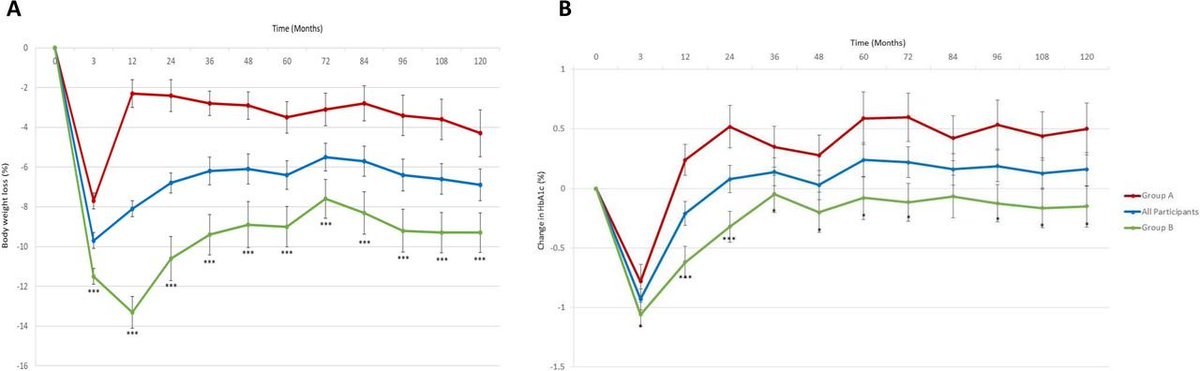
This systematic review and meta-analysis finds little evidence for or against recommending the dietary inclusion of legumes for the purpose of cardiovascular disease and type 2 diabetes prevention for healthy general populations.
- This study aimed to systematically review the evidence for associations between consumption of legumes and cardiovascular disease, type 2 diabetes and their risk factors among healthy adults using both observational and intervention studies.
- Findings from observational studies (generally with low legume consumption) did not support an association, although clinical trials did indicate some likely beneficial (although clinically small) effects on blood lipids and fasting glucose.
Legume consumption in adults and risk of cardiovascular disease and type 2 diabetes: a systematic review and meta-analysis (open access)
doi.org/10.29219/fnr.v…
#nutrition #diet
doi.org/10.29219/fnr.v…
#nutrition #diet
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter