We've just presented and published a multicenter RCT at #CCR23 and in @JAMA_current!
Continuous vs Intermittent Meropenem Administration in Critically Ill Patients with Sepsis: The #MERCYtrial!
🔗 jamanetwork.com/journals/jama/…
This 🧵 will explain the study in detail /11
#FOAMcc
Continuous vs Intermittent Meropenem Administration in Critically Ill Patients with Sepsis: The #MERCYtrial!
🔗 jamanetwork.com/journals/jama/…
This 🧵 will explain the study in detail /11
#FOAMcc
2/
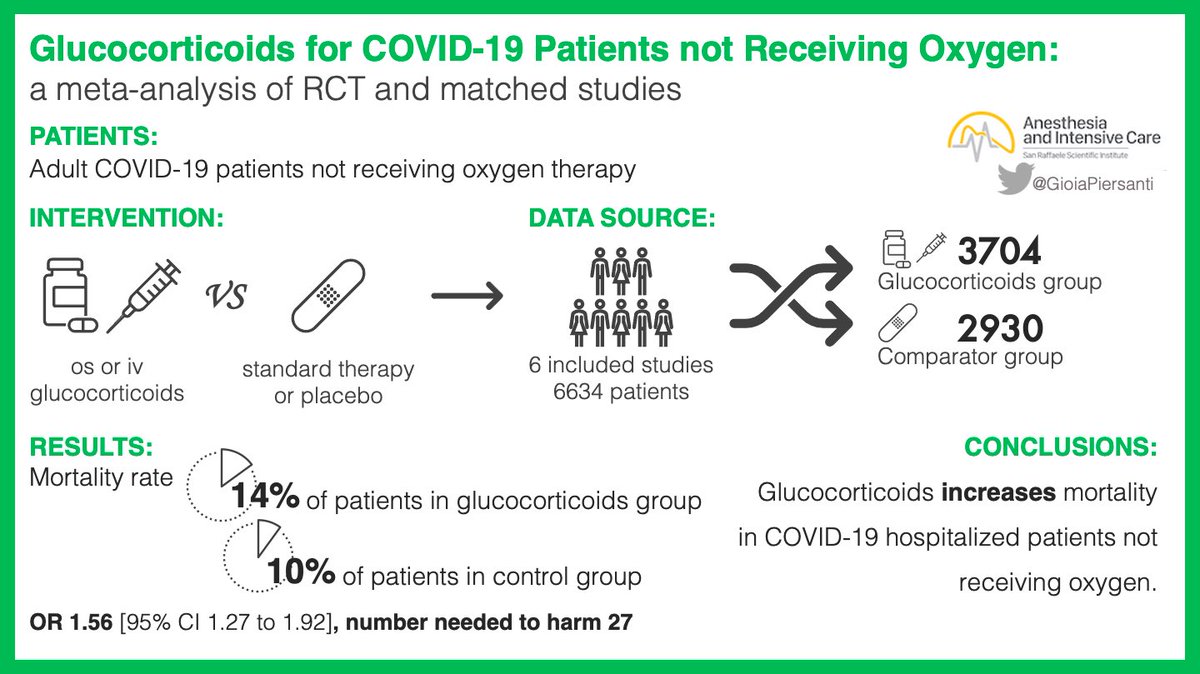
β-lactams (e.g., #meropenem), are typically given intermittently, but continuous administration can provide constant serum levels and may improve outcomes.
In fact, several meta-analyses reported reduced mortality when administered continuously.
β-lactams (e.g., #meropenem), are typically given intermittently, but continuous administration can provide constant serum levels and may improve outcomes.
In fact, several meta-analyses reported reduced mortality when administered continuously.

3/
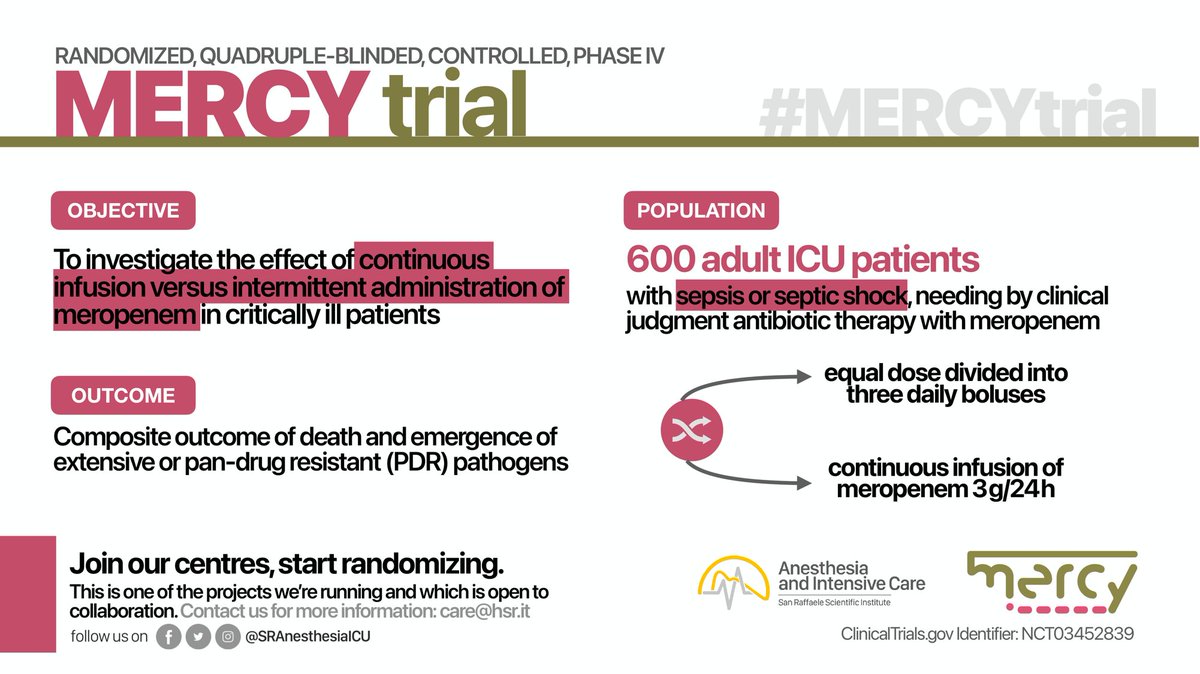
Therefore, we conducted a multinational, double-blind, randomized controlled trial to test the hypothesis that continuous administration of #meropenem, compared with intermittent administration, would improve clinically relevant outcomes in critically ill pts with #sepsis
Therefore, we conducted a multinational, double-blind, randomized controlled trial to test the hypothesis that continuous administration of #meropenem, compared with intermittent administration, would improve clinically relevant outcomes in critically ill pts with #sepsis
4/
P: ICU patients with sepsis or septic shock who needed new meropenem treatment
I: continuous infusion (3g/day)
C: intermittent administration (1g q8h)
O: composite of mortality and/or the emergence of pandrug-resistant or extensively drug-resistant bacteria at day 28
P: ICU patients with sepsis or septic shock who needed new meropenem treatment
I: continuous infusion (3g/day)
C: intermittent administration (1g q8h)
O: composite of mortality and/or the emergence of pandrug-resistant or extensively drug-resistant bacteria at day 28

5/
A total of 607 patients were randomized, 303 in the continuous and 304 in the intermittent arm.
The two arms are well-balanced
64 years old
61% with septic shock
Time from hospital admission to randomization = 9 days
A total of 607 patients were randomized, 303 in the continuous and 304 in the intermittent arm.
The two arms are well-balanced
64 years old
61% with septic shock
Time from hospital admission to randomization = 9 days

6/
The daily dose of meropenem was 3 g in both groups.
At randomization, 74% received concurrent antibiotic therapy, with glycopeptide being the most common.
Among patients with identified bacteria (71%), Klebsiella and Pseudomonas are the common gram-negative species.
The daily dose of meropenem was 3 g in both groups.
At randomization, 74% received concurrent antibiotic therapy, with glycopeptide being the most common.
Among patients with identified bacteria (71%), Klebsiella and Pseudomonas are the common gram-negative species.
7/
The primary outcome (mortality and/or emergence of PDR/XDR bacteria) was not significantly different between the two arms (47% vs 49%; RR 0.96 [95% CI 0.81–1.13]).
No interaction was found in any subgroup analysis.
#MERCYtrial
The primary outcome (mortality and/or emergence of PDR/XDR bacteria) was not significantly different between the two arms (47% vs 49%; RR 0.96 [95% CI 0.81–1.13]).
No interaction was found in any subgroup analysis.
#MERCYtrial

8/
No significant difference was observed in any secondary outcome (including 28-day mortality).
No adverse events related to meropenem (e.g., seizure) were reported.
#MERCYtrial
No significant difference was observed in any secondary outcome (including 28-day mortality).
No adverse events related to meropenem (e.g., seizure) were reported.
#MERCYtrial

9/
Conclusion
In critically ill patients with sepsis, compared with intermittent administration, the continuous administration of meropenem did not improve the composite outcome of mortality and pan or extensively drug-resistance emergence.
Conclusion
In critically ill patients with sepsis, compared with intermittent administration, the continuous administration of meropenem did not improve the composite outcome of mortality and pan or extensively drug-resistance emergence.
10/
It's our honor to publish the results of #MERCYtrial in JAMA @JAMA_current: Continuous vs Intermittent Meropenem Administration in Critically Ill Patients with Sepsis
🔗 jamanetwork.com/journals/jama/…
#FOAMcc
It's our honor to publish the results of #MERCYtrial in JAMA @JAMA_current: Continuous vs Intermittent Meropenem Administration in Critically Ill Patients with Sepsis
🔗 jamanetwork.com/journals/jama/…
#FOAMcc
11/
We thank all the patients, families, funder, investigators, and clinicians.
We also appreciate the editors/reviewers of @JAMA_current and @CritCareReviews for giving us the opportunity for the simultaneous publication/presentation.
We thank all the patients, families, funder, investigators, and clinicians.
We also appreciate the editors/reviewers of @JAMA_current and @CritCareReviews for giving us the opportunity for the simultaneous publication/presentation.
• • •
Missing some Tweet in this thread? You can try to
force a refresh

 Read on Twitter
Read on Twitter