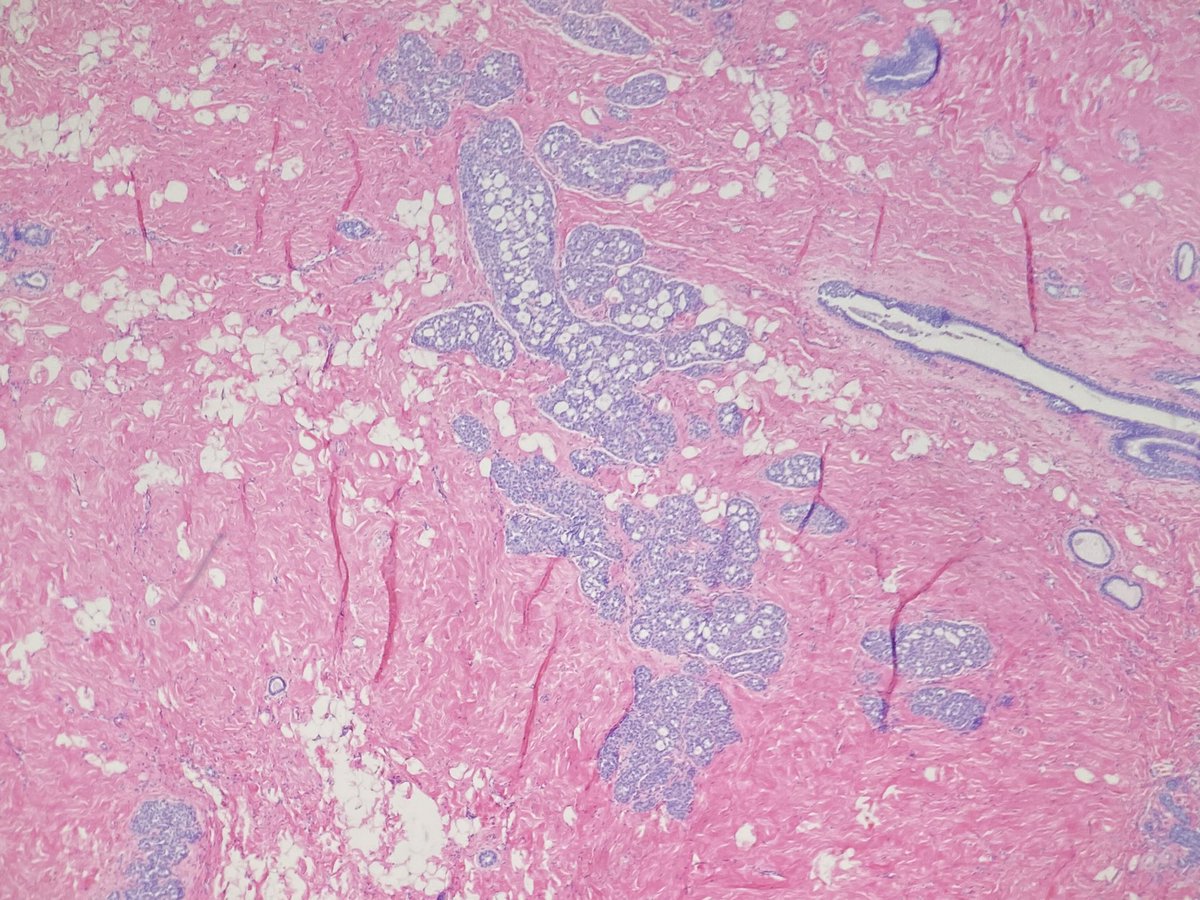
Breast biopsy for calcs. What is your diagnosis? Would you do stains? Since I’m asking that means I did 😉🔬 #breastpath @BIDMCpath @CollinsLauraC @jennpincus @RanaAldreesMD @tlabiano @lara_pijuan @ADamronMD @ariella8 @kis_lorand @TheISBP 







Thanks for all the comments! Here are the stain. All (including p120, not pictured) were consistent with a lobular phenotype. 



This is a nice example of florid LCIS with comedo necrosis and associated calcifications. The nuclei aren't pleomorphic enough for me to call PLCIS; I would classify these are type B cells. Exc was recommended and showed more florid and classical LCIS with no invasive component.
We have limited info on the natural history of PLCIS and FLCIS. Per the who 25-60% of cases on core are upgraded to carcinoma on exc therefore exc is recommended.
Here is an example of PLCIS with associated invasive lobular I had a couple years ago.
https://twitter.com/LizaMQuintana/status/959528557331582976
• • •
Missing some Tweet in this thread? You can try to
force a refresh