1/Remembering spinal fracture classifications is back breaking work!
A #tweetorial to help your remember the scoring system for thoracic & lumbar fractures—“TLICS” to the cool kids!
#medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #backpain #spine #Neurosurgery
A #tweetorial to help your remember the scoring system for thoracic & lumbar fractures—“TLICS” to the cool kids!
#medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #backpain #spine #Neurosurgery

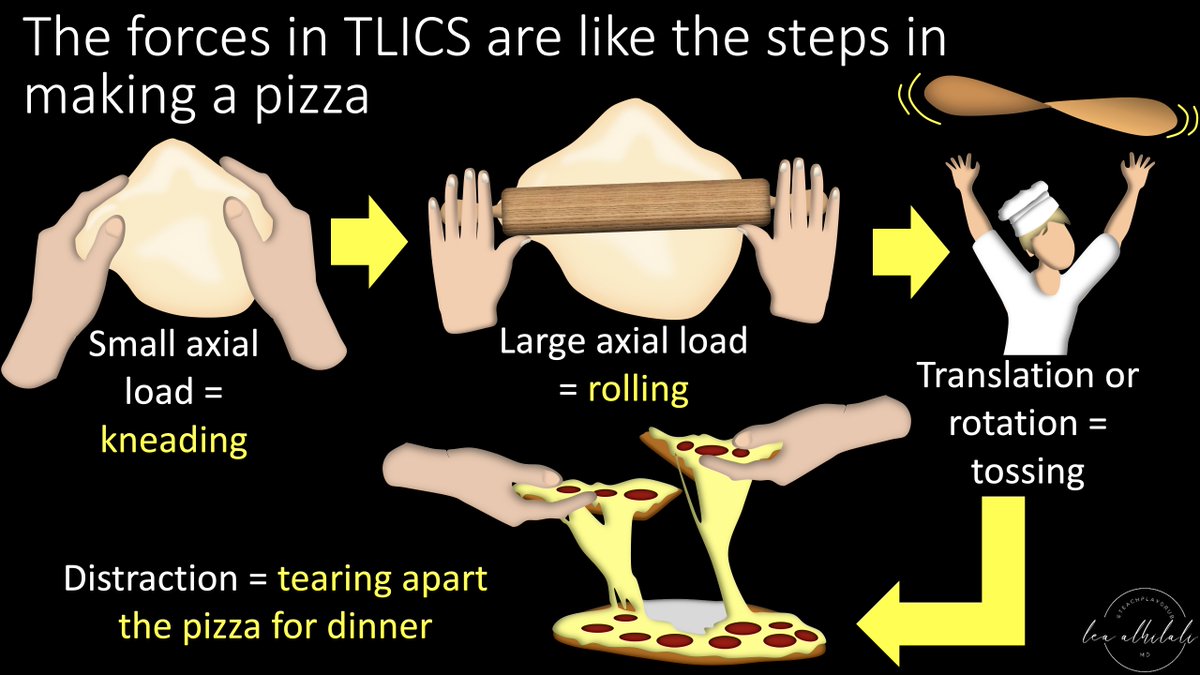
2/TLICS scores a fx on (1) morphology & (2) posterior ligamentous complex injury. Let's start w/morphology. TLICS scores severity like the steps to make & eat a pizza:
Mild compression (kneading), strong compression (rolling), rotation (tossing), & distraction (tearing in)
Mild compression (kneading), strong compression (rolling), rotation (tossing), & distraction (tearing in)
3/At the most mild, w/only mild axial loading, you get the simplest fx, a compression fx—like a simple long bone fx--worth 1 pt.
This is like when you just start to kneading the dough. There's pressure, but not as much as with a rolling pin!
This is like when you just start to kneading the dough. There's pressure, but not as much as with a rolling pin!

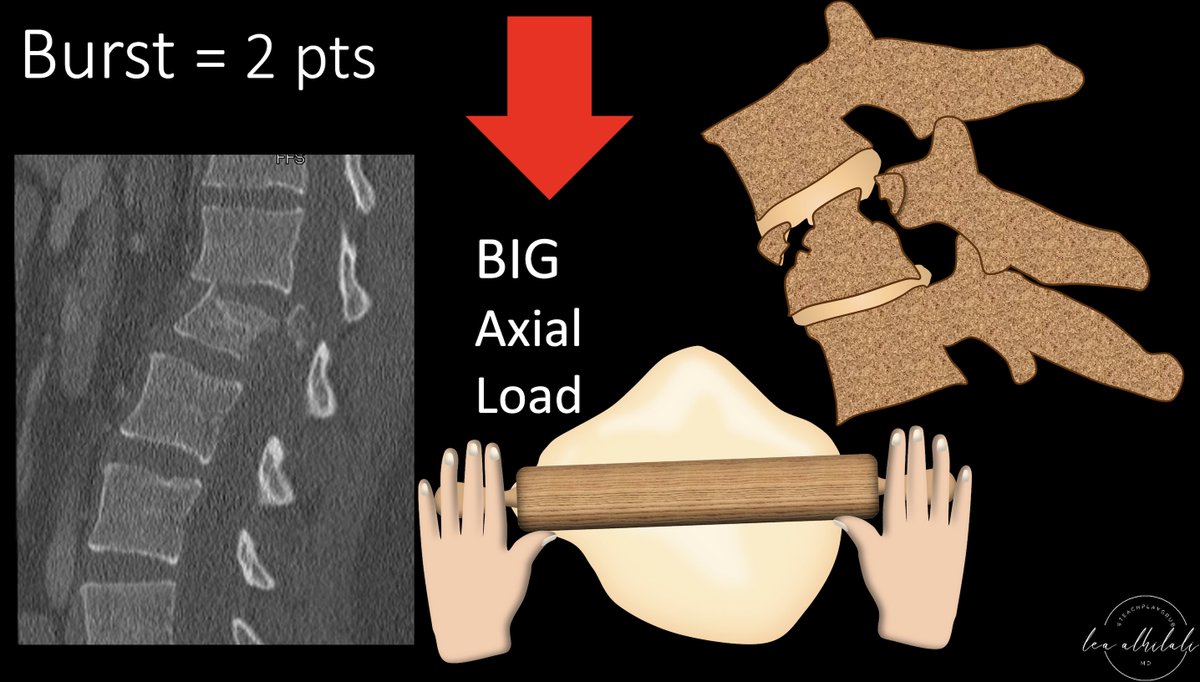
4/As the axial force grows, this becomes a burst fx with retropulsion of the posterior vertebral body—just as greater force causes more comminution in long bone fxs.
This is like moving up from your hands to the rolling pin. A burst is worth 2 points.
This is like moving up from your hands to the rolling pin. A burst is worth 2 points.
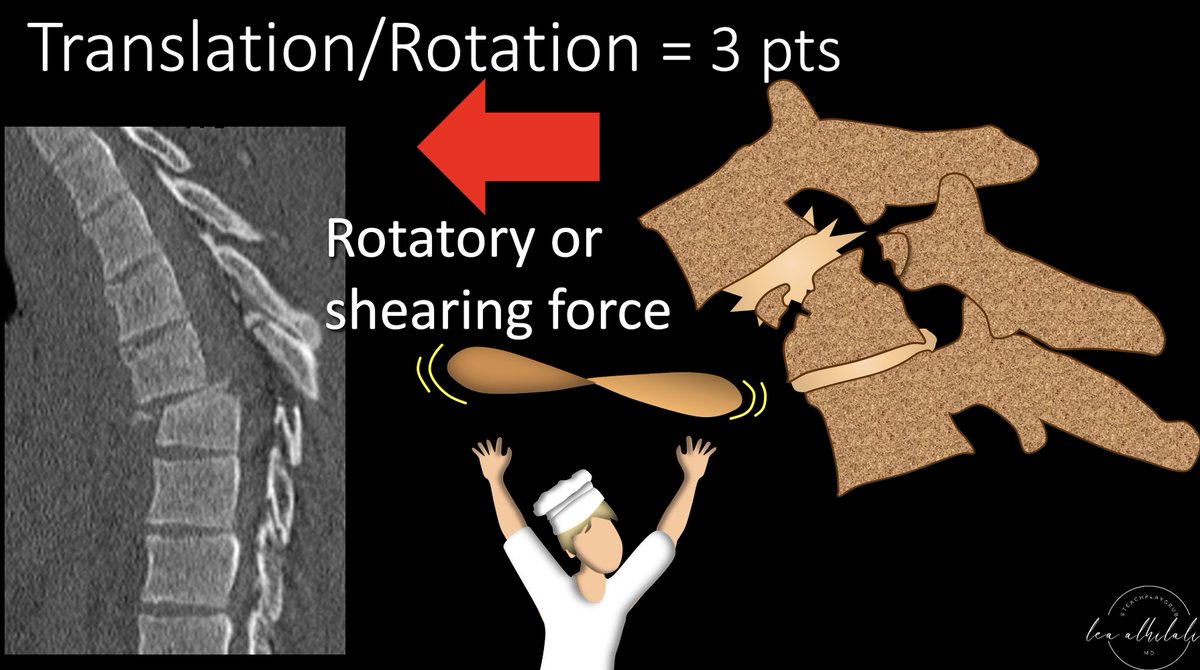
5/If the force is shearing, you rip the connection between the vertebral bodies—it's is the equivalent of pulling on a long bone & causing its dislocation from its joint or connection with another bone
This is like when you throw the pizza up into the air. This is worth 3 points
This is like when you throw the pizza up into the air. This is worth 3 points
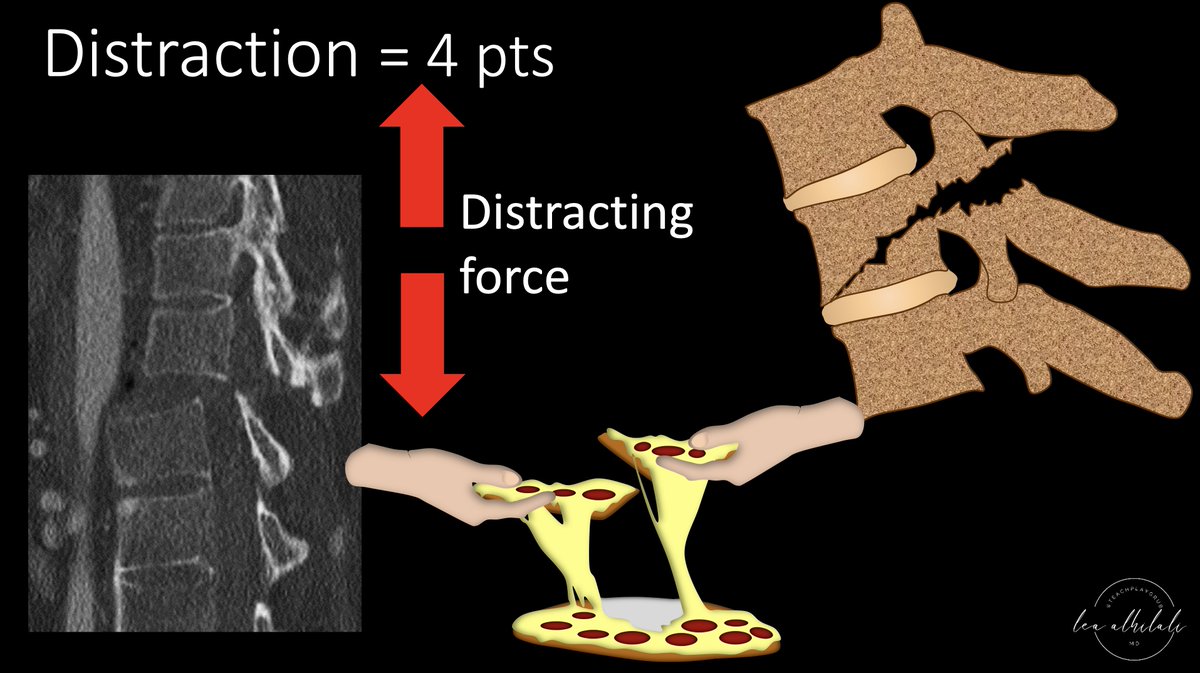
6/Similar to shear forces, distracting forces rip the vertebral bodies apart. But rather than sliding forward or back, vertebral bodies are pulled up or down, resulting in a vertical gap between the vertebrae.
It is like tearing the pizza apart to eat it. It is worth 4 points
It is like tearing the pizza apart to eat it. It is worth 4 points
7/This summarizes the TLICS scoring for fracture morphology. The higher the number, the greater the force and injury to the spine—ranging from simple compression fxs worth only 1 point to where the spine is literally ripped apart—a distraction injury, worth 4 points. 

8/The next TLICS imaging finding is the integrity of the PLC. If it is intact, you get 0 pts. If you needed a tweetorial for that, well…I can’t help you much. If there is edema, but no true rupture on MRI, that is worth 2 pts. True disruption on MRI is worth 3 pts. 

9/The difference between suspected injury & injured is like the difference of seeing smoke & suspecting fire (you see edema on MR & suspect injury) and actually seeing the fire (seeing the ligamentous tear as disruption of the T2 dark line of the ligament on MR). 

10/ Here is an example of suspected injury—edema is seen in the posterior ligamentous complex, but the T2 dark lines that are the ligaments themselves appear intact. This is worth 2 pts. 

11/If you can find a true disruption or gap in the T2 dark line of the ligament, that is considered truly disrupted and worth 3 points. 

12/Here is the summary of the scoring for PLC injury in TLICS. Edema is suspicious, but only a true gap is considered injured. 

13/So now you know how to score imaging findings in thoracolumbar fxs--I hope that takes a load off your back!
Remember, it's as easy as pizza pie!
Remember, it's as easy as pizza pie!

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















