Teaming up again with the great @VerwerftJan to share our experience with #echoCPET in #HFpEF. This hot-of-the-press paper @ESC_Journals demonstrates myriad of opportunities for diagnosis & treatment, far beyond #SGLT2i only. Tweetorial below!
@SarahStroobant2 @HerbotsLieven
@SarahStroobant2 @HerbotsLieven

We have recently described our set-up for a dedicated #dyspnoeaclinic in detail @JACCJournals
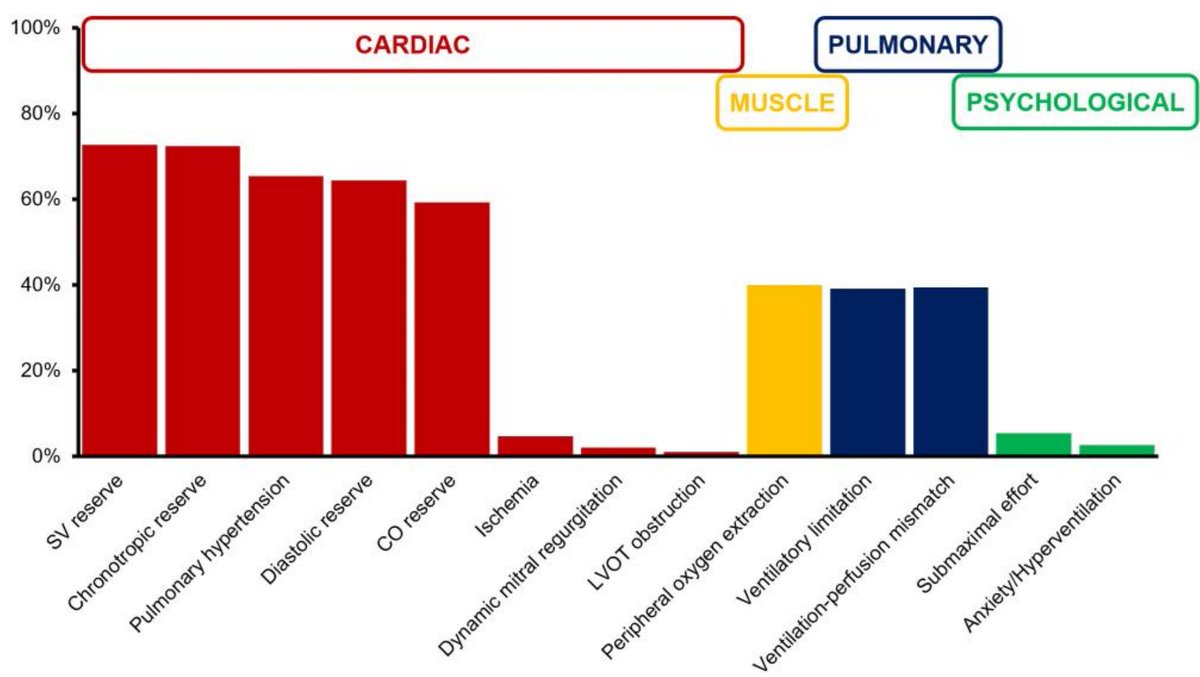
In #HFpEF, early & correct diagnosis are important, #phenotyping is everything. There are a lot of mechanisms for dyspnoea involved
https://twitter.com/FH_Verbrugge/status/1622711913909026828
In #HFpEF, early & correct diagnosis are important, #phenotyping is everything. There are a lot of mechanisms for dyspnoea involved
Current @ESC_Journals paper goes one step further: "In patients with confirmed HFpEF or probability >90% according to well-validated HFpEF scores (both are complimentary in our view), why #echoCPET within a dedicated #dyspnoea clinic? What is the impact of findings?" 

1. Further diagnostic work-up !
#HFpEF has a lot of mimickers that deserve to be ruled out, in 9/10 patients we searched further for causes of dyspnoea, on average 2 diagnostic exams per patient!
#cardiomyopathy #amyloid #CAD #lungdisease
#HFpEF has a lot of mimickers that deserve to be ruled out, in 9/10 patients we searched further for causes of dyspnoea, on average 2 diagnostic exams per patient!
#cardiomyopathy #amyloid #CAD #lungdisease

2. Medical treatment changes !
In virtually all patients, one can optimize therapies... We change on average 3 meds!
#SGLT2i & #spironolactone are obvious ones, but #hypertension & #lipids should be within targets!
Also, I single out reducing/stopping #betablockers, done in ~60%!
In virtually all patients, one can optimize therapies... We change on average 3 meds!
#SGLT2i & #spironolactone are obvious ones, but #hypertension & #lipids should be within targets!
Also, I single out reducing/stopping #betablockers, done in ~60%!

3. Tackle comorbidities in 1 stop !
- Obesity is a treatable disease nowadays: #GLP1agonists, sometimes surgery
- Iron deficiency present in 40% (need more data in #HFpEF for R/, but we do often do provide IV iron)
- Too many patients w #diabetes to leave only to endocrinologists
- Obesity is a treatable disease nowadays: #GLP1agonists, sometimes surgery
- Iron deficiency present in 40% (need more data in #HFpEF for R/, but we do often do provide IV iron)
- Too many patients w #diabetes to leave only to endocrinologists
"Don't blame the patient for not caring for themselves, blame yourself for not taking the action that is necessary"
Pro-active = making a difference together
Pro-active = making a difference together
4. Cardiac interventions !
So much easier to stop betablockers in #HFpEF after #AFib ablation. However, first get the meds right and #decongest proberly, more success!
In selected patients pacing & valvular interventions are useful, but ONLY AFTER getting the other things right!
So much easier to stop betablockers in #HFpEF after #AFib ablation. However, first get the meds right and #decongest proberly, more success!
In selected patients pacing & valvular interventions are useful, but ONLY AFTER getting the other things right!

Do You have a dyspnoea clinic for #HFpEF at your place?
• • •
Missing some Tweet in this thread? You can try to
force a refresh