Collaborative resource to promote ID clinical reasoning for #IDfellows | #IDTwitter #IDMedEd | https://t.co/sbD2rV1riH | infectiousdiseasesfellows@gmail.com
How to get URL link on X (Twitter) App


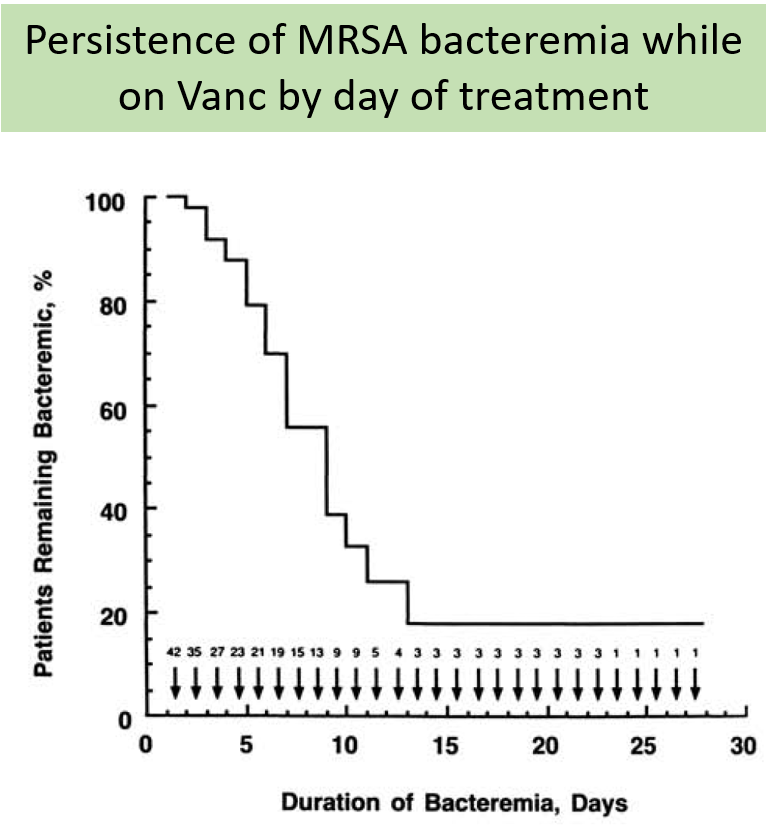
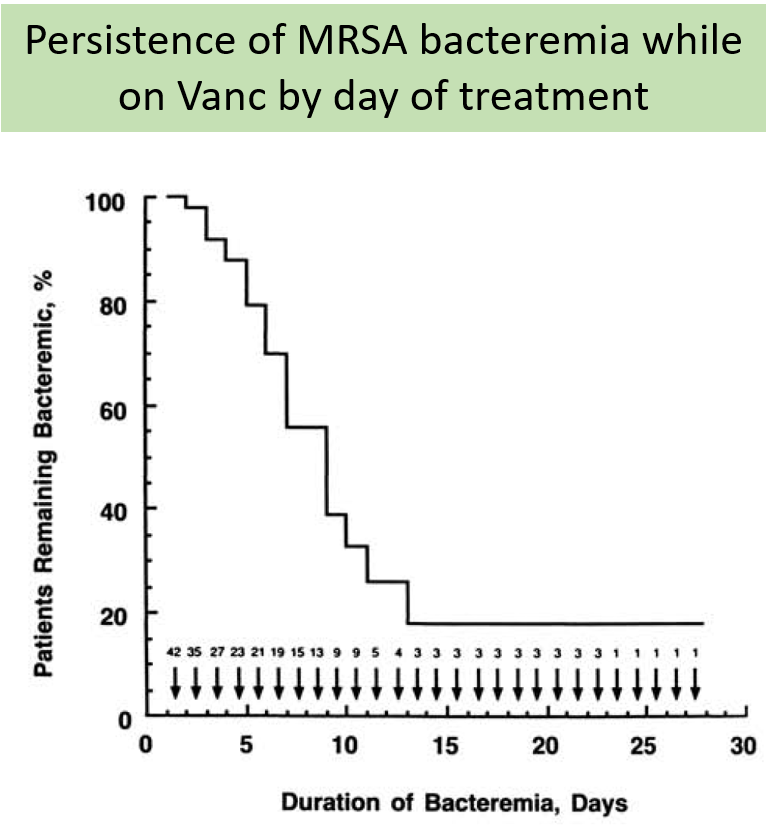
 2/ What is the best next therapeutic step?
2/ What is the best next therapeutic step?

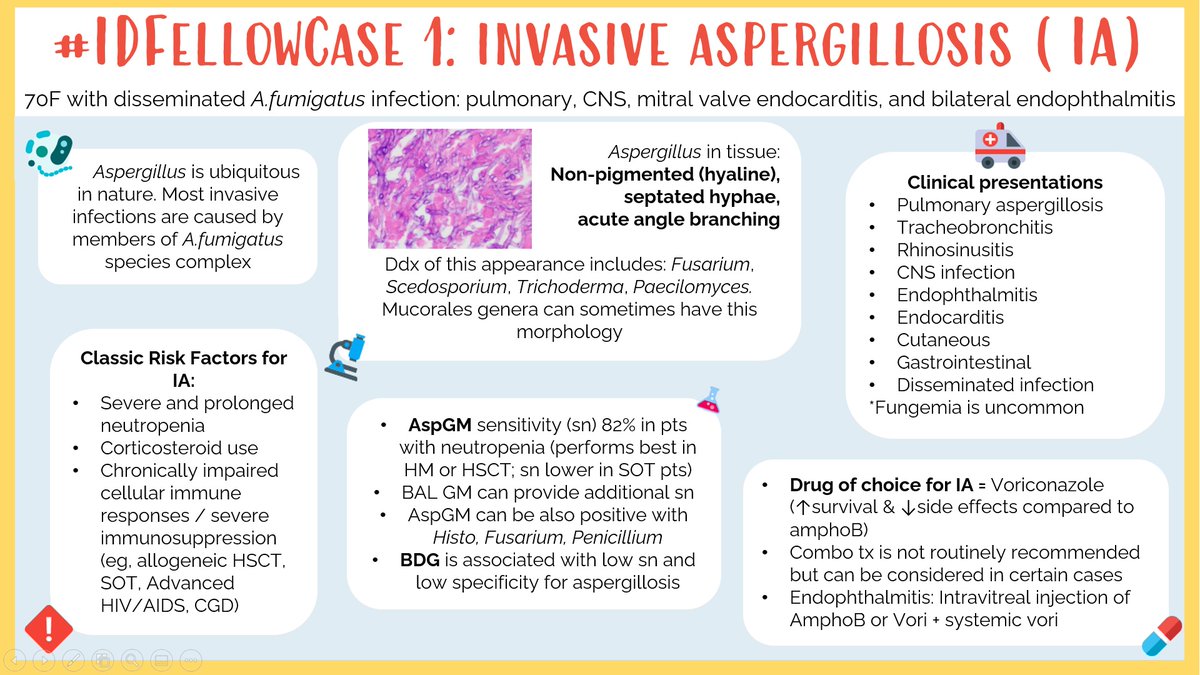
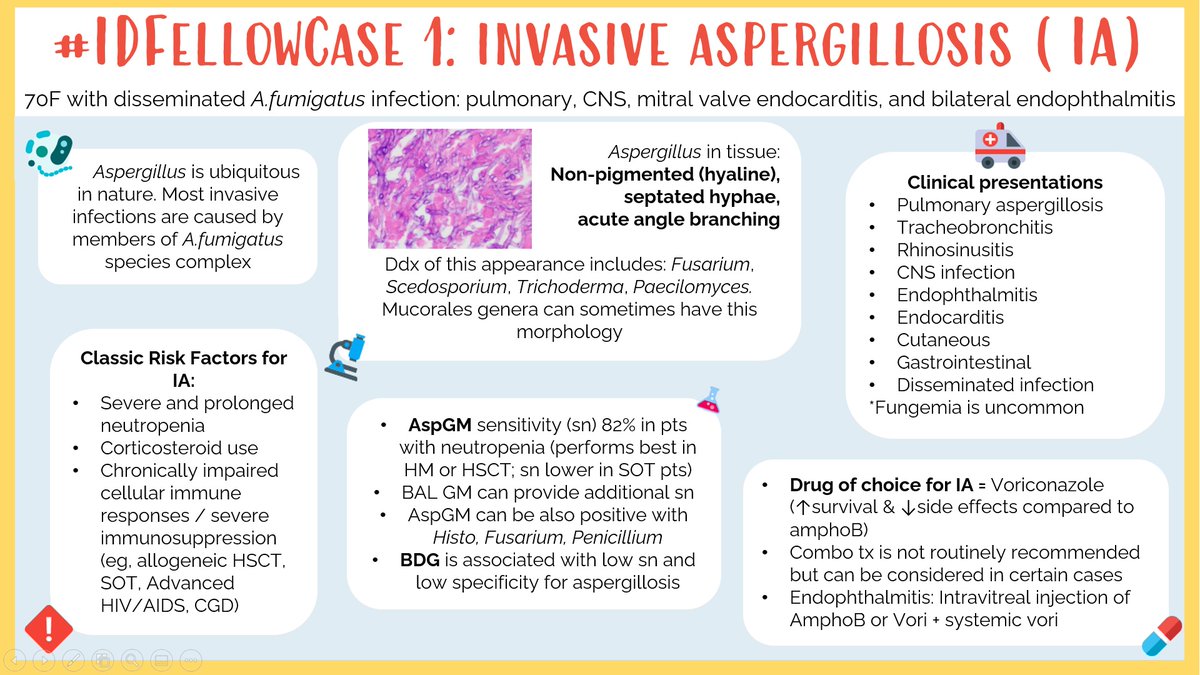
 2/ Following tissue diagnosis, what is the best next step in management?
2/ Following tissue diagnosis, what is the best next step in management?

 2/ While awaiting pending work-up, what is the best next step?
2/ While awaiting pending work-up, what is the best next step?
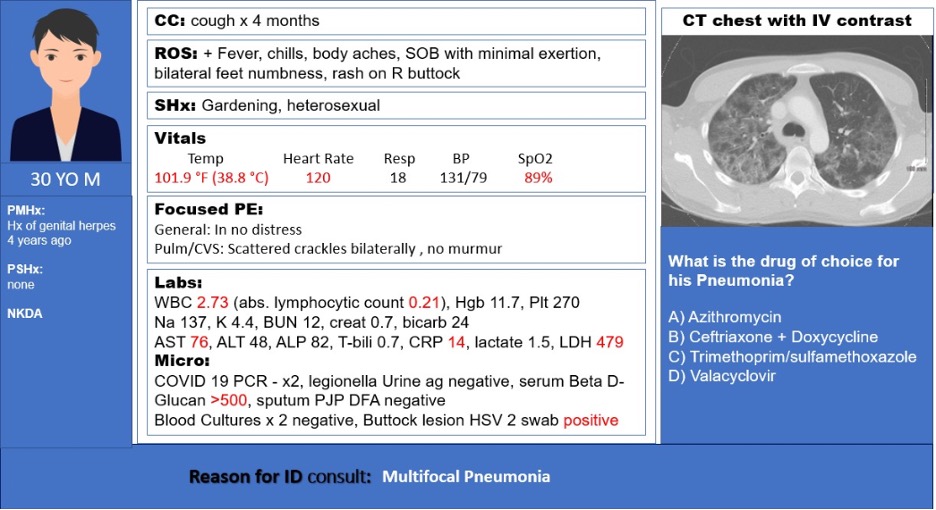
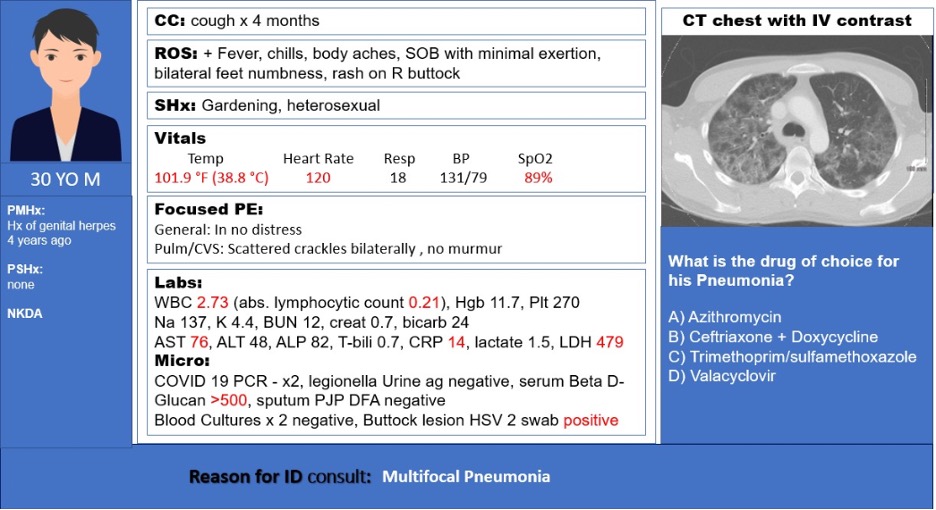 2/ What is the drug of choice for his pneumonia?
2/ What is the drug of choice for his pneumonia?

 There are a four major types of gram-negative resistance mechanisms:
There are a four major types of gram-negative resistance mechanisms:



https://twitter.com/ID_fellows/status/1369719330661949445
 We welcome Rookies (Anyone Pre-ID fellowship), Legends (those post-ID fellowship), and everything in between!
We welcome Rookies (Anyone Pre-ID fellowship), Legends (those post-ID fellowship), and everything in between!


 2/
2/

https://twitter.com/nejm/status/1109141522413428737?lang=en
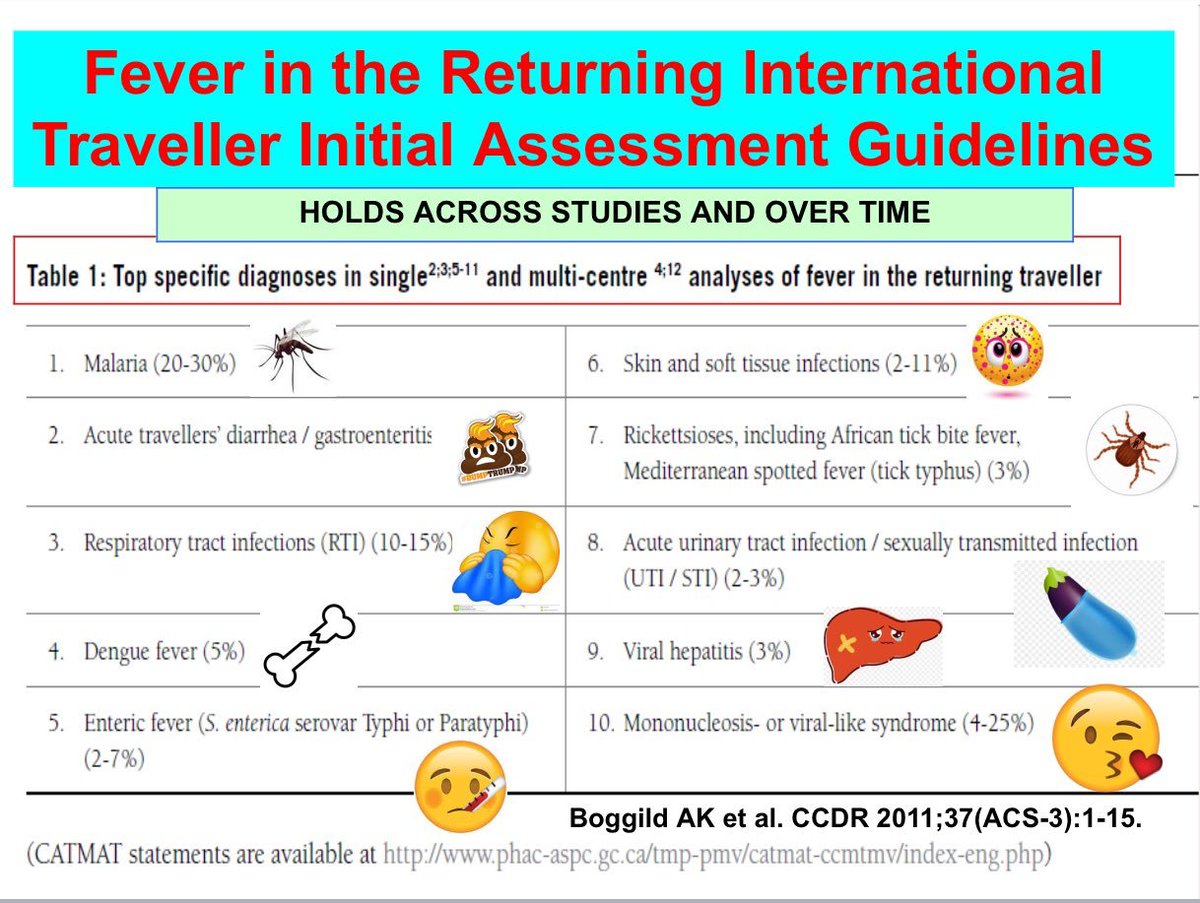
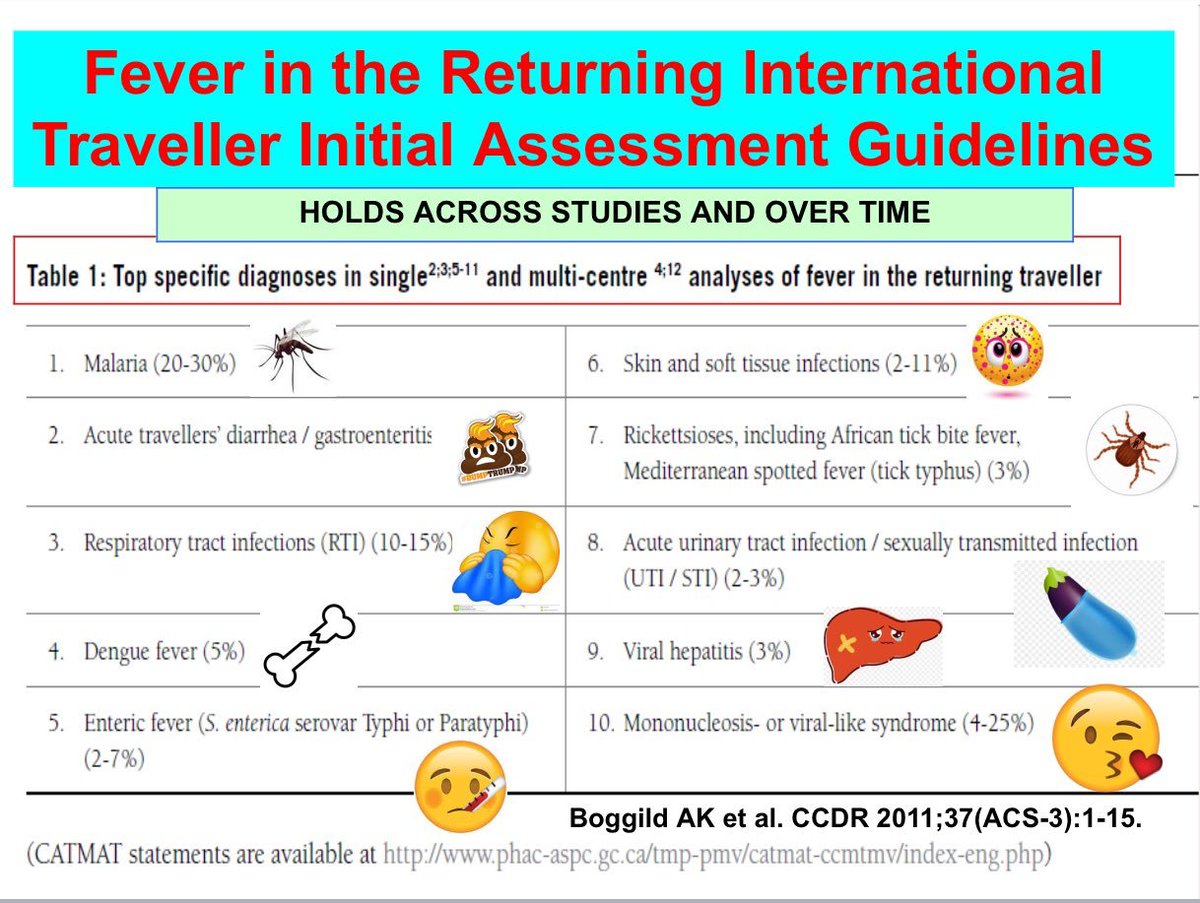
https://twitter.com/BoggildLab/status/1226586319901659137?s=20