One of the most important diagnostic tests in Cardiology to interpret is the EKG.
Here are my thoughts and notes. Will continue to this thread. Let me know what you think!
Thread #11: Myocardial Ischemia
#arjuncardiology #medtwitter #CardioTwitter #MedEd #IMG
Here are my thoughts and notes. Will continue to this thread. Let me know what you think!
Thread #11: Myocardial Ischemia
#arjuncardiology #medtwitter #CardioTwitter #MedEd #IMG
Myocardial Ischemia:
- One of the most important things to evaluate on EKG
- If severe narrowing/complete blockage of a coronary artery causes blood flow to become adequate, ischemia of the heart muscle develops
- Can be transient (angina pectoris) or more severe (necrosis & MI)
- One of the most important things to evaluate on EKG
- If severe narrowing/complete blockage of a coronary artery causes blood flow to become adequate, ischemia of the heart muscle develops
- Can be transient (angina pectoris) or more severe (necrosis & MI)

Myocardial Ischemia
- LV consists of an outer layer (epicardium/sub-epicardium) and inner layer (sub-endocardium)
- Can have limit of ischemia to the inner layer or can affect the entire thickness of the ventricular wall (transmural ischemia)
- LV consists of an outer layer (epicardium/sub-epicardium) and inner layer (sub-endocardium)
- Can have limit of ischemia to the inner layer or can affect the entire thickness of the ventricular wall (transmural ischemia)

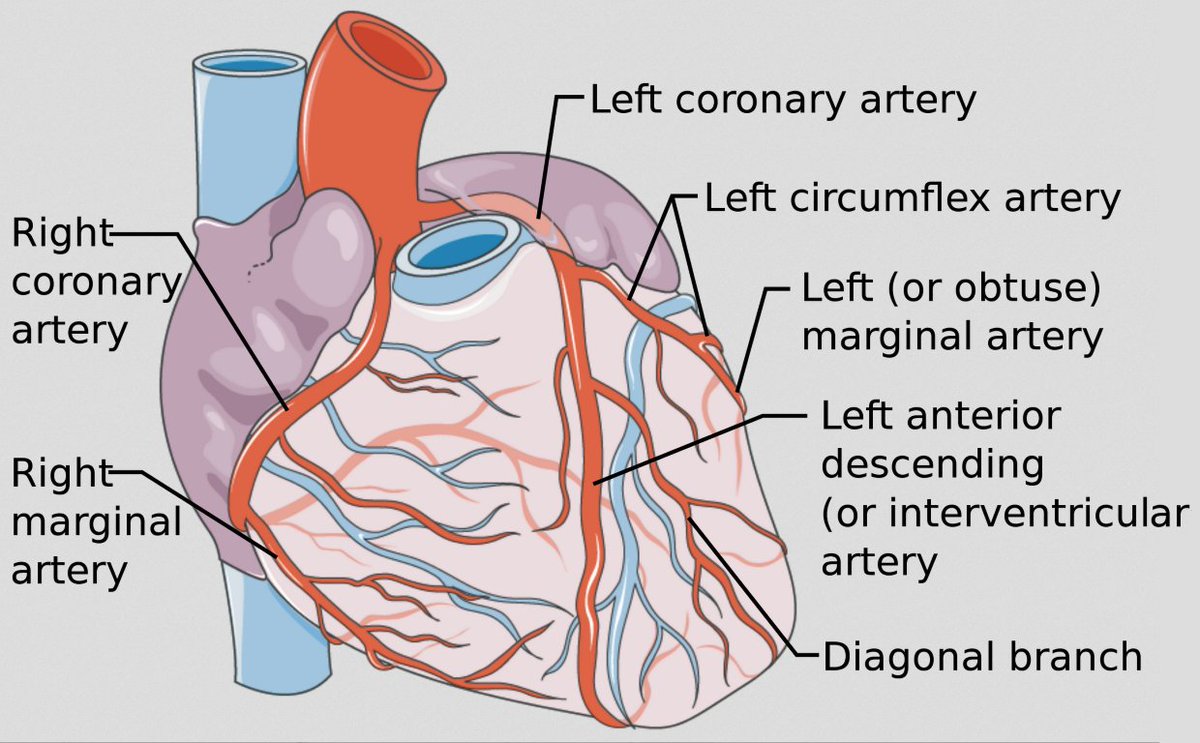
Myocardial Blood Supply
- RCA supplies both inferior (diaphragmatic) portion of the heart and RV
- Left main divides into the left anterior descending artery (LAD), which supplies the ventricular septum and large part of free LV wall, and LCx (lateral wall of the LV)
- RCA supplies both inferior (diaphragmatic) portion of the heart and RV
- Left main divides into the left anterior descending artery (LAD), which supplies the ventricular septum and large part of free LV wall, and LCx (lateral wall of the LV)
ST Elevation/Transmural Ischemia
- Ischemia & ultimately necrosis of a portion of the LV free wall
- Most patients w/ acute MI have underlying atherosclerotic disease
- Occlusion of coronary artery with a ruptured plaque leads to coagulation cascade (fibrin & platelets)
- Ischemia & ultimately necrosis of a portion of the LV free wall
- Most patients w/ acute MI have underlying atherosclerotic disease
- Occlusion of coronary artery with a ruptured plaque leads to coagulation cascade (fibrin & platelets)

ST Elevation/Transmural Ischemia
- Other factors for acute STEMI: cocaine, coronary artery dissection, coronary artery emboli
- Acute phase: ST elevations, hyper-acute T-waves in multiple leads
- Evolving phase: Hours/days later with deep T-wave inversions replacing ST elevation
- Other factors for acute STEMI: cocaine, coronary artery dissection, coronary artery emboli
- Acute phase: ST elevations, hyper-acute T-waves in multiple leads
- Evolving phase: Hours/days later with deep T-wave inversions replacing ST elevation

ST Elevation/Transmural Ischemia
- Anterior MI: infarct of anterior/lateral wall of LV
- Inferior MI: infarct of inferior wall of LV
- ST segment (& reciprocal) changes generally seen within minutes of blood flow occlusion
- Reperfusion therapy can decrease ST elevations
- Anterior MI: infarct of anterior/lateral wall of LV
- Inferior MI: infarct of inferior wall of LV
- ST segment (& reciprocal) changes generally seen within minutes of blood flow occlusion
- Reperfusion therapy can decrease ST elevations
Thanks to these amazing website for the wonderful graphics:
litfl.com/myocardial-isc…
grepmed.com/images/3929/ek…
ccasociety.org/education/echo…
Stay tuned for the next thread on Q-waves!
litfl.com/myocardial-isc…
grepmed.com/images/3929/ek…
ccasociety.org/education/echo…
Stay tuned for the next thread on Q-waves!
• • •
Missing some Tweet in this thread? You can try to
force a refresh