Interesting case in this patient with acute right-sided weakness
#neurorad #neurotwitter #meded #Neurosurgery #Neurology @TheASNR @RSNA #medtwitter



#neurorad #neurotwitter #meded #Neurosurgery #Neurology @TheASNR @RSNA #medtwitter
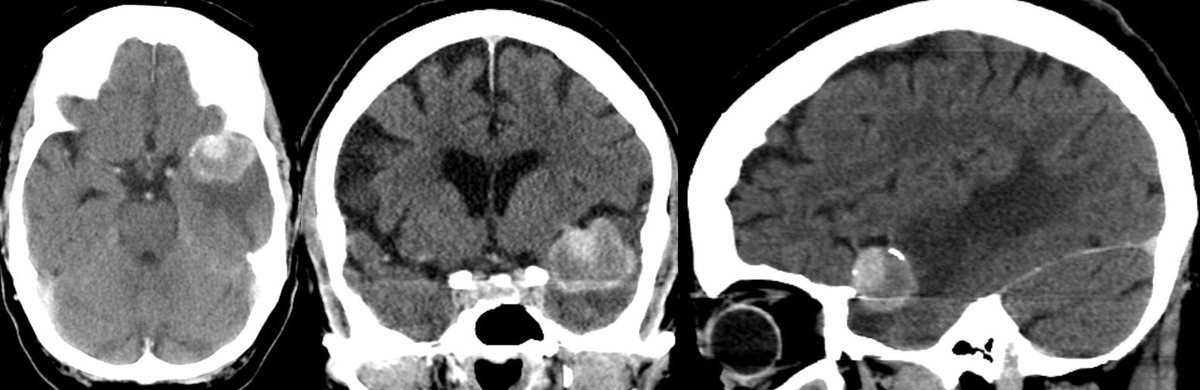


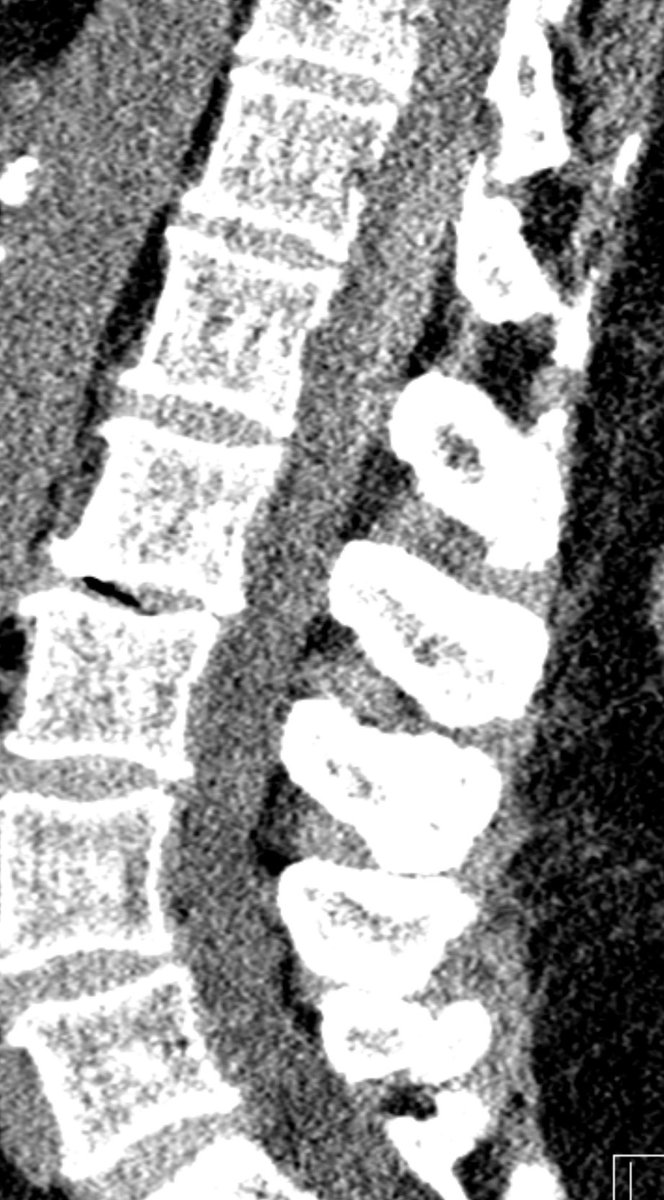
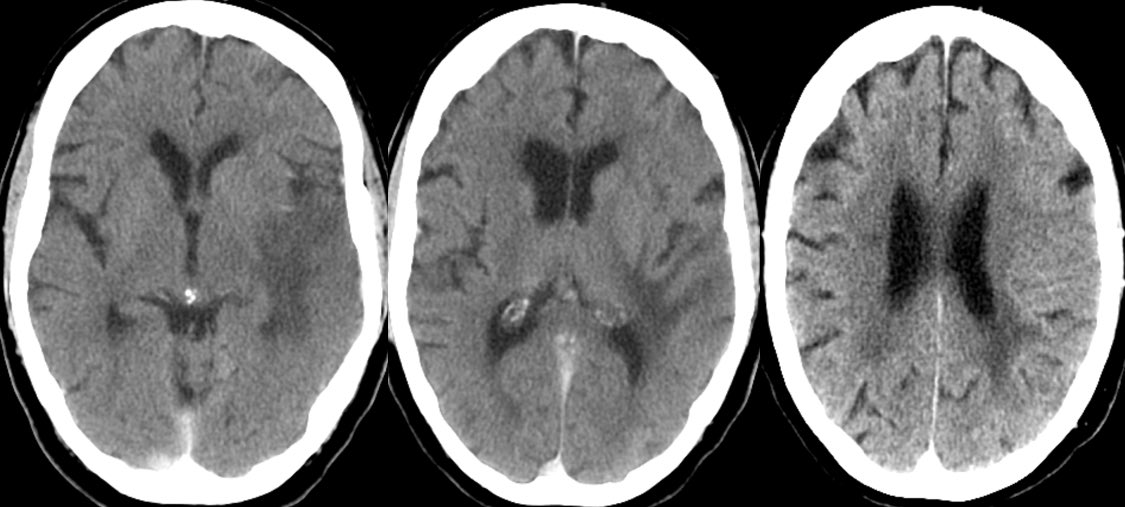
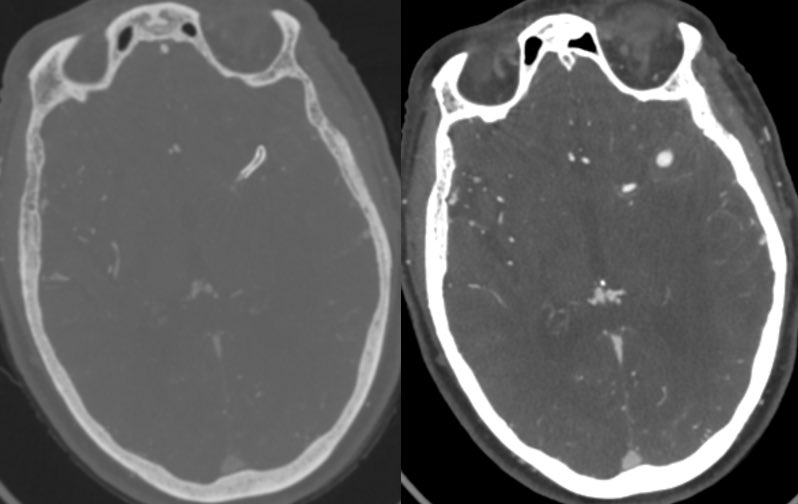
Can you determine the diagnosis off the CT?
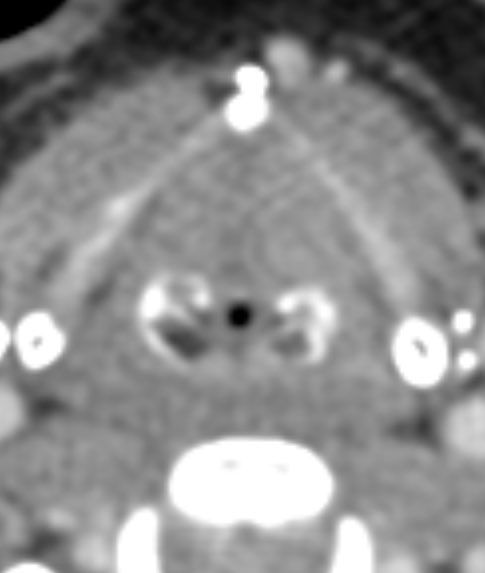
▶️Initial non-con CT shows a 3cm hyperdense lobulated extra-axial mass in the expected region of the left MCA bifurcation, consistent with a giant aneurysm. There are associated peripheral calcifications
▶️ What is the cause of the surrounding hypodensity?
▶️ What is the cause of the surrounding hypodensity?
What is the cause for the surrounding hypodensity?
▶️Mass effect and/leakage from the aneurysm induces vasogenic edema which moves easily through the white matter and relatively spares the more dense gray matter.
▶️However, we also see more subtle hypodensity of the lateral temporal lobe cortex, suspicious for acute ischemia


▶️However, we also see more subtle hypodensity of the lateral temporal lobe cortex, suspicious for acute ischemia

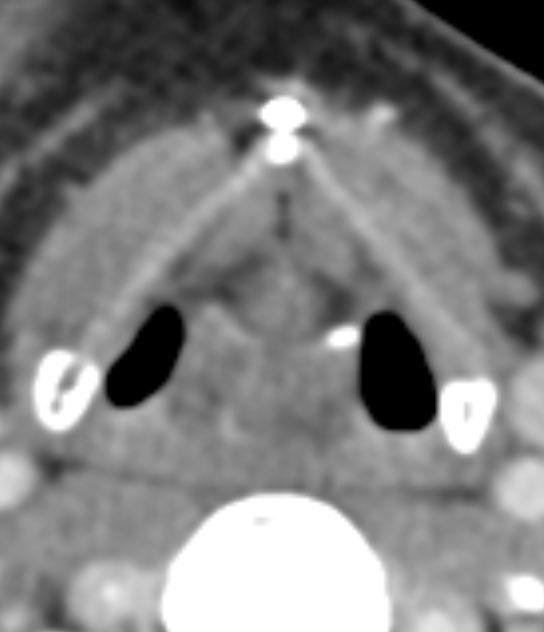
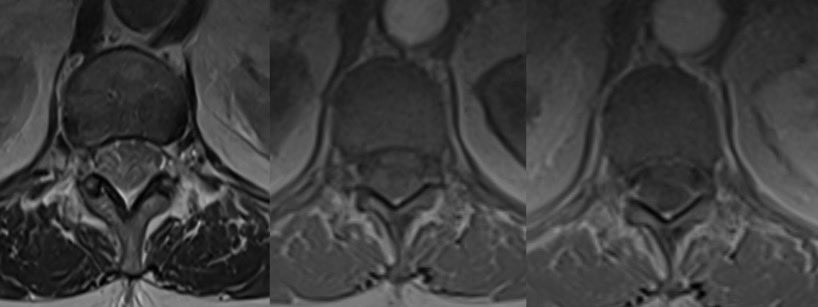
▶️CTA shows filling of the partially thrombosed aneurysm
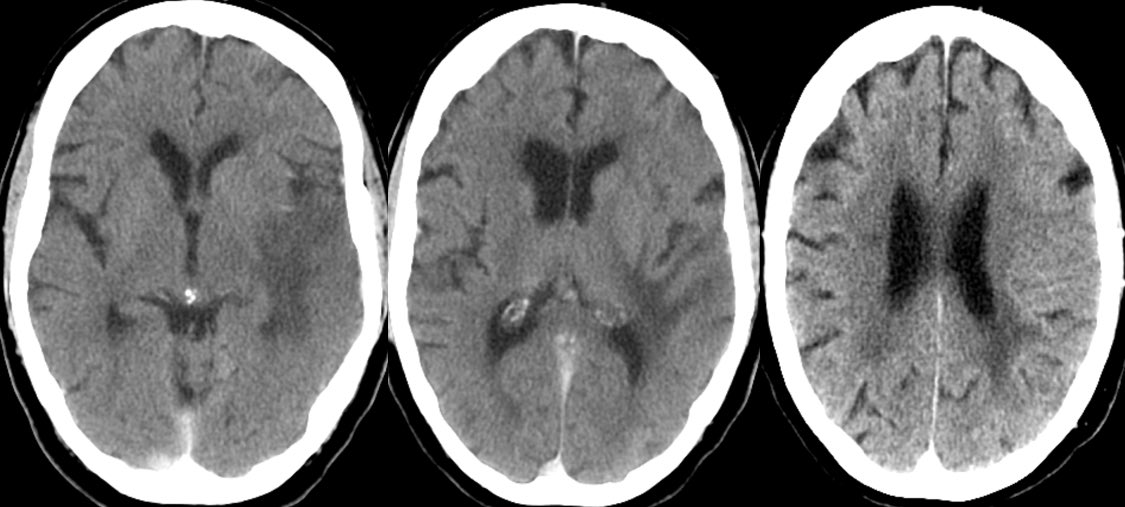
▶️CT perfusion shows reduced CBF and corresponding elevated Tmax within the left MCA territory

▶️CT perfusion shows reduced CBF and corresponding elevated Tmax within the left MCA territory

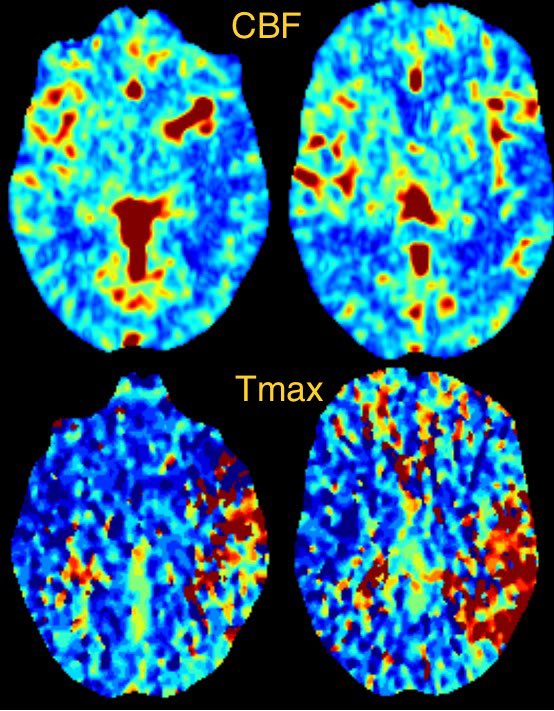
▶️I am not sure if the stroke is due to thromboembolism from intraaneurysmal thrombus or if it’s 2/2 altered flow kinetics given the large size 🤷🏻♂️ (no occlusion was seen)
▶️Thoughts welcome 🙏
▶️Thoughts welcome 🙏
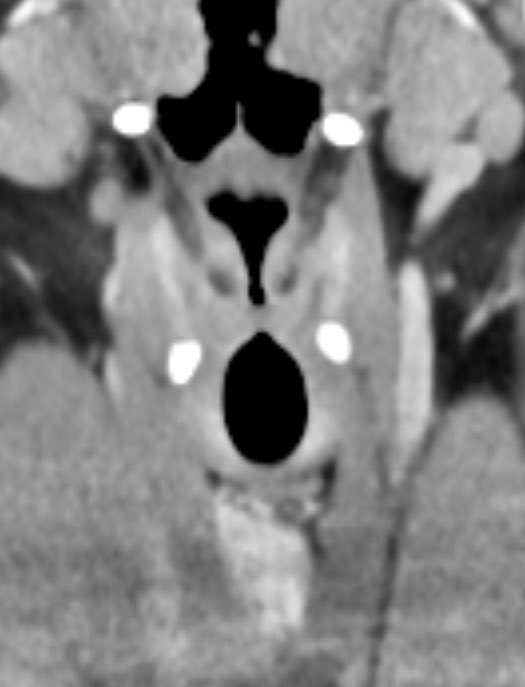
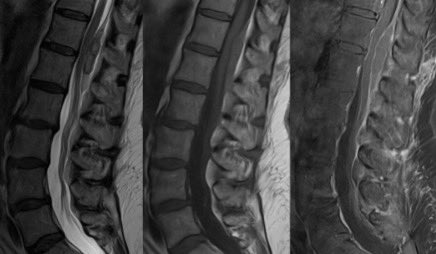
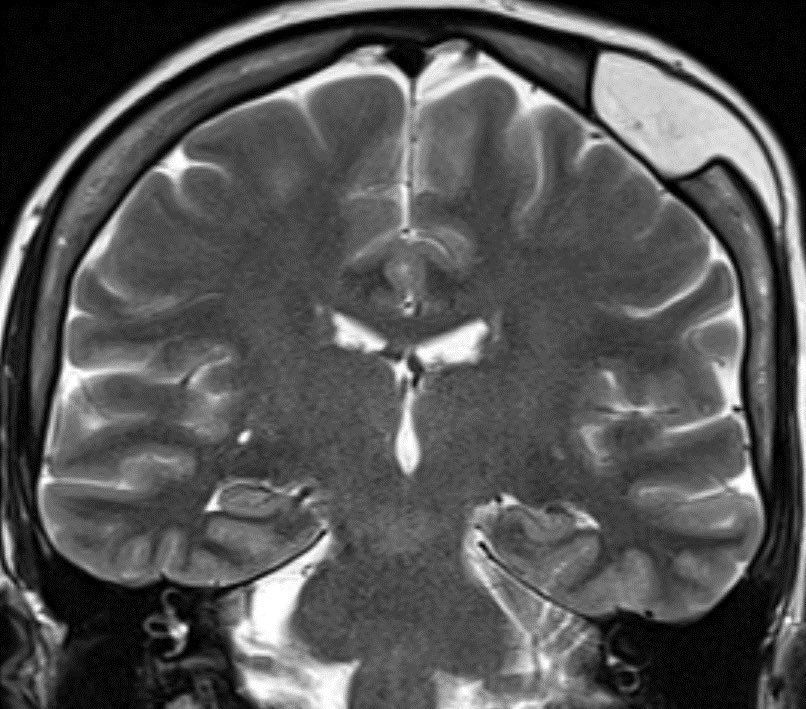
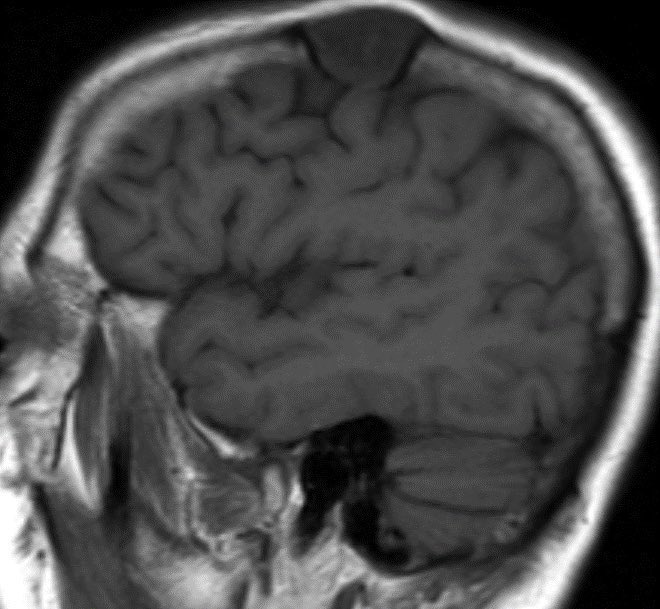
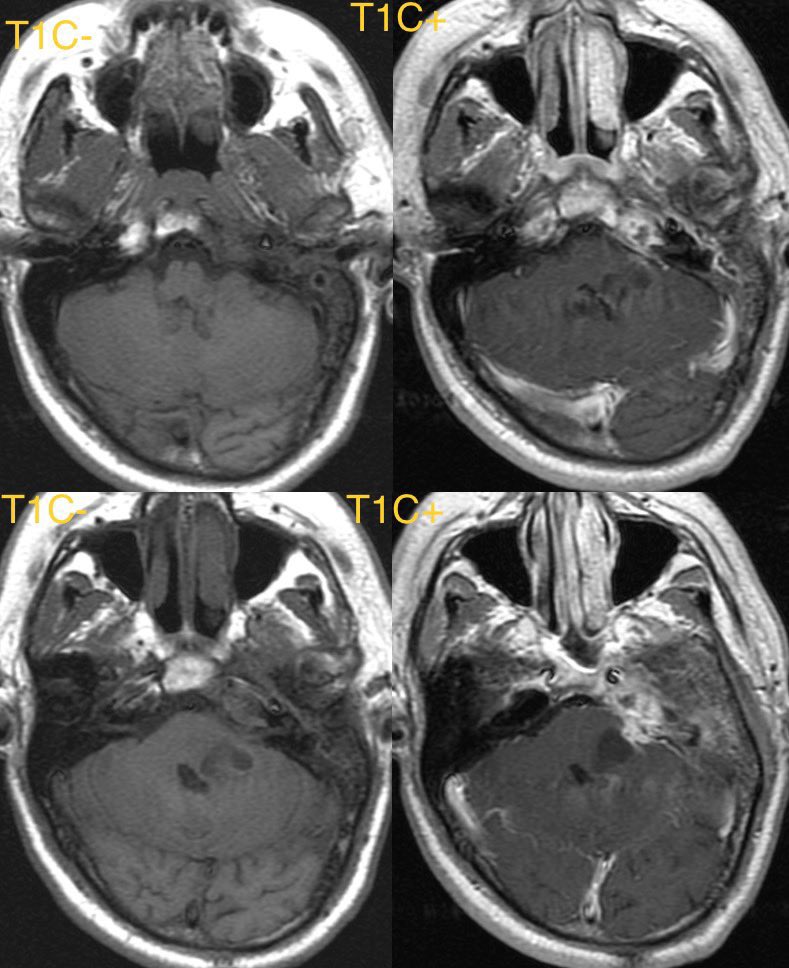
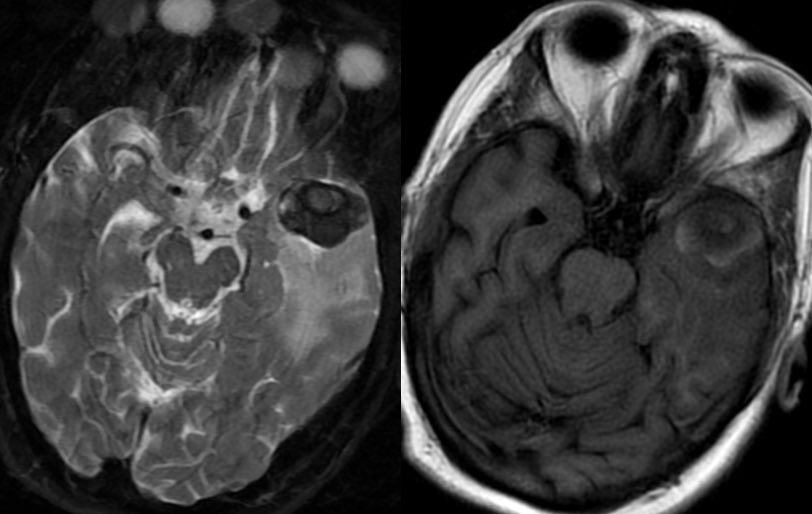
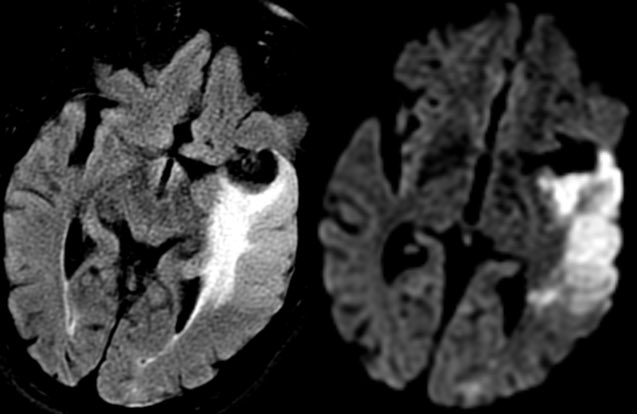
▶️MR shows the hypointense aneurysm on T2 with mixed iso and hyperintensity on T1
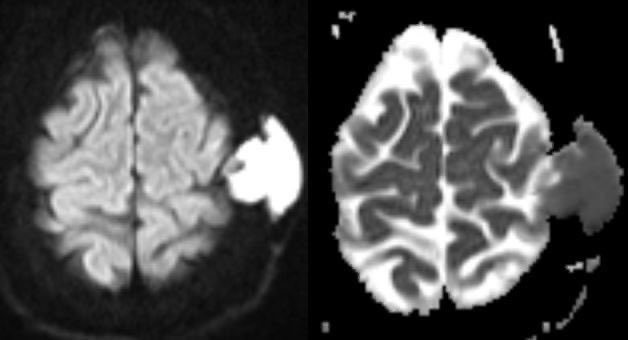
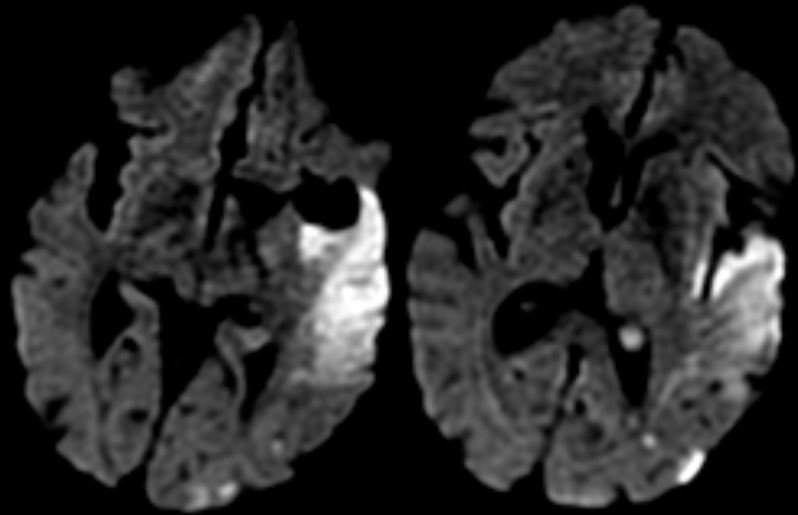
▶️ADC nicely delineates the areas of shine through from vasogenic edema and low ADC value from cytotoxic edema 2/2 infarct



▶️ADC nicely delineates the areas of shine through from vasogenic edema and low ADC value from cytotoxic edema 2/2 infarct
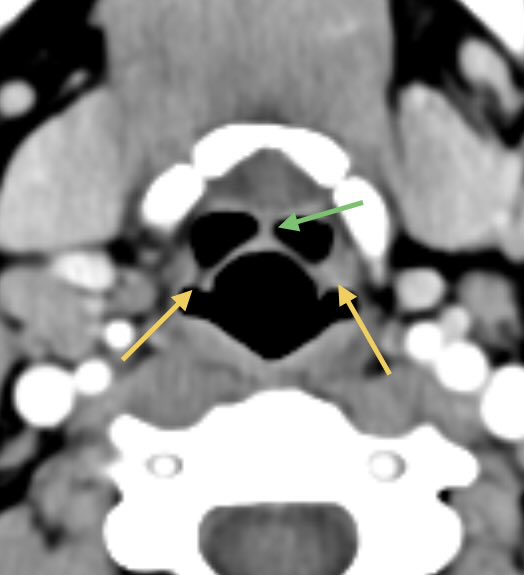
▶️The aneurysm was treated with flow diversion using a pipeline shield rather than coiling due to a wide neck.
▶️Follow up, shows persistent filling of the sac despite stent placement

▶️Follow up, shows persistent filling of the sac despite stent placement

Learning points:
💡 Most intracranial aneurysms are asymptomatic
💡 Complications include rupture and rarely stroke
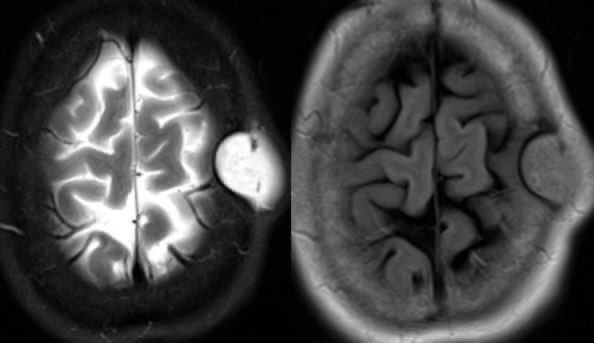
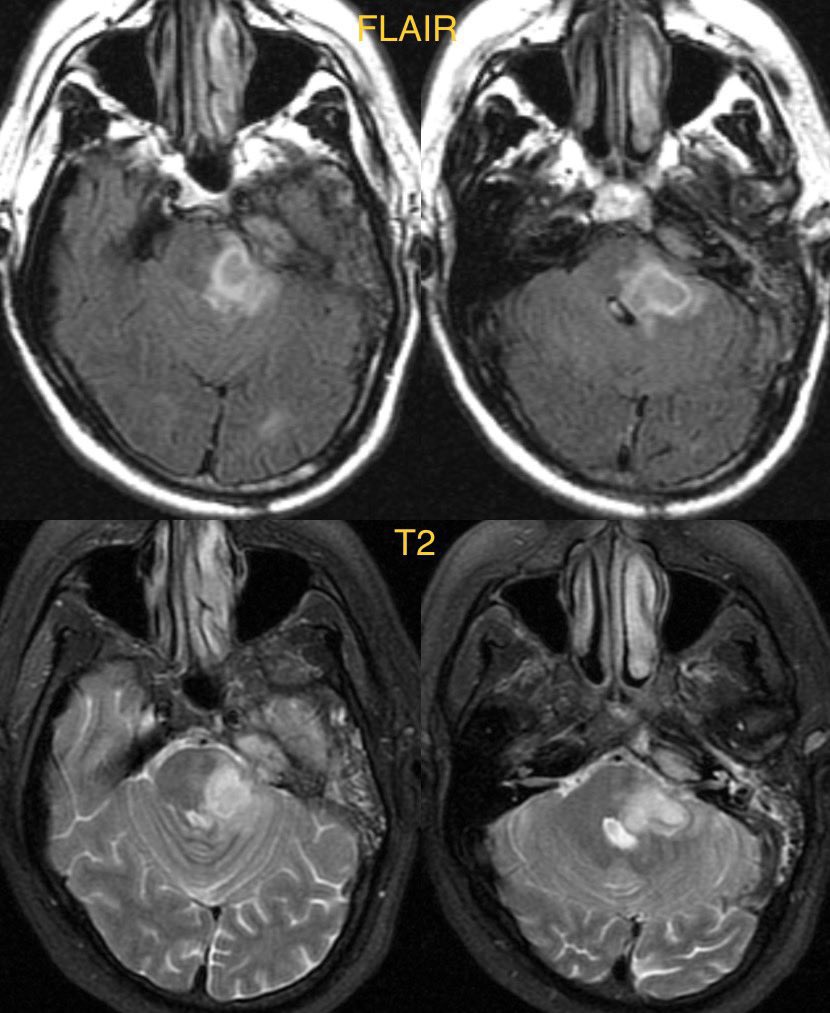
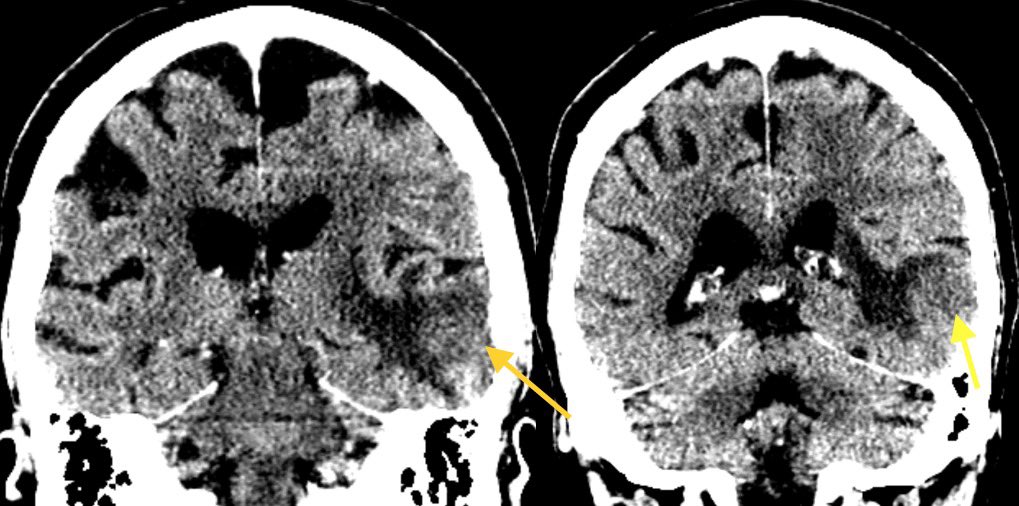
💡 When you see vasogenic edema around an aneurysm you must worry about impending rupture/leaking (as shown below, 24 hours apart in a different patient)

💡 Most intracranial aneurysms are asymptomatic
💡 Complications include rupture and rarely stroke
💡 When you see vasogenic edema around an aneurysm you must worry about impending rupture/leaking (as shown below, 24 hours apart in a different patient)


• • •
Missing some Tweet in this thread? You can try to
force a refresh