One of the most important diagnostic tests in Cardiology to interpret is the EKG.
Here are my thoughts and notes. Will continue to this thread. Let me know what you think!
Thread #10: Fascicular Blocks
#arjuncardiology #medtwitter #CardioTwitter #MedEd #IMG
Here are my thoughts and notes. Will continue to this thread. Let me know what you think!
Thread #10: Fascicular Blocks
#arjuncardiology #medtwitter #CardioTwitter #MedEd #IMG
Fascicular Blocks:
- Left bundle branch system: sub-divided into an anterior & posterior fascicle.
- Hemi-block does not widen the QRS complex markedly (compared to a RBBB or LBBB)
- Left bundle branch system: sub-divided into an anterior & posterior fascicle.
- Hemi-block does not widen the QRS complex markedly (compared to a RBBB or LBBB)
Left Anterior Fascicular Block (LAFB):
- Diagnosed by finding of a left axis deviation (-45 degrees or more negative)
- Delayed activation of more superior & leftward position of the LV
- Isolated finding is non-specific; can be seen w/ HTN, AV disease, CAD, and aging
- Diagnosed by finding of a left axis deviation (-45 degrees or more negative)
- Delayed activation of more superior & leftward position of the LV
- Isolated finding is non-specific; can be seen w/ HTN, AV disease, CAD, and aging

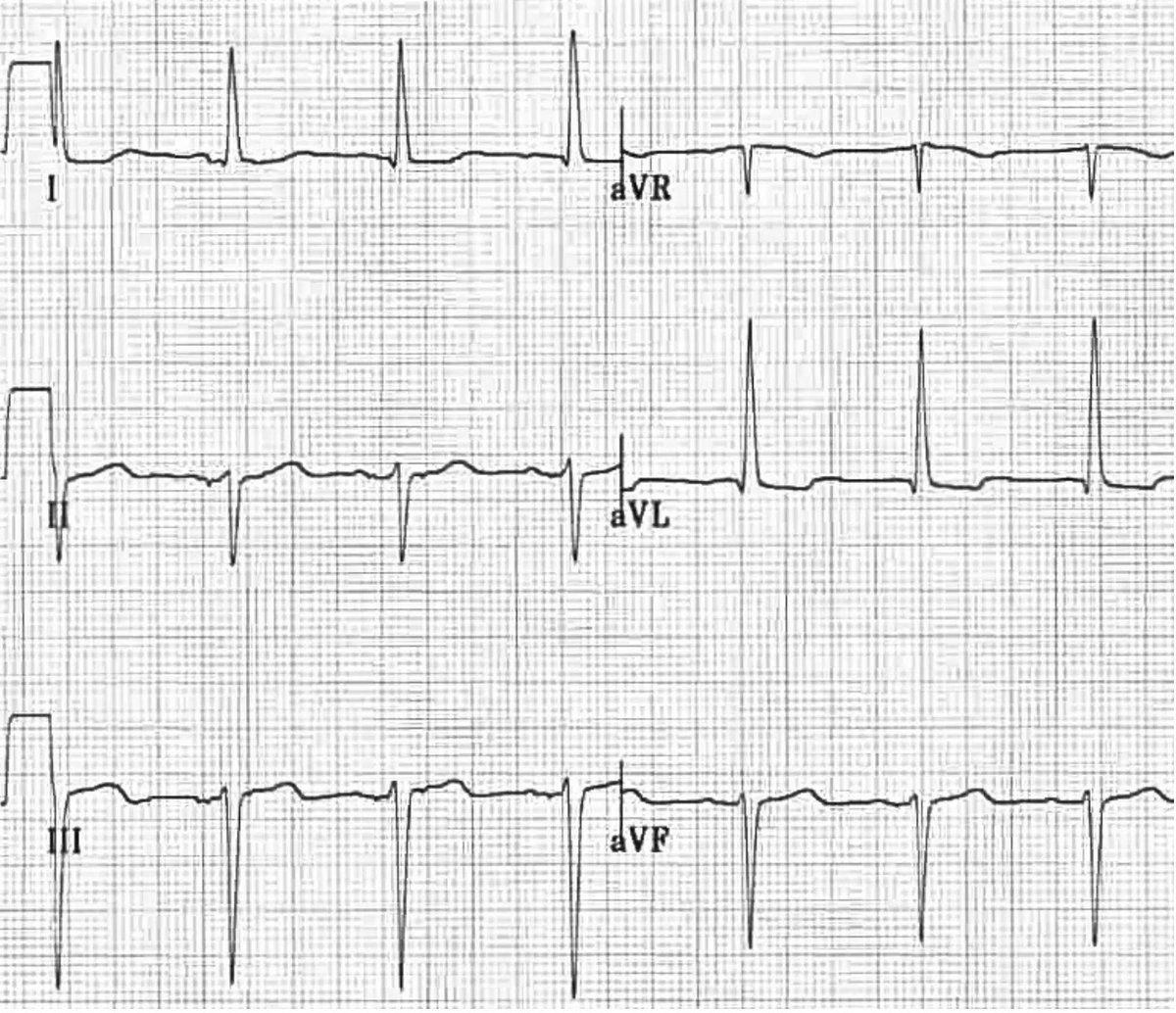
LAFB ECG:
- rS complexes in lead II, III, avF, and small R waves and deep S waves
- qR complexes in leads I, aVL, with small Q waves and tall R waves
- (+) deflection in I & avL and (-) deflection in II, III, aVF
- rS complexes in lead II, III, avF, and small R waves and deep S waves
- qR complexes in leads I, aVL, with small Q waves and tall R waves
- (+) deflection in I & avL and (-) deflection in II, III, aVF
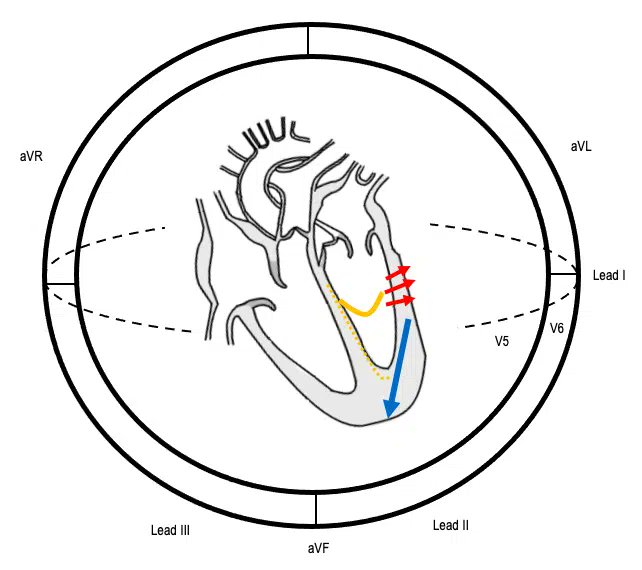
Left Posterior Fascicular Block (LPFB):
- Right axis deviation (+ 120 degrees or more positive)
- Delayed activation of more inferior & rightward portion of LV
- Diagnosis of exclusion for right-axis deviation (other more common: RVH, emphysema, lateral wall infarction, PE)
- Right axis deviation (+ 120 degrees or more positive)
- Delayed activation of more inferior & rightward portion of LV
- Diagnosis of exclusion for right-axis deviation (other more common: RVH, emphysema, lateral wall infarction, PE)
LPFB ECG:
- rS complexes in leads I and avL, with small R waves and deep S waves
- qR complexes in leads II, III, avF with small Q waves and tall R waves
- Right axis deviation: (+) in II, III, aVF and (-) in I & aVL
- rS complexes in leads I and avL, with small R waves and deep S waves
- qR complexes in leads II, III, avF with small Q waves and tall R waves
- Right axis deviation: (+) in II, III, aVF and (-) in I & aVL

Bi-fascicular Block
- Block in any of 2/3 fascicles
- RBBB + LAFB = RBBB with left-axis deviation
- RBBB + LPFB = RBBB with right-axis deviation
- Development of a new bi-fascicular block (usually RBBB with LAFB) during acute anterior MI may be warning for complete heart block
- Block in any of 2/3 fascicles
- RBBB + LAFB = RBBB with left-axis deviation
- RBBB + LPFB = RBBB with right-axis deviation
- Development of a new bi-fascicular block (usually RBBB with LAFB) during acute anterior MI may be warning for complete heart block

Tri-fascicular Block
- With 1:1 AV conduction is rarely present on ECG
- Patients can present with alternating LBBB & RBBB. In these patients, a permanent pacemaker is indicated because of high risk for abrupt complete heart block.
- Image: RBBB + LAFB + 3rd degree
- With 1:1 AV conduction is rarely present on ECG
- Patients can present with alternating LBBB & RBBB. In these patients, a permanent pacemaker is indicated because of high risk for abrupt complete heart block.
- Image: RBBB + LAFB + 3rd degree

Thanks to this amazing site for the graphics! Stay tuned for the next threads on myocardial ischemia!
litfl.com/left-anterior-…
litfl.com/left-posterior…
litfl.com/bifascicular-b…
litfl.com/trifascicular-…
litfl.com/left-anterior-…
litfl.com/left-posterior…
litfl.com/bifascicular-b…
litfl.com/trifascicular-…
• • •
Missing some Tweet in this thread? You can try to
force a refresh