Hepatic encephalopathy in the hospital (An ode to #lactulose):
A brief #livertwitter #tweetorial
Aims:
1. Share the greatest t-shirt ever made
2. Rule out infection!
3. Laxation now! But how?
keywords: #cirrhosis, paracentesis, stool pH
A brief #livertwitter #tweetorial
Aims:
1. Share the greatest t-shirt ever made
2. Rule out infection!
3. Laxation now! But how?
keywords: #cirrhosis, paracentesis, stool pH
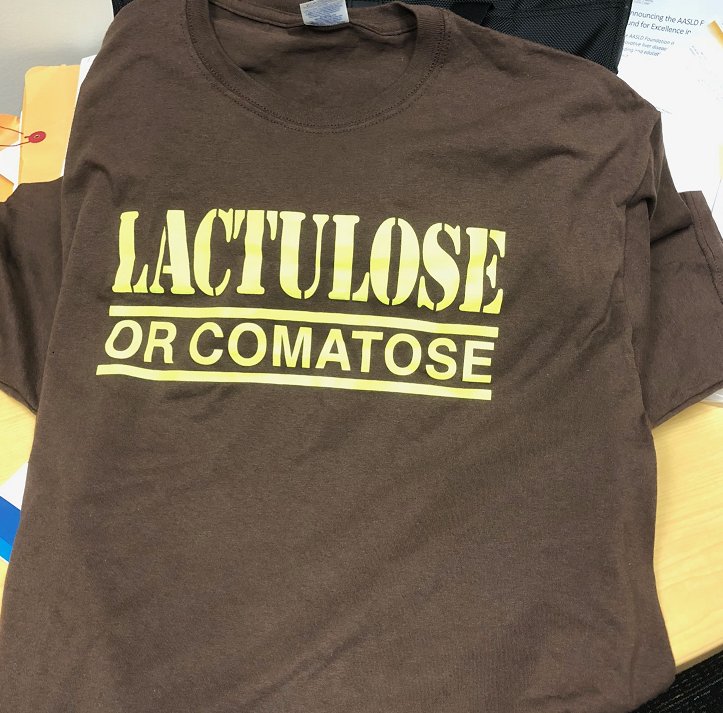
1. This shirt, made by a patient, reminds us:
▶️HE is horrible, unpredictable
▶️Preventing HE is hard
▶️Dont be quick 2 label pts as 'noncompliant' - there's more to the story
▶️Our patients are awesome. Hepatology is the best
#lactuloseorcomatose
▶️HE is horrible, unpredictable
▶️Preventing HE is hard
▶️Dont be quick 2 label pts as 'noncompliant' - there's more to the story
▶️Our patients are awesome. Hepatology is the best
#lactuloseorcomatose
2. Think of hepatic encephalopathy as a biomarker.
For what? The answers form a mandatory checklist of sorts
1. Para to r/o SBP. Delay @ your patient's peril. (Fig1)
2. GI Bleeding?
3. UA/Blood Cultures/CXR
3. What's the Cr? Na? K?
review: nature.com/articles/s4139…
#AmJGastro
For what? The answers form a mandatory checklist of sorts
1. Para to r/o SBP. Delay @ your patient's peril. (Fig1)
2. GI Bleeding?
3. UA/Blood Cultures/CXR
3. What's the Cr? Na? K?
review: nature.com/articles/s4139…
#AmJGastro
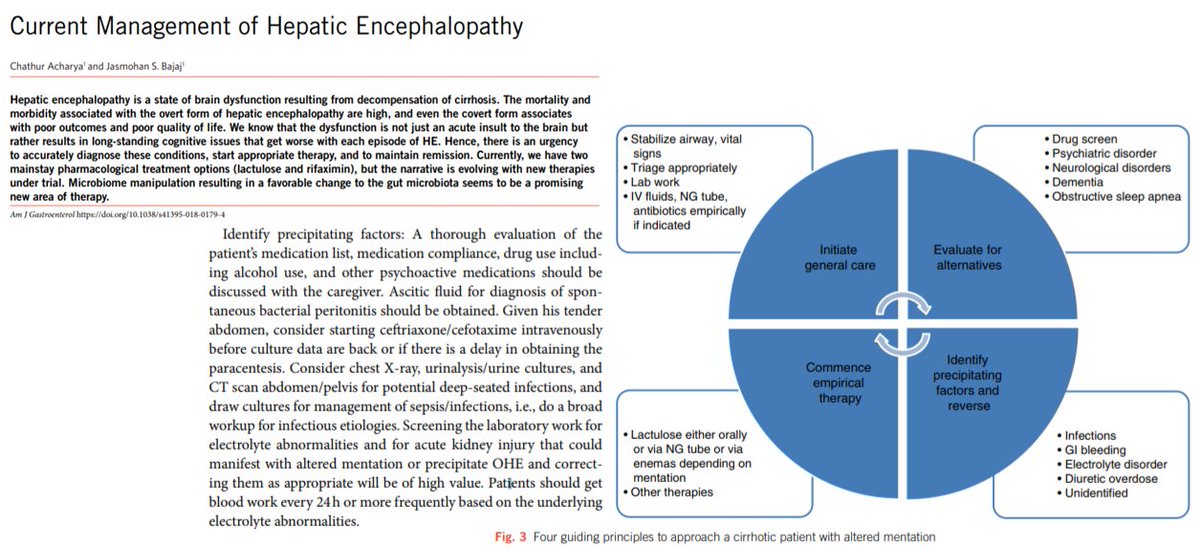
3. First line therapy for hospitalized "overt" HE is lactulose
This nonabsorbable disaccharide has been used for HE for >50 years. (Fig1)
It was known even then that there had to be another mode of action beyond frequent BMs

This nonabsorbable disaccharide has been used for HE for >50 years. (Fig1)
It was known even then that there had to be another mode of action beyond frequent BMs

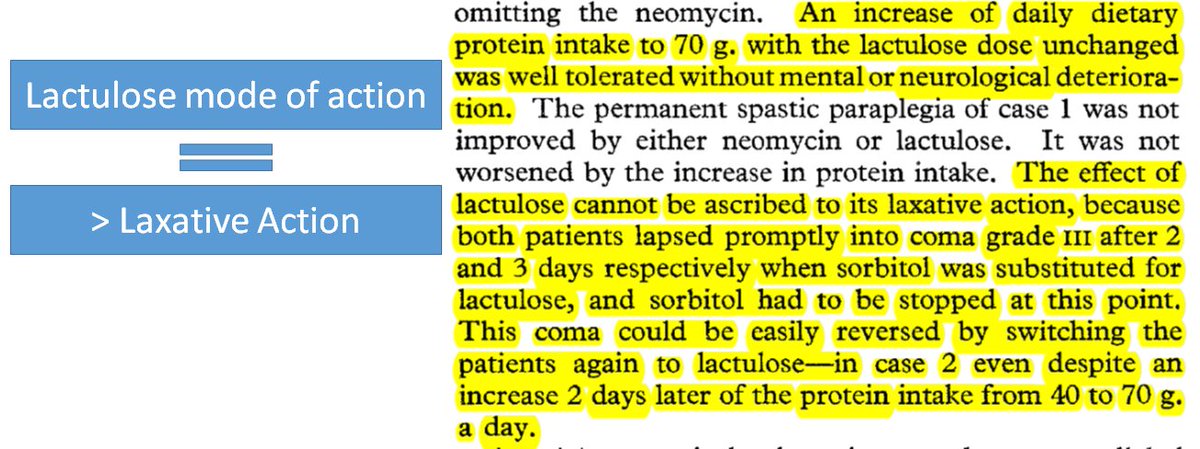
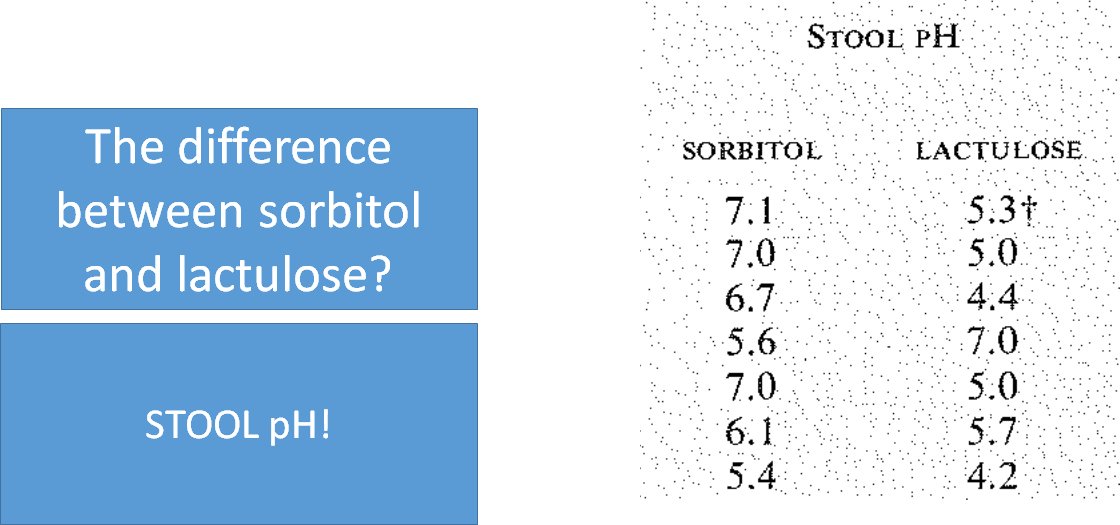
Lactulose's mechanism of action came into focus after a 1966 trial in patients w/chronic HE
Fig1: Design - lactulose before or after sorbitol (osmotic laxative) with run-in
Fig2: HE that occurred on sorbitol could be resolved on lactulose
Fig3: The key difference: STOOL PH!


Fig1: Design - lactulose before or after sorbitol (osmotic laxative) with run-in
Fig2: HE that occurred on sorbitol could be resolved on lactulose
Fig3: The key difference: STOOL PH!


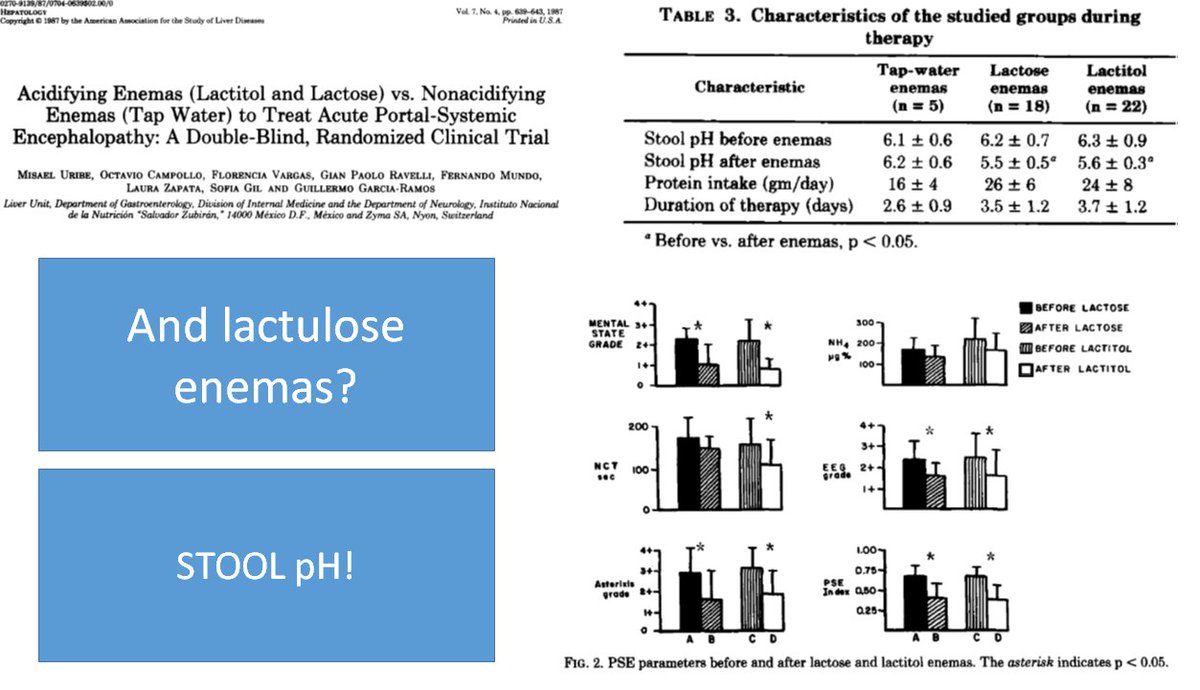
The same effect occurs after a lactulose enema.
See these data from a randomized trial of tap water vs lactulose enema in @HEP_Journal
ncbi.nlm.nih.gov/pubmed/3301614
See these data from a randomized trial of tap water vs lactulose enema in @HEP_Journal
ncbi.nlm.nih.gov/pubmed/3301614
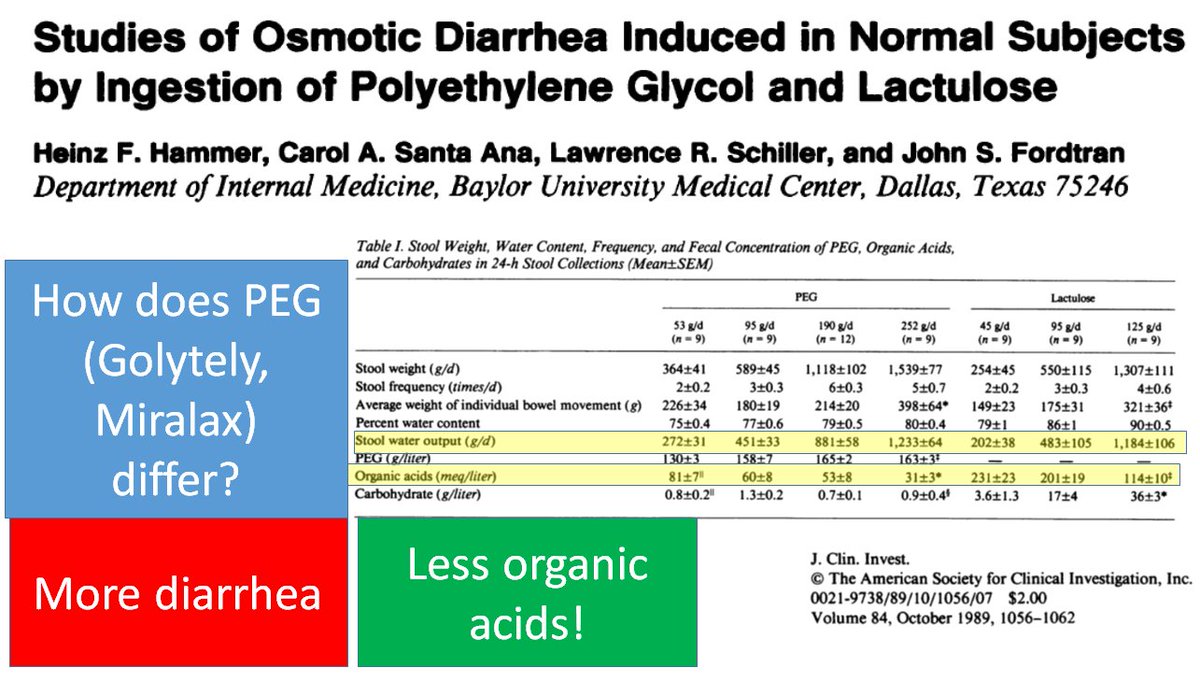
How does lactulose lower stool pH?
The answer is that colonic bacteria metabolize the lactulose, spitting out organic acids
Check out this study from @jclinicalinvest comparing the stool output and organic acid concentration after PEG (aka golytely) vs lactulose
The answer is that colonic bacteria metabolize the lactulose, spitting out organic acids
Check out this study from @jclinicalinvest comparing the stool output and organic acid concentration after PEG (aka golytely) vs lactulose
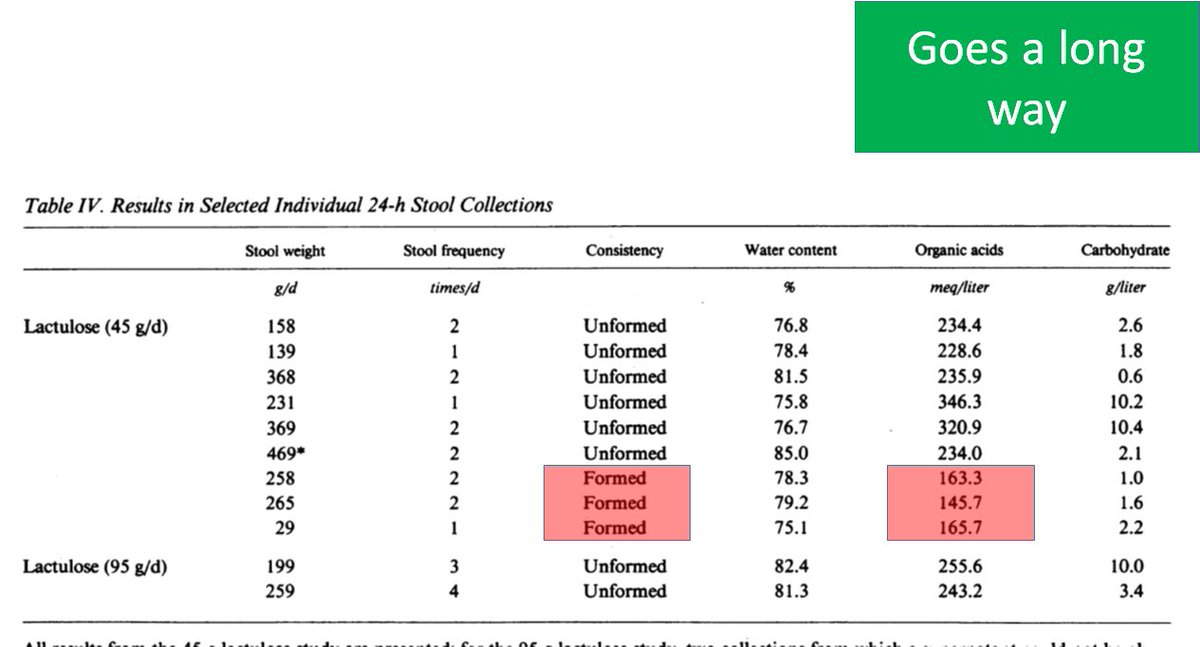
And here is the kicker: A little lactulose goes a long way
Even in subjects who had formed stool, lactulose still increased the organic acid concentration!
ncbi.nlm.nih.gov/pubmed/2794043
Even in subjects who had formed stool, lactulose still increased the organic acid concentration!
ncbi.nlm.nih.gov/pubmed/2794043
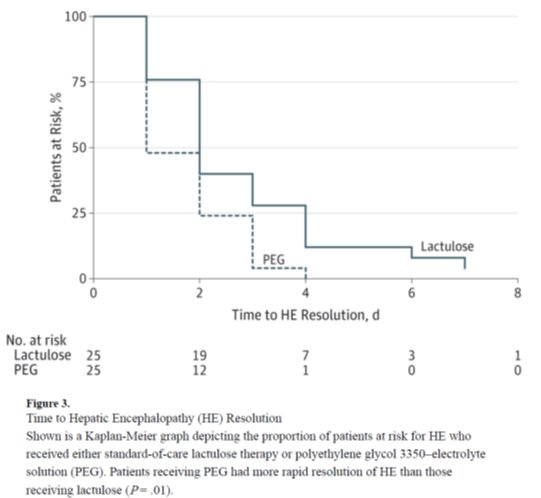
🥊 PEG vs Lactulose 🥊 The HELP RCT
ncbi.nlm.nih.gov/pubmed/25243839
This remarkable study was led by Dr. Bob Rahimi - who, as a FELLOW, enrolled 50 patients who often present in the middle of the night! #hustle
Lactulose (20-30grams TID) vs PEG Colonoscopy prep (4L)
Who wins?

ncbi.nlm.nih.gov/pubmed/25243839
This remarkable study was led by Dr. Bob Rahimi - who, as a FELLOW, enrolled 50 patients who often present in the middle of the night! #hustle
Lactulose (20-30grams TID) vs PEG Colonoscopy prep (4L)
Who wins?
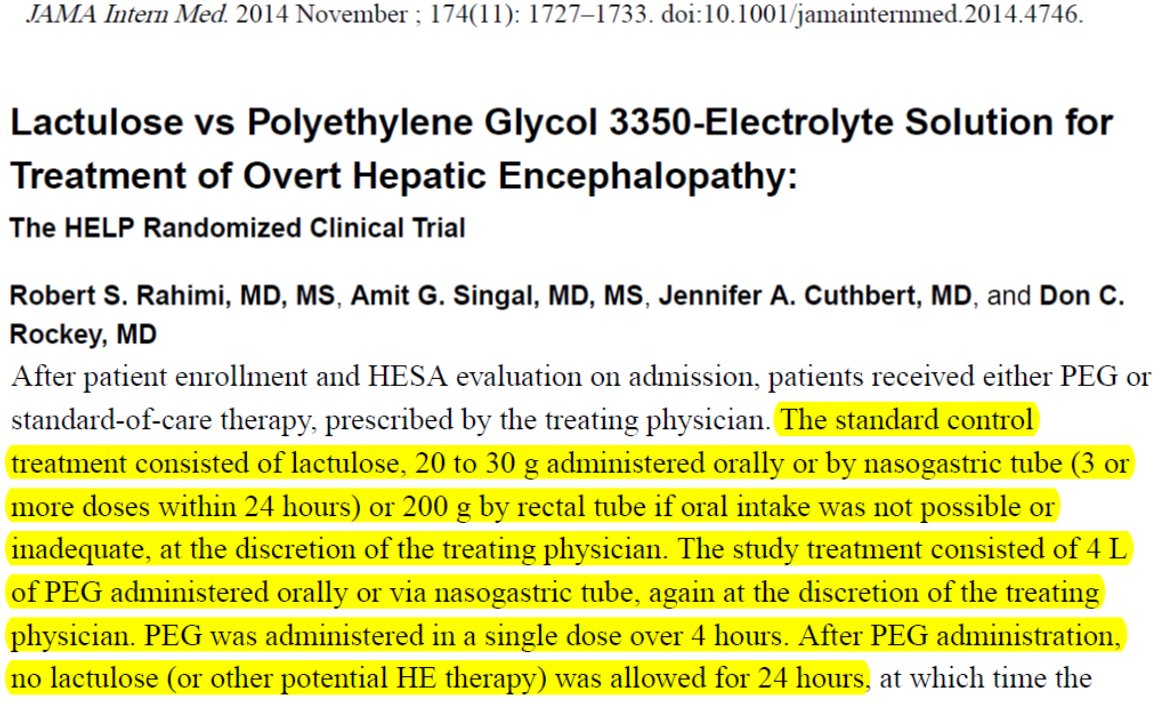
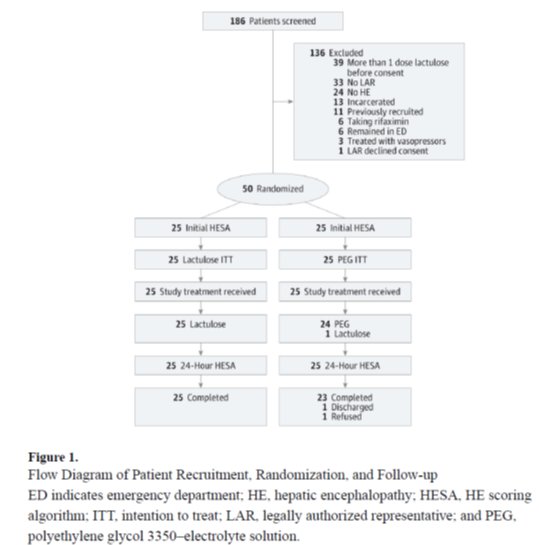
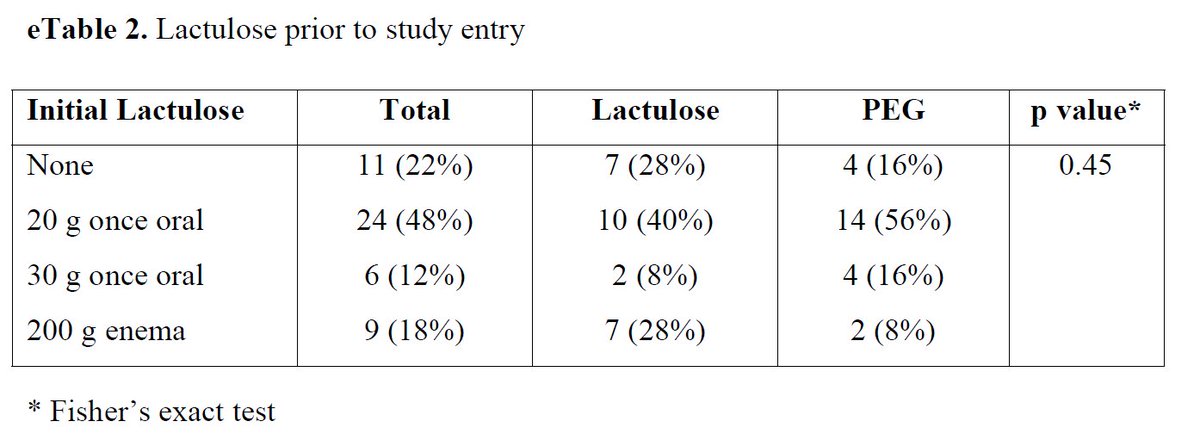
But...
Before you pop the cork on the Golytely, check out the supplement(Fig1):
84% of PEG patients got lactulose before randomization
CLEARLY you need 2 get the bowels moving (more laxative=better)
but a little lactulose goes a long way. Stool pH not measured.
Before you pop the cork on the Golytely, check out the supplement(Fig1):
84% of PEG patients got lactulose before randomization
CLEARLY you need 2 get the bowels moving (more laxative=better)
but a little lactulose goes a long way. Stool pH not measured.
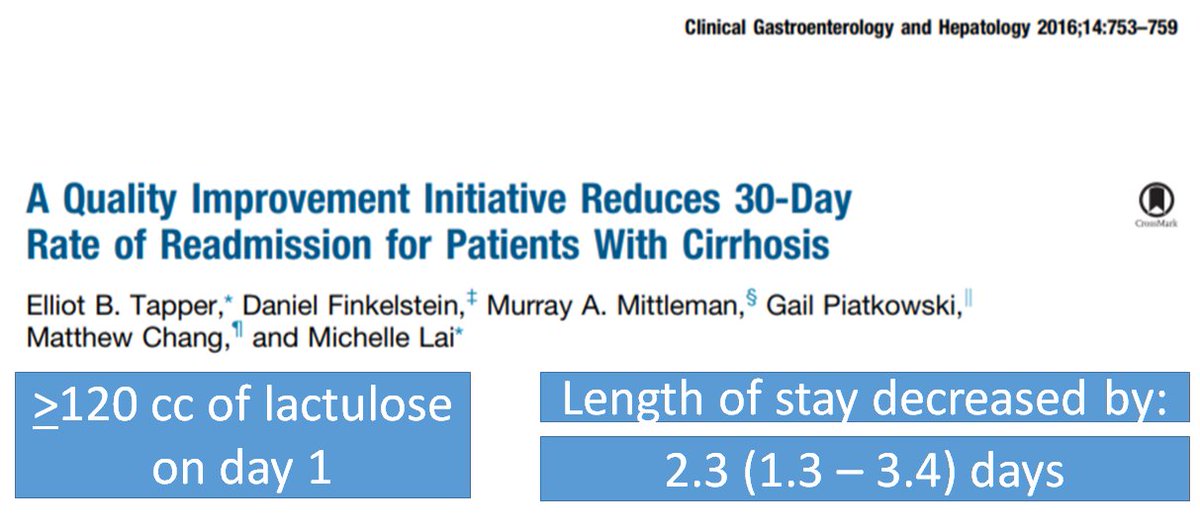
Also...what's the right dose of lactulose?
When a pt comes in with acute CHF, would we give them their home diuretic dose?
Patients admitted with HE often get ~10-20cc TID
🔥Hot take 🔥 This is not enough: That is a maintenance dose
Your pt needs an induction dose!
When a pt comes in with acute CHF, would we give them their home diuretic dose?
Patients admitted with HE often get ~10-20cc TID
🔥Hot take 🔥 This is not enough: That is a maintenance dose
Your pt needs an induction dose!
Unlike with PEG, you dont need 4 liters, but >20cc lactulose q6-8? Definitely!
I learned how 2 treat HE from nurses when I was an intern. We took what they were doing & standardized treatment for HE. Some extra, frequent doses make a big difference(Fig1)
cghjournal.org/article/S1542-…
I learned how 2 treat HE from nurses when I was an intern. We took what they were doing & standardized treatment for HE. Some extra, frequent doses make a big difference(Fig1)
cghjournal.org/article/S1542-…
In summary:
- Hepatology = the best
- Do that para! Search 4 HE triggers
- Drop that stool pH! Even a little lactulose helps
- Laxation now!! Need frequent BMs on Day 0-1 to treat Overt HE. Take your pick: extra doses of lactulose or lactulose + PEG.
Thanks for stopping by!
- Hepatology = the best
- Do that para! Search 4 HE triggers
- Drop that stool pH! Even a little lactulose helps
- Laxation now!! Need frequent BMs on Day 0-1 to treat Overt HE. Take your pick: extra doses of lactulose or lactulose + PEG.
Thanks for stopping by!
• • •
Missing some Tweet in this thread? You can try to
force a refresh