The conventional diuretic treatment of ascites in patients with cirrhosis is high doses of spironolactone w/furosemide (classic 100/40 ratio). This was also mentioned recently on @thecurbsiders. Where does this come from and is it true? A quick🧵. #MedTwitter #nephtwitter
In 1981 Fogel et al compared 3 diuretic strategies in 90 patients w/cirrhosis
1.spironolactone + lasix prn
2.lasix alone
3.spironolactone + lasix
🔥Furosemide alone appeared to perform worst for weight loss though not statistically sig. Required sig up-titration and massive KCl
1.spironolactone + lasix prn
2.lasix alone
3.spironolactone + lasix
🔥Furosemide alone appeared to perform worst for weight loss though not statistically sig. Required sig up-titration and massive KCl

In 1983 Perez-Ayuso et al: lasix v spiro. in 40 pts w/cirrhosis and nml kidney function
If🚫response (UNa excretion <50mmol/d) alt. tx given
🔥Lasix grp: 50% response
🔥90% of non-responders responded to spiro.
🔥spiro. grp: 95% responded: 1 non-responder🚫response to lasix
If🚫response (UNa excretion <50mmol/d) alt. tx given
🔥Lasix grp: 50% response
🔥90% of non-responders responded to spiro.
🔥spiro. grp: 95% responded: 1 non-responder🚫response to lasix

Conclusions from the above:
🔥Furosemide alone is a poor choice - perhaps ineffective and comes with more electrolyte disturbances like hypokalemia which can precipitate encephalopathy
🔥spiro alone seems effective but takes longer to work
🔥combo therapy works faster
🔥Furosemide alone is a poor choice - perhaps ineffective and comes with more electrolyte disturbances like hypokalemia which can precipitate encephalopathy
🔥spiro alone seems effective but takes longer to work
🔥combo therapy works faster
In modern times a 2003 study from Santos et al randomized 100 pts w/cirrhosis to spiro + lasix or spiro alone.
🔥No difference in mobilization of ascites
🔥No diff. in response time
🔥No diff in AEs
🔥⬆️need to reduce diuretic dose in combo group to avoid excessive diuresis
🔥No difference in mobilization of ascites
🔥No diff. in response time
🔥No diff in AEs
🔥⬆️need to reduce diuretic dose in combo group to avoid excessive diuresis

In 2010 Angeli et al randomized 100 pts to combo spiro + lasix or spiro alone with addition of lasix in case of non-response. Both in escalating doses.
🔥Overall response rate was the same b/w groups
🔥Combo therapy worked faster
🔥Increased AEs w/sequential therapy (mainly⬆️K)
🔥Overall response rate was the same b/w groups
🔥Combo therapy worked faster
🔥Increased AEs w/sequential therapy (mainly⬆️K)

So: mostly older studies suggesting poor response to lasix and superiority of spiro. Even if true then why? Conclusions will cite activation of the RAAS but that's not true in HF (or most causes of volume overload) where the RAAS is also revved⬆️and loops are preferred diuretic
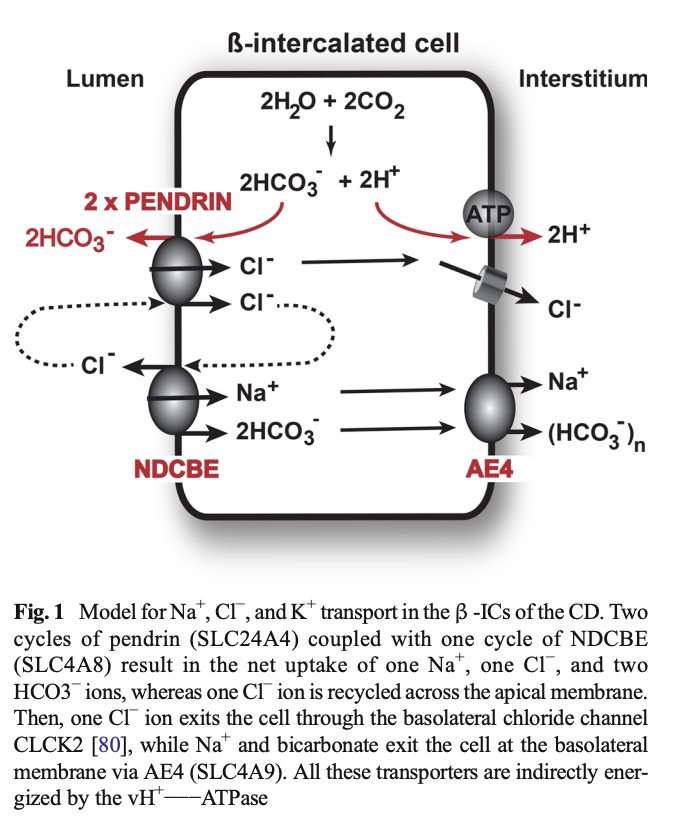
Another theory is impaired tubular secretion
💡Loop diuretics have to be secreted into the tubule via OATs to reach their site of action, whereas spironolactone doesn't
This study suggests impairment in furosemide transport in pts with alcoholic liver dz pubmed.ncbi.nlm.nih.gov/3466836/
💡Loop diuretics have to be secreted into the tubule via OATs to reach their site of action, whereas spironolactone doesn't
This study suggests impairment in furosemide transport in pts with alcoholic liver dz pubmed.ncbi.nlm.nih.gov/3466836/

Although this study suggests a significant increase in tubular secretion (at least of creatinine) in patients with compensated cirrhosis as shown by a significant decrease in creatinine based GFR with cimetidine administration, which inhibits tubular secretion. (PMID: 11749665) 

Conclusion
🔥idea that spiro is a better diuretic in cirrhosis seems to be perpetuated from small studies
🔥questionable pharmacologic basis
🔥maybe true for outpatients but inpatients I still prefer loops
I also don't treat a lot of these anymore so curious what experts think
🔥idea that spiro is a better diuretic in cirrhosis seems to be perpetuated from small studies
🔥questionable pharmacologic basis
🔥maybe true for outpatients but inpatients I still prefer loops
I also don't treat a lot of these anymore so curious what experts think
• • •
Missing some Tweet in this thread? You can try to
force a refresh