
13/
13/
Given these concerns, what is the work up for a new DM patient in regards to malignancy? I was taught the following:
Age-appropriate cancer screening
Transvaginal US + CA-125 (if applicable)
CT Scan Neck to pelvis
Check out the whole list👇:
Source: acrabstracts.org/abstract/cance…
14/
Age-appropriate cancer screening
Transvaginal US + CA-125 (if applicable)
CT Scan Neck to pelvis
Check out the whole list👇:
Source: acrabstracts.org/abstract/cance…
14/

Although a topic of debate, the risk of malignancy goes back to baseline after 3-5 years, so I was trained to do the aforementioned periodically until that point.
What about autoantibodies? Here’s a list of what I check and why!
15/
What about autoantibodies? Here’s a list of what I check and why!
15/

The proximal mm weakness I’ll leave to #rheumtwitter to discuss, but this is where I’m testing muscle strength in derm clinic. Remember to ask about washing hair and standing from a seated position ;)
Can you get DM without muscle weakness?
16/
Can you get DM without muscle weakness?
16/
You can! If you have all the skin findings, but NO muscle involvement on exam, labs, nor imaging, you might have something called Clinically amyopathic dermatomyositis (CADM).
This is presumptive for 6 months, after which if all is still negative, it's confirmed CADM!
17/
This is presumptive for 6 months, after which if all is still negative, it's confirmed CADM!
17/
This #tweetorial is getting much too long, so we’ll leave treatment to the next time. Before we get to the summary, a huge thank you to @DrScottElman for giving me feedback! A huge thanks to @visualdx for the photos. And I hope #rheumtwitter will add as they see fit!
18/
18/
SUMMARY
✅DM is a clinical diagnosis. Biopsy can help but not necessary.
✅The consistent findings on exam are poikiloderma and photodistribution.
✅Screening for cancer should happen!
✅You can get DM without muscle involvement!
19/19
✅DM is a clinical diagnosis. Biopsy can help but not necessary.
✅The consistent findings on exam are poikiloderma and photodistribution.
✅Screening for cancer should happen!
✅You can get DM without muscle involvement!
19/19
• • •
Missing some Tweet in this thread? You can try to
force a refresh