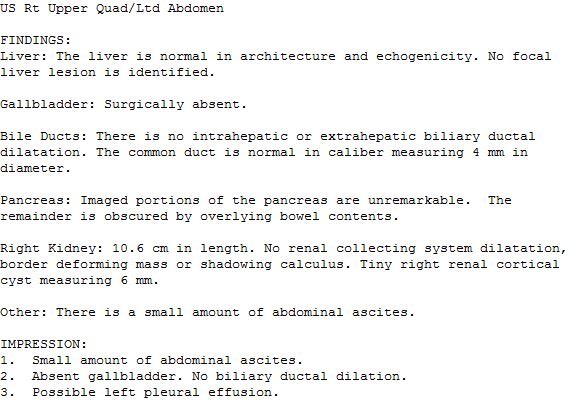
ICU stories (a brief one): 60 yo male w lung cancer / CAD / HTN / HLD / status post chemotherapy a month ago presented to the ED w SOB/cough/weakness after failing outpatient tx w azithromycin. CT chest: no PE but positive for bilateral consolidations:
Patient came to the ICU intubated, sedated, on pressors & antibiotics for PNA. Next step: POCUS. PLAX looked "weird", so Doppler and "zoomed" views were recorded:
PSAX & subcostal views:
4-chamber views:
IVC:
What was this 👆incidental finding (?) in the IVC?
This was an IVC filter. Returning to the POCUS (skipping the lung & VEXUS parts of it): it showed significant thickening of the tips of both the anterior and posterior MV leaflets. A TEE was performed two days later:
It confirmed thickening of the tips of both the anterior and posterior MV leaflets w mobile echodensities consistent w vegetations. There was a MR jet central to posteriorly directed w flow reversal in the pulmonary veins (not shown here).
What did the blood cultures grow?
Blood culures (and the rest of the ID workup) remained negative. Most likely scenario: patient had non-bacterial thrombotic endocarditis (also known as marantic or Libman-Sachs)
Take-home messages:
1. According to Hickam's dictum: "patients can have as many diseases as they damn well please". Interestingly, this aphorism was stated many years before POCUS became common practice! Sadly, I have not myself searched for the origin of this principle.
1. According to Hickam's dictum: "patients can have as many diseases as they damn well please". Interestingly, this aphorism was stated many years before POCUS became common practice! Sadly, I have not myself searched for the origin of this principle.
It is attributed to John Hickam, Chair of the Department of Medicine at the University of Indiana. According to the legend, Hickam was housestaff in the Department of Medicine at Grady Memorial Hospital in Atlanta. Knowing Grady Hospital quite well, I have little doubt that
the principle was borne there...
2. Nonbacterial thrombotic endocarditis (NBTE) is most frequently associated with neoplasia but also w SLE, RA, antiphospholipid syndrome, multiple myeloma, Crohn’s disease etc & of course, w COVID-19. Systemic embolization is
2. Nonbacterial thrombotic endocarditis (NBTE) is most frequently associated with neoplasia but also w SLE, RA, antiphospholipid syndrome, multiple myeloma, Crohn’s disease etc & of course, w COVID-19. Systemic embolization is
the most common clinical manifestation. NBTE vegetations are most frequently L-sided, w 2/3 involving the MV & the remainder the AoV. It cannot be distinguished from infectious endocarditis w imaging alone. Even w anticoagulation, its prognosis is unfavorable due to the
association with the primary condition, such as advanced cancer
Thanks for reading!
#POCUS #ECHOFIRST #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedTwitter #MedEd #EMBound @RJonesSonoEM @NephroP @MynephCC @ICUltrasonica @TaotePOCUS @cianmcdermott @cjosephy @KalagaraHari @MegriMohammed @icmteaching @curromir #MedStudentTwitter
#POCUS #ECHOFIRST #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedTwitter #MedEd #EMBound @RJonesSonoEM @NephroP @MynephCC @ICUltrasonica @TaotePOCUS @cianmcdermott @cjosephy @KalagaraHari @MegriMohammed @icmteaching @curromir #MedStudentTwitter
• • •
Missing some Tweet in this thread? You can try to
force a refresh