
Critical care PA, FCCM, former EMT. Teaches at https://t.co/dhDfHwVfKo, podcasts at https://t.co/1KA4lxqiiO, blogs at https://t.co/Qf4aPrrBRw. #FOAMcc #FOAMed
How to get URL link on X (Twitter) App

https://twitter.com/AlexLawandi/status/1731075400858542490Many people will pin the wire with their off-hand as they dilate (good), and some will periodically wriggle it in and out (okay); it will "catch" on retraction if you're kinking your wire (dilating off-axis) and making an angle at the tip. But too late! It's already kinked.
https://twitter.com/fuzzymittens/status/15604489189570846721. In almost all cases, anesthesiology will be the most-experienced, most-trained people to manage an airway.

 In this case, the Impella is completely decompressing the LV and taking over its output. There is NO pulsatility to the arterial flow — only laminar flow from the Impella. Can you think of any implications of this for the immediate resuscitation?
In this case, the Impella is completely decompressing the LV and taking over its output. There is NO pulsatility to the arterial flow — only laminar flow from the Impella. Can you think of any implications of this for the immediate resuscitation? 


 UW offers free online modules to educate clinicians on performing ECG screening for athletes uwsportscardiology.org/e-academy/ecg-…
UW offers free online modules to educate clinicians on performing ECG screening for athletes uwsportscardiology.org/e-academy/ecg-…

 Double sequential defibrillation may work, but just changing the vector (moving pads) may work as well.
Double sequential defibrillation may work, but just changing the vector (moving pads) may work as well.
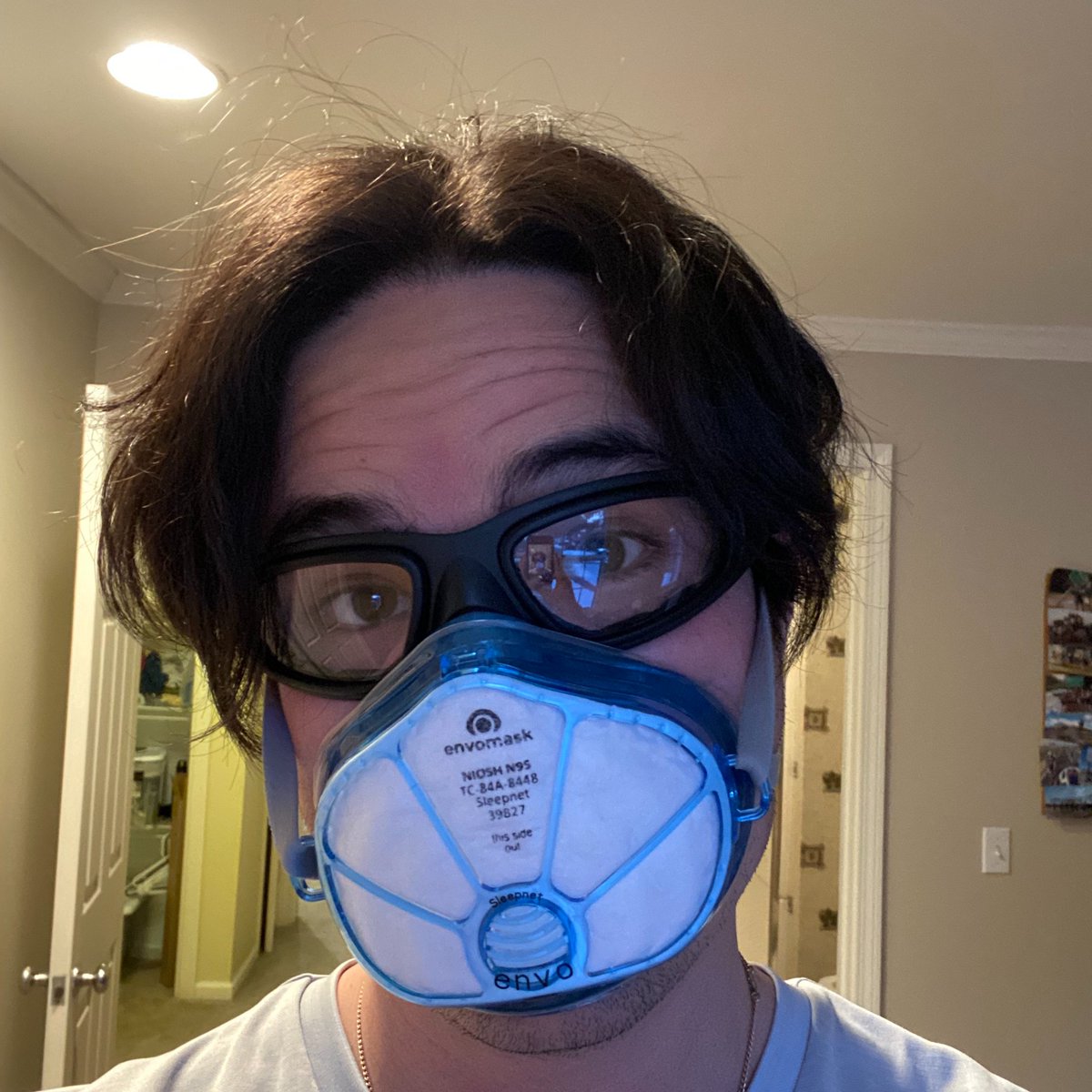
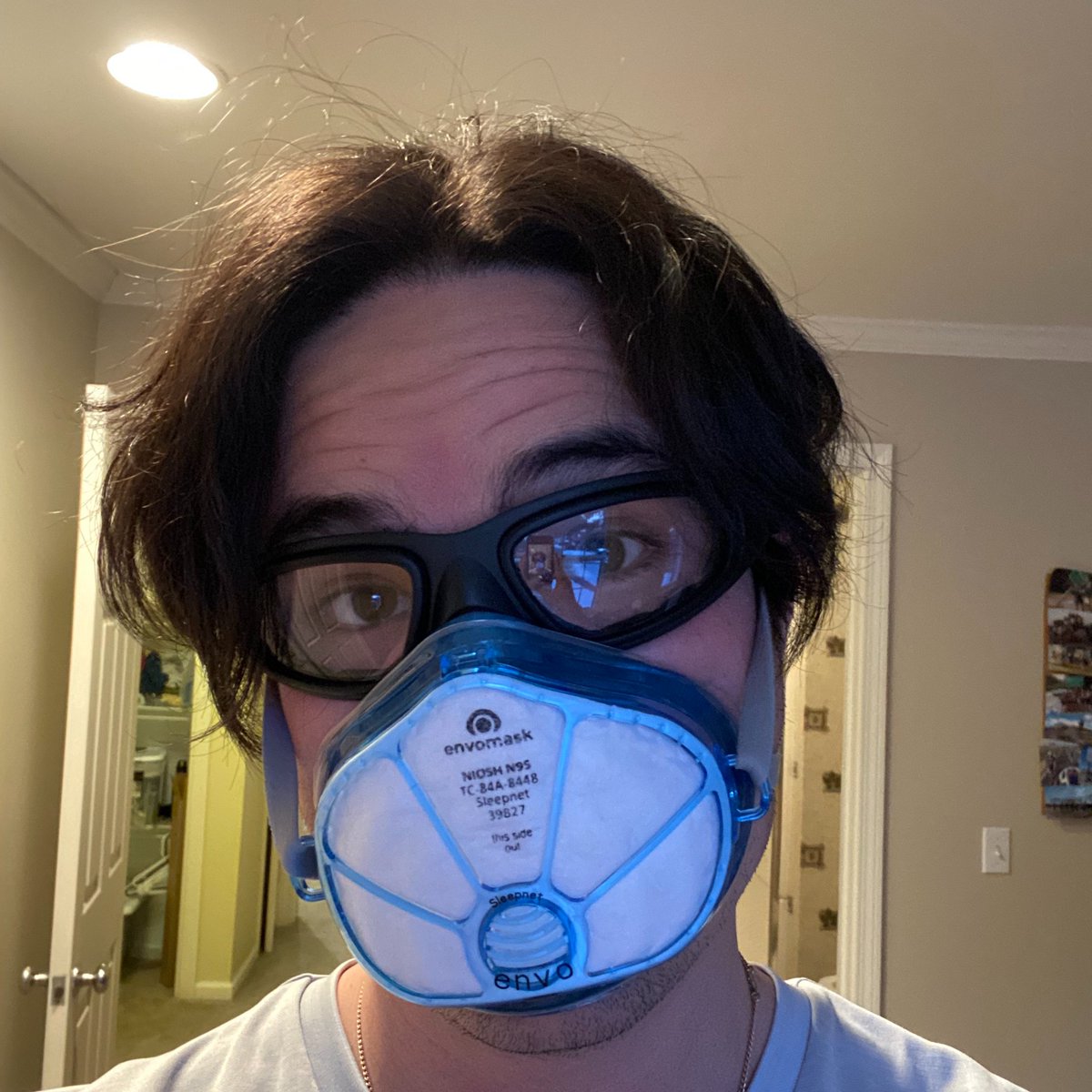 1. The goggles are not 100% sealed and have small vents along the sides. However, I do not think a 100% seal is necessary, and would be an incredible fog-creator. The Wileys are also pricey; consider these, almost as good (amazon.com/gp/product/B00…) but don't seal quite as well.
1. The goggles are not 100% sealed and have small vents along the sides. However, I do not think a 100% seal is necessary, and would be an incredible fog-creator. The Wileys are also pricey; consider these, almost as good (amazon.com/gp/product/B00…) but don't seal quite as well.