1/Does trying to remember inferior frontal gyrus anatomy leave you speechless?
Do you get a Broca’s aphasia trying to name the parts?
Here’s a #tweetorial to help you remember the #anatomy of this important region
#medtwitter #meded #neurotwitter #neurorad #radtwitter #radres
Do you get a Broca’s aphasia trying to name the parts?
Here’s a #tweetorial to help you remember the #anatomy of this important region
#medtwitter #meded #neurotwitter #neurorad #radtwitter #radres

2/Anatomy of the inferior frontal gyrus (IFG) is best seen on the sagittal images, where it looks like the McDonald’s arches.
To find the IFG on MR, I open the sagittal images & scroll until I see the arches. When it comes to this method of finding the IFG, "i’m lovin it."
To find the IFG on MR, I open the sagittal images & scroll until I see the arches. When it comes to this method of finding the IFG, "i’m lovin it."

3/Inferior frontal gyrus also looks like a sideways 3 on sagittal images, if you prefer.
This 3 is helpful bc the inferior frontal gyrus has 3 parts—or "pars"
This 3 is helpful bc the inferior frontal gyrus has 3 parts—or "pars"

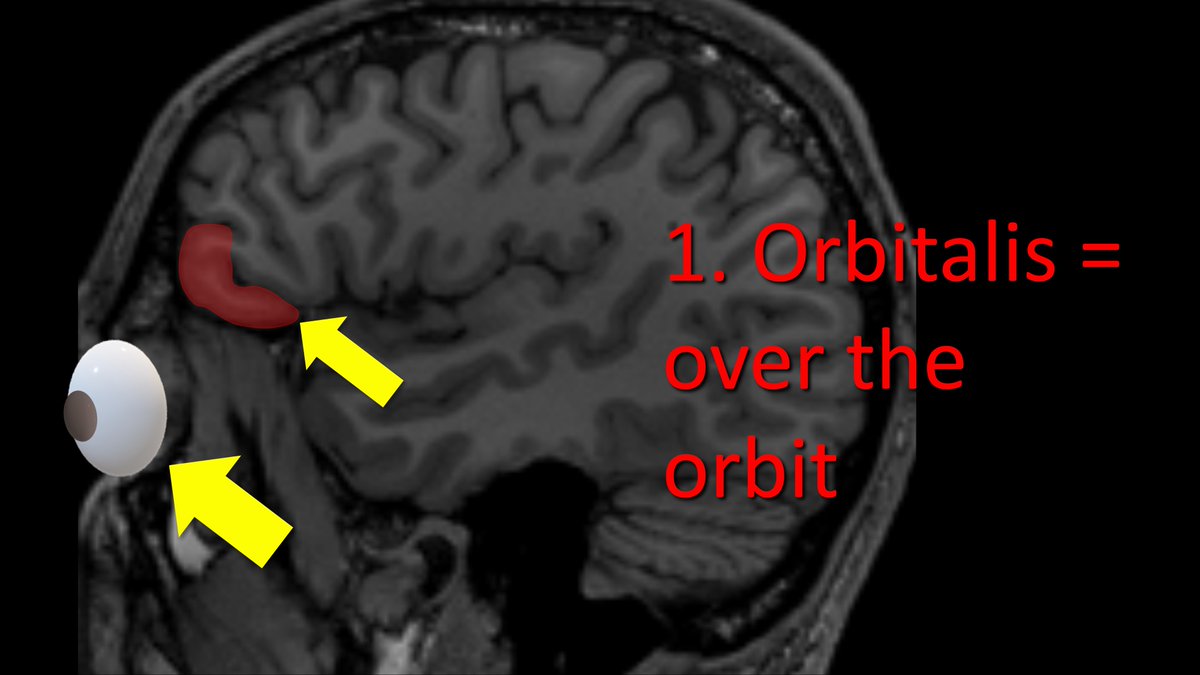
4/Starting anteriorly, the first part is the pars orbitalis. This name is easy to remember bc the pars orbitalis is right next to…wait for it…the orbit.
Orbits are in the front & so the pars orbitalis is at the front of the inferior frontal gyrus
Orbits are in the front & so the pars orbitalis is at the front of the inferior frontal gyrus
5/Behind the pars orbitalis is the pars triangularis—another great name.
This region is shaped like an upside down triangle—so it is easy to remember its name is triangularis
This region is shaped like an upside down triangle—so it is easy to remember its name is triangularis

6/Finally is the pars opercularis. This one is a bit harder to remember.
It is called the pars opercularis bc it forms part of the frontal operculum.
Frankly, I think the name sounds the genus & species of a type of possum. But operculum has nothing to do w/possums
It is called the pars opercularis bc it forms part of the frontal operculum.
Frankly, I think the name sounds the genus & species of a type of possum. But operculum has nothing to do w/possums

7/So where does the word operculum come from?
Operculum is Latin for lid.
“Oper” is from same derivative for “over” & “cover” & “aperture.”
It gets it name bc the pars opercularis forms the "cover" or lid over the insula
Operculum is Latin for lid.
“Oper” is from same derivative for “over” & “cover” & “aperture.”
It gets it name bc the pars opercularis forms the "cover" or lid over the insula

8/Operculum comes from the same derivative as “over”—so I like to call the pars opercularis the “pars overlayeris” instead
This helps me to remember that it overlays the insula, like a blanket or cover.
This helps me to remember that it overlays the insula, like a blanket or cover.

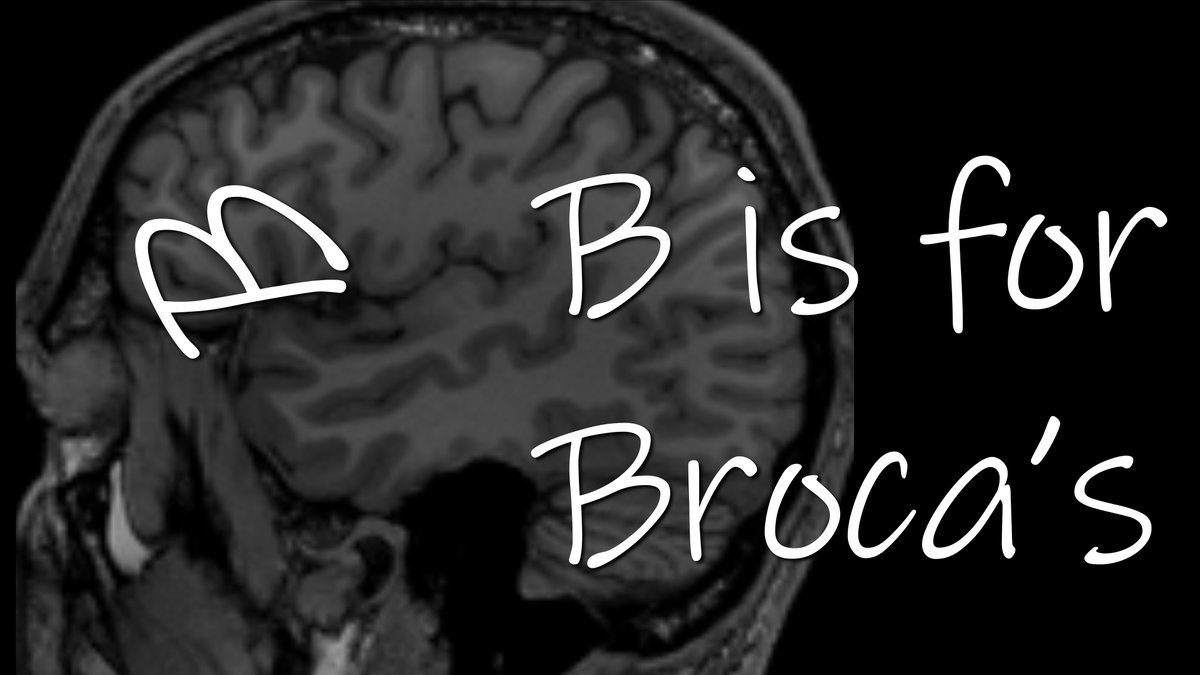
9/IFG is home to Broca’s area, responsible for language fluency. Damage to Broca’s causes an expressive aphasia or difficulty producing speech
If you draw a line through the sylvian fissure underneath the IFG, this line turns the sideways 3 into a sideways B, & B is for Broca
If you draw a line through the sylvian fissure underneath the IFG, this line turns the sideways 3 into a sideways B, & B is for Broca
10/So where is Broca’s in the inferior frontal gyrus?
Well, that is controversial & depends on who you ask.
But the most common localization is between the pars triangularis & pars opercularis
Well, that is controversial & depends on who you ask.
But the most common localization is between the pars triangularis & pars opercularis

11/You can remember that bc Brocas is between the "triangle" pars & the "cover" pars.
Just remember:
If you only use triangles as a cover, you will leave people speechless (or with a Broca’s aphasia!)
Just remember:
If you only use triangles as a cover, you will leave people speechless (or with a Broca’s aphasia!)

12/On axials, Broca’s area is more difficult to find bc you don’t have a McDonalds sign or triangle to look for, like on sagittals
My rule of thumb is:
If the frontal horns of the lateral ventricles look like eyes, Broca’s is sort of like Princess Leia buns on either side
My rule of thumb is:
If the frontal horns of the lateral ventricles look like eyes, Broca’s is sort of like Princess Leia buns on either side

13/So now you know the anatomy of the inferior frontal gyrus, its parts, & its relation to Broca’s area.
Hopefully, now when you are asked about this region, you can speak about it fluently!
Hopefully, now when you are asked about this region, you can speak about it fluently!

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















