A thread on mechanics, logistics and reasons behind positive end expiratory pressure (PEEP) significance while handling patients on mechanical or non-invasive ventilation 🧵
#MedTwitter #EDTweeter #PulmTwitter @PulmPEEPs
#MedTwitter #EDTweeter #PulmTwitter @PulmPEEPs
PEEP is the air pressure that stays “WITHIN” the lungs after a person finishes exhaling. Now, this PEEP pressure is always greater than atmospheric pressure. It essentially prevents the alveoli’s to collapse and maintains the airways open.
CPAP is a non-invasive mode of ventilation which works by the same principal of PEEP, I.e. to provide end expiratory positive pressure
EPAP means expiratory positive airway pressure which works with the same logic & dynamics of PEEP, but is used for patients receiving BPAP
EPAP means expiratory positive airway pressure which works with the same logic & dynamics of PEEP, but is used for patients receiving BPAP

So, why PEEP is so popular while discussing ventilation ?
Two big reasons to consider ⬇️
Two big reasons to consider ⬇️
1. PEEP can be either, “therapeutic” when provided as extrinsic PEEP, via ventilation as seen in ARDS, COPD, atelectasis, pneumonia , etc.
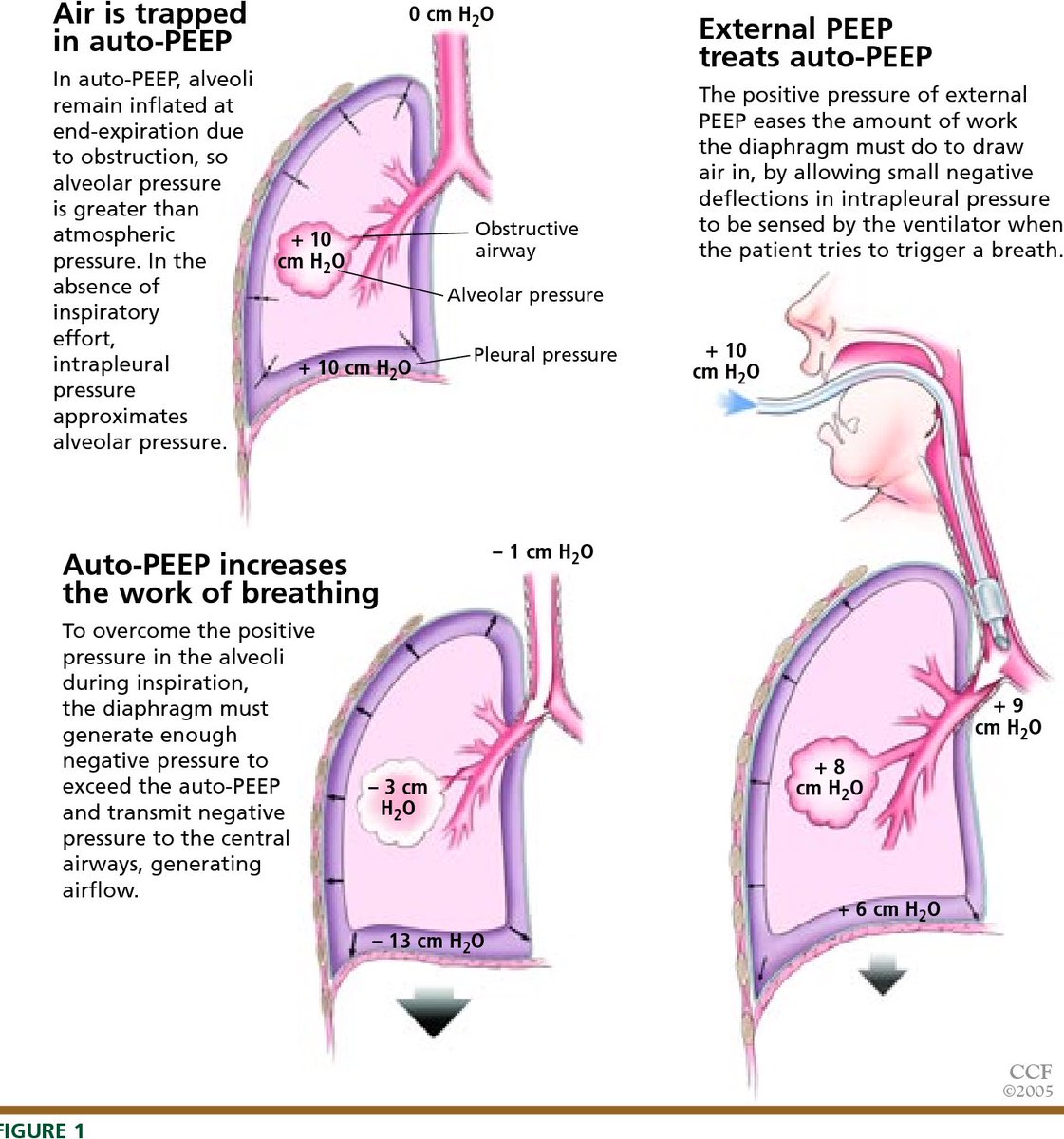
or instead, it can be “a resulting complication” of intrinsic air trapping due to over ventilation also known as “Auto-PEEP”
And …
or instead, it can be “a resulting complication” of intrinsic air trapping due to over ventilation also known as “Auto-PEEP”
And …
…
2. It can be very helpful to improve oxygenation. For reference, Henry’s law states that : high expiratory pressure means high O2 diffusion and improved pO2/SpO2.
2. It can be very helpful to improve oxygenation. For reference, Henry’s law states that : high expiratory pressure means high O2 diffusion and improved pO2/SpO2.
POSITIVES of PEEP
1. Extrinsic PEEP improves V/Q mismatch and keeps it close to one. It does this by “splinting open” the collapsed alveoli’s to better facilitate air exchange in disorders like COPD, ARDS and other pulmonary inflammations. ⬇️
1. Extrinsic PEEP improves V/Q mismatch and keeps it close to one. It does this by “splinting open” the collapsed alveoli’s to better facilitate air exchange in disorders like COPD, ARDS and other pulmonary inflammations. ⬇️
2. Extrinsic PEEP may help decrease the work of breathing and decrease lactate and CO2, improving overall wellbeing of pts. ⬇️
3. Extrinsic PEEP in case of COPD (emphysema) where the core pathology is collapsing alveoli’s upon expiration, PEEP helps keep the alveoli’s open to allow for the trapped air to escape. ⬇️
4. In patients with cariogenic shock (pulmonary edema) might benefit by decreasing preload.
Wait but how does PEEP decrease preload ?
Let us understand further in the next tweet ⬇️😃
Wait but how does PEEP decrease preload ?
Let us understand further in the next tweet ⬇️😃
Our “respiratory drive” originates when the diaphragm contracts and creates (-) intrapulmonary & intra-thoracic pressure, to suck in more air from the atmosphere but at the same time, it sucks in more blood too from the inferior vena cava into the Rt atrium of heart.
Cont…
Cont…
… When you increase PEEP, this increases the intra-thoracic pressure and decreases the filling of right heart, resulting in decreased preload (potentially beneficial in Pulmonary edema).
But what can go wrong with this ?
But what can go wrong with this ?
If the PEEP remains high and preload remains low, patients with “Distributive Shock” could decompensate, as they lack an ability to increase SVR !!
(Hence, one of the situations where PEEP is to be cautiously administered is distributive shock)
#CriticalCare #MedEd
(Hence, one of the situations where PEEP is to be cautiously administered is distributive shock)
#CriticalCare #MedEd

Complications of PEEP !
1. Barotrauma due to inadvertently high plateau and peak pressures in “stiff lung” lung pathologies (ARDS, pneumonia, Fibrosis etc) — More on plateau pressure and peak pressure later
cont…
#MedStudentTwitter
1. Barotrauma due to inadvertently high plateau and peak pressures in “stiff lung” lung pathologies (ARDS, pneumonia, Fibrosis etc) — More on plateau pressure and peak pressure later
cont…
#MedStudentTwitter

…
2. Interference with accurate hemodynamic measurements in patients with Rt heart catheters in place
👉🏻 General rule to avoid barotrauma : Keep the plateau pressure < 30 cm H2O & while going up or down the PEEP values always check mean arterial pressure (MAP)
2. Interference with accurate hemodynamic measurements in patients with Rt heart catheters in place
👉🏻 General rule to avoid barotrauma : Keep the plateau pressure < 30 cm H2O & while going up or down the PEEP values always check mean arterial pressure (MAP)

So what are plateau pressure and peak pressure ?
Plateau pressure - the pressure that remains in the lungs after full inspiratory hold
Peak pressure - the pressure provided against the resistance of airways and alveoli
So what’s crazy about them ? ⬇️
Plateau pressure - the pressure that remains in the lungs after full inspiratory hold
Peak pressure - the pressure provided against the resistance of airways and alveoli
So what’s crazy about them ? ⬇️

Elevations in plateau pressure means “compliance issue” (the lungs are stiff/not willing to expand like in ARDS) while elevations in peak pressure means “increased airway resistance” 

To end our discussion I want to shed some light on “Auto-PEEP”
There are two types of Auto-PEEP as described in sequential tweets ⬇️
There are two types of Auto-PEEP as described in sequential tweets ⬇️
1. Dynamic hyperinflation WITH intrinsic expiratory flow obstruction — COPD or mucus plugs in air inflammation and creates air trapping and (+) auto-PEEP. Little bot of extrinsic PEEP actually proves beneficial as discussed above.
2. Dynamic hyperinflation WITHOUT intrinsic expiratory flow obstruction — essentially when not enough time is given for removing air accumulated in last respiration i.e. to say increased RR and TV —> extrinsic PEEP in such case is prone to barotrauma
Signs of auto-PEEP :
1. Failure of the volume curve to go back to 0, when next resp. cycle begins (volume curve = shown on ventilator monitor)
2. Increase in plateau pressure
3. Increased work of breathing (accessory muscle use), prolonged expiratory time
4. Hypotension
1. Failure of the volume curve to go back to 0, when next resp. cycle begins (volume curve = shown on ventilator monitor)
2. Increase in plateau pressure
3. Increased work of breathing (accessory muscle use), prolonged expiratory time
4. Hypotension

It is said that, for mechanically ventilated patients, those who develop respiratory distress and are found to have volume curve that doesn’t go back to zero before the next resp. cycle, it is highly suggestive of (+) AUTO-PEEP !!
Manage AUTO-PEEP by decreasing RR and TV
Manage AUTO-PEEP by decreasing RR and TV
• • •
Missing some Tweet in this thread? You can try to
force a refresh