What is the most likely diagnosis in this 30 y/o w/ history of discitis/osteomyelitis presenting w/ fevers, chills, and neck pain? 🧠
#ent #Neurosurgery #Neurology #medtwitter #MedEd @The_ASSR #NeuroTwitter



#ent #Neurosurgery #Neurology #medtwitter #MedEd @The_ASSR #NeuroTwitter




Answer: Longus Colli Calcific Tendinitis
▶️Etiology: inflammatory reaction in response to deposition of calcium hydroxyapatite crystals (just like in the rotator cuff)
▶️This case is a bit tricky as the history is somewhat misleading (though it often is in radiology)
▶️Etiology: inflammatory reaction in response to deposition of calcium hydroxyapatite crystals (just like in the rotator cuff)
▶️This case is a bit tricky as the history is somewhat misleading (though it often is in radiology)
Imaging:
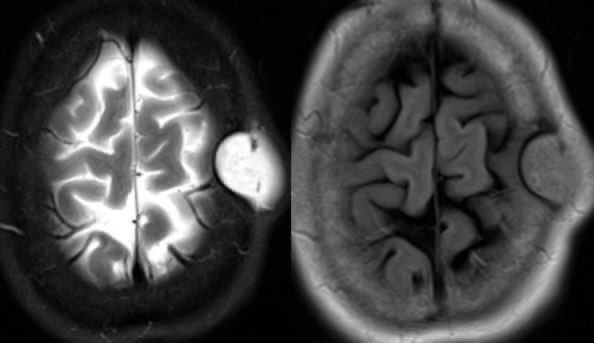
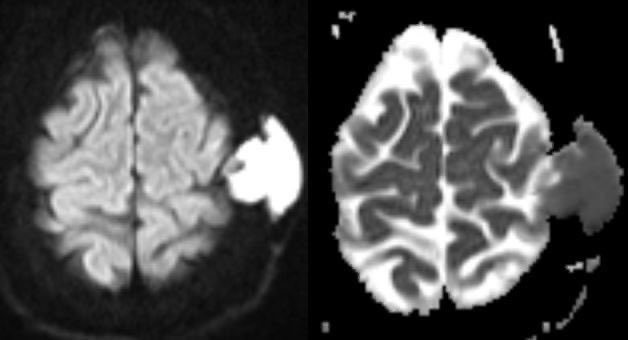
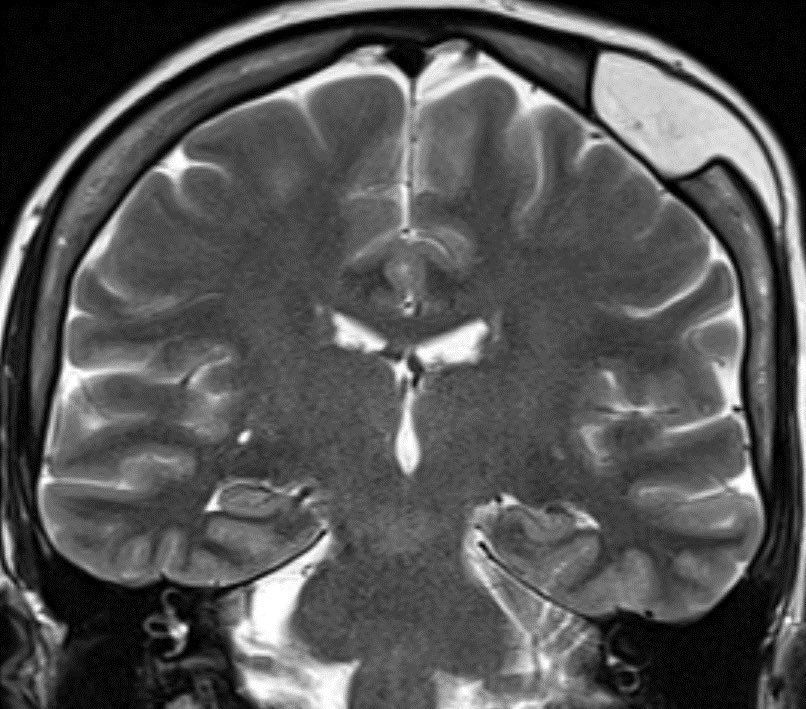
▶️Sagittal STIR shows marked retropharyngeal/prevertebral edema (yellow arrow) and focal hypointensity from the hydroxyapatite crystals (green arrow)
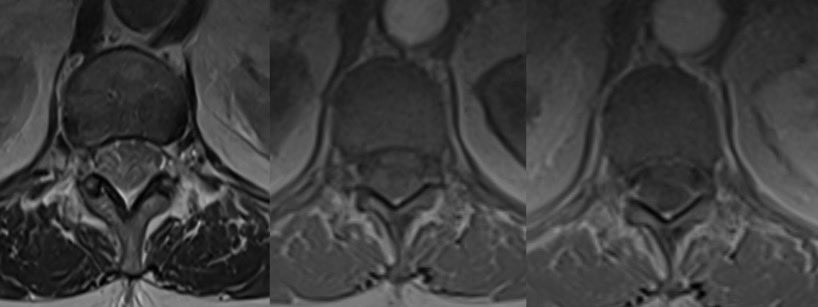
▶️Axial T2 again shows the marked edema

▶️Sagittal STIR shows marked retropharyngeal/prevertebral edema (yellow arrow) and focal hypointensity from the hydroxyapatite crystals (green arrow)
▶️Axial T2 again shows the marked edema


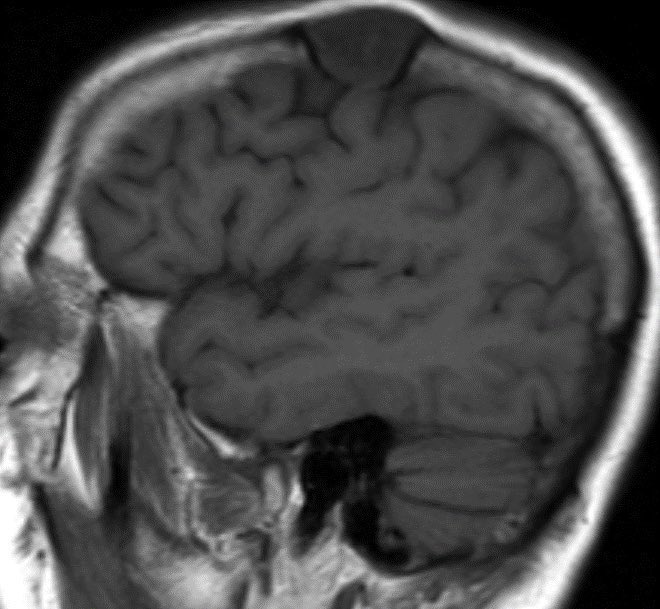
▶️T2* is key in this case showing the markedly hypointense amorphous calcs at the longus colli tendons
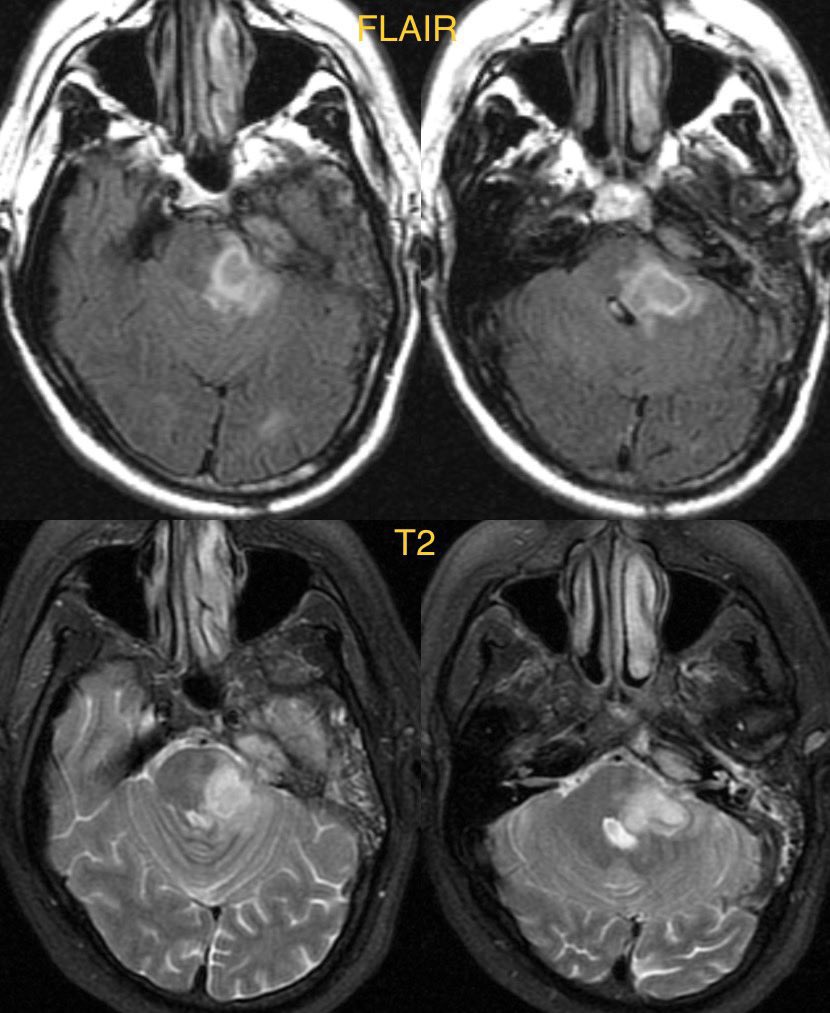
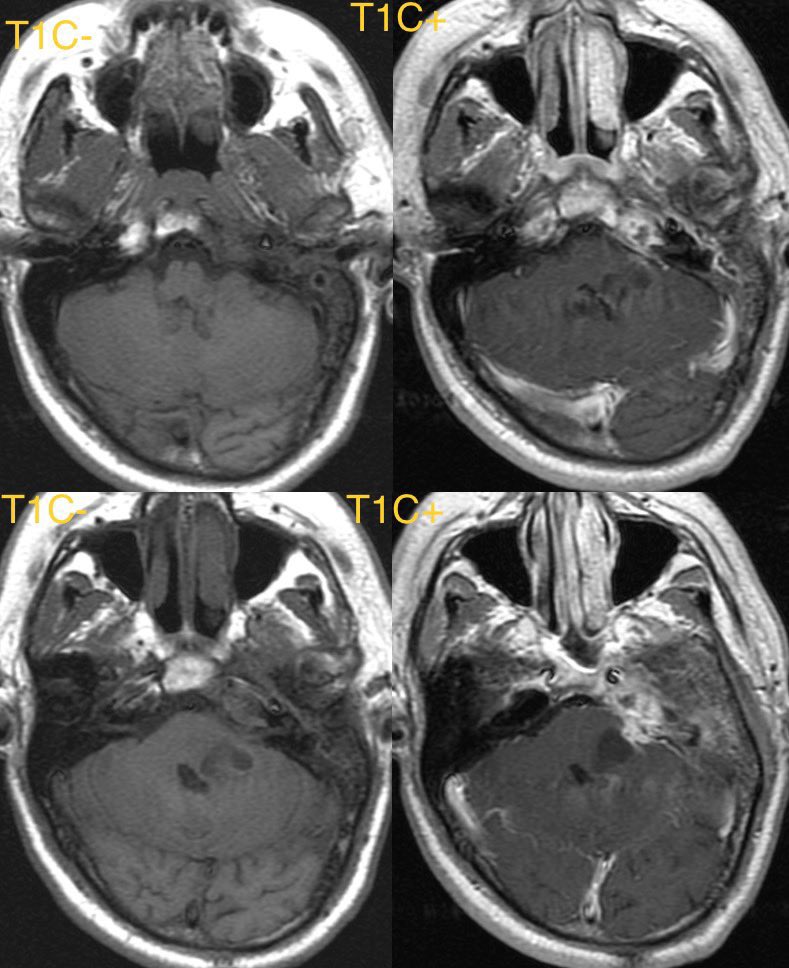
▶️Pre and post con T1 shows the edema w/ reactive enhancement (yellow arrows) and the focal hypointense calcs (green arrows)

▶️Pre and post con T1 shows the edema w/ reactive enhancement (yellow arrows) and the focal hypointense calcs (green arrows)


General imaging features:
▶️Amorphous calcifications at C1-C2 junction near the insertion of the longus colli muscles is pathognomonic
▶️ Be careful not to mix up calcification at the C1-C2 junction w/ the more common COARSE calcs in DJD!
▶️Amorphous calcifications at C1-C2 junction near the insertion of the longus colli muscles is pathognomonic
▶️ Be careful not to mix up calcification at the C1-C2 junction w/ the more common COARSE calcs in DJD!
Imaging cont:
▶️Calcs on MR can be trickier, look for MARKED FOCAL HYPOINTENSITY on T2*/GRE at the C1-C2 JUNCTION
▶️Expect prevertebral and/or retropharyngeal edema
▶️Reactive soft tissue enhancement on T1C+
▶️Calcs on MR can be trickier, look for MARKED FOCAL HYPOINTENSITY on T2*/GRE at the C1-C2 JUNCTION
▶️Expect prevertebral and/or retropharyngeal edema
▶️Reactive soft tissue enhancement on T1C+
DDX:
Must differentiate from infection (as calcific tendinitis is treated with time and NSAIDs)
▶️For infection, expect a more spherical or convex retropharyngeal collection, more enhancement, and presence of head and neck infection
Must differentiate from infection (as calcific tendinitis is treated with time and NSAIDs)
▶️For infection, expect a more spherical or convex retropharyngeal collection, more enhancement, and presence of head and neck infection
▶️Calcifications at the C1-C2 junction are pathognomonic for calcific longus colli tendonitis 🧠
Companion cases:
▶️Radiograph showing prevertebral swelling and amorphous calcs on C1-C2 junction
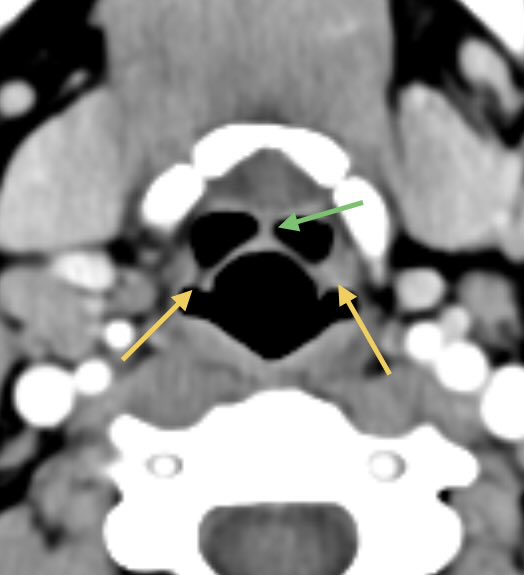
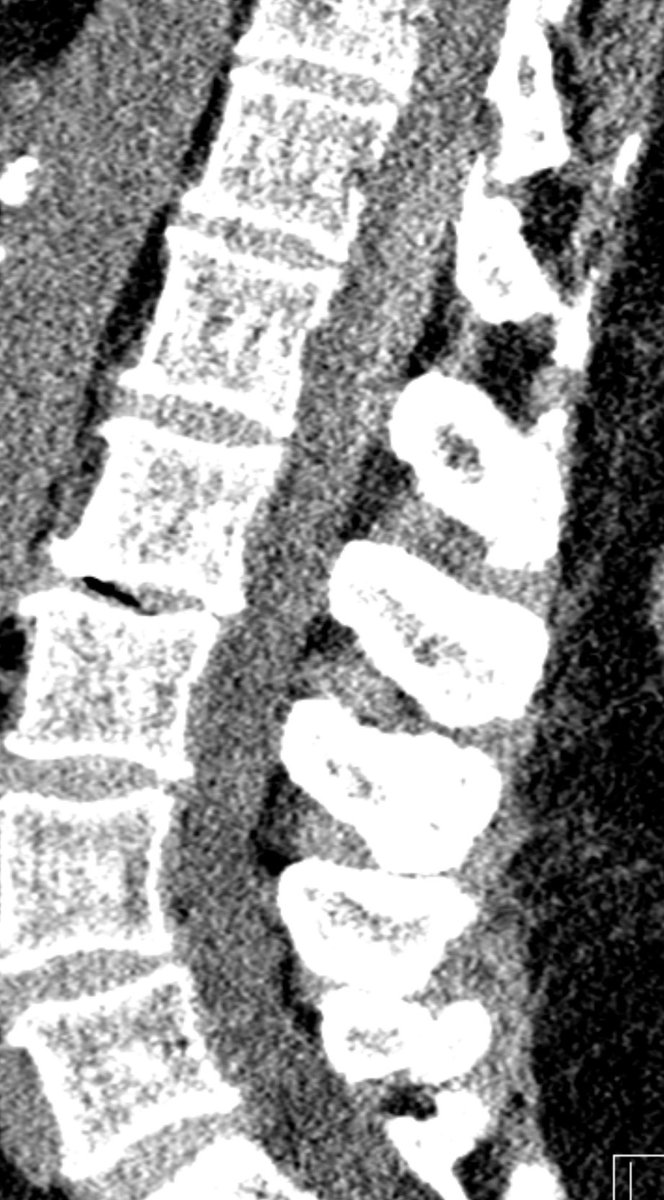
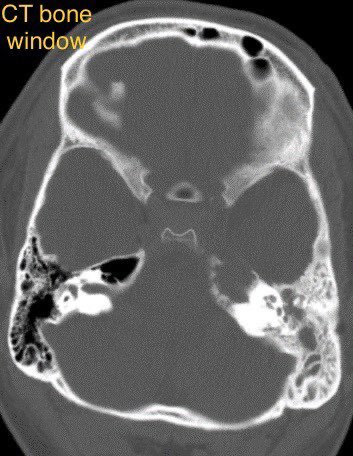
▶️Appearance on CT in a different patient showing the amorphous calcs and edema


Companion cases:
▶️Radiograph showing prevertebral swelling and amorphous calcs on C1-C2 junction
▶️Appearance on CT in a different patient showing the amorphous calcs and edema



Companion case 3 (DJD fake out!!):
▶️CT shows COARSE calcifications at C1-C2 junction with mild pharyngeal edema (from prior radiation in this case)

▶️CT shows COARSE calcifications at C1-C2 junction with mild pharyngeal edema (from prior radiation in this case)


• • •
Missing some Tweet in this thread? You can try to
force a refresh