A #TWEETORIAL summary of the Fleischner Society consensus statement @Radiology_RSNA: doi.org/10.1148/radiol…
Podcast: doi.org/10.1148/radiol…
#RadsInTraining
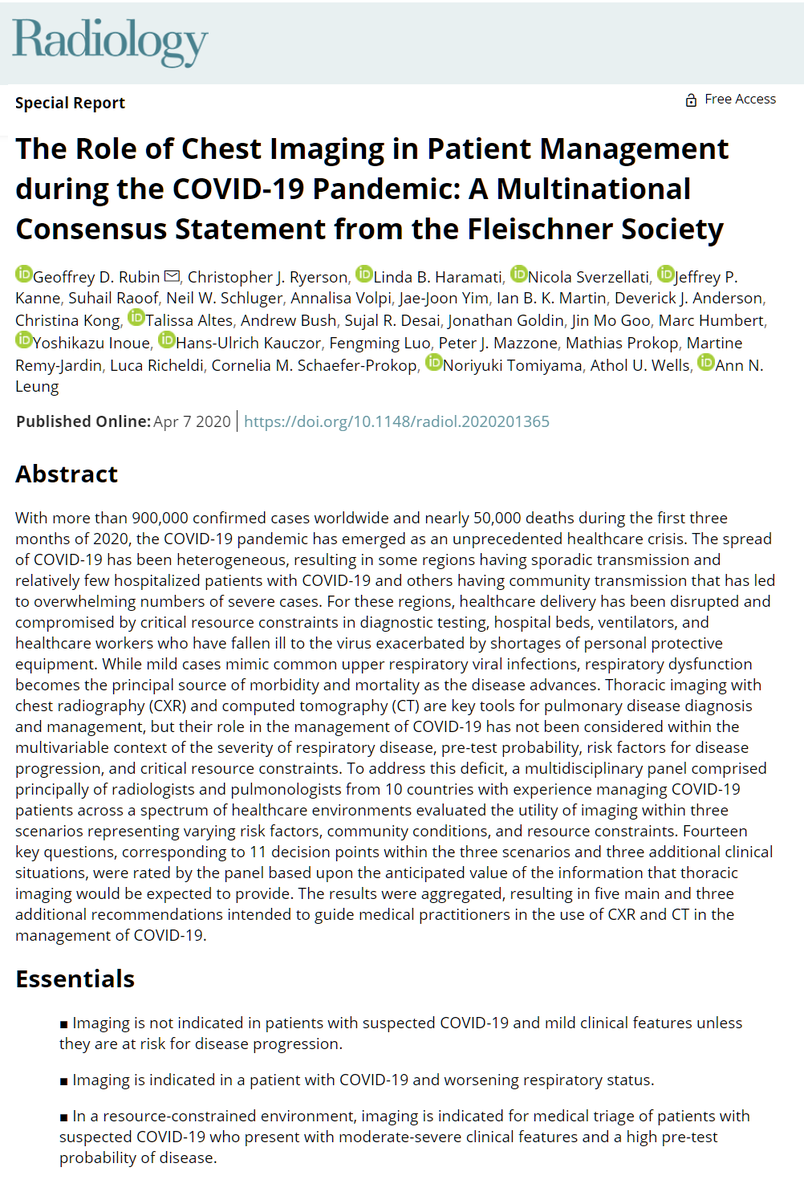
A) RT-PCR unavailable, age/comorbidity risk factors for severe disease present
B) Positive RT-PCR, no risk factors for severe disease
C) Negative RT-PCR, mild symptoms persisting 5 days
Step 3: identify risk factors for progression if pt has COVID, like
-age >65
-diabetes
-cardiovascular disease, eg hypertension
-chronic respiratory disease, eg COPD
-immunocompromise
A) Positive RT-PCR only
B) Unavailable RT-PCR only
C) Either positive, negative, or unavailable RT-PCR
A) COVID-19 test positive, initial presentation, moderate
B) COVID-19 test positive, clinical worsening in hospital
C) COVID-19 test delayed, emergency dept patient
(Case @derekrad rID: 75249)

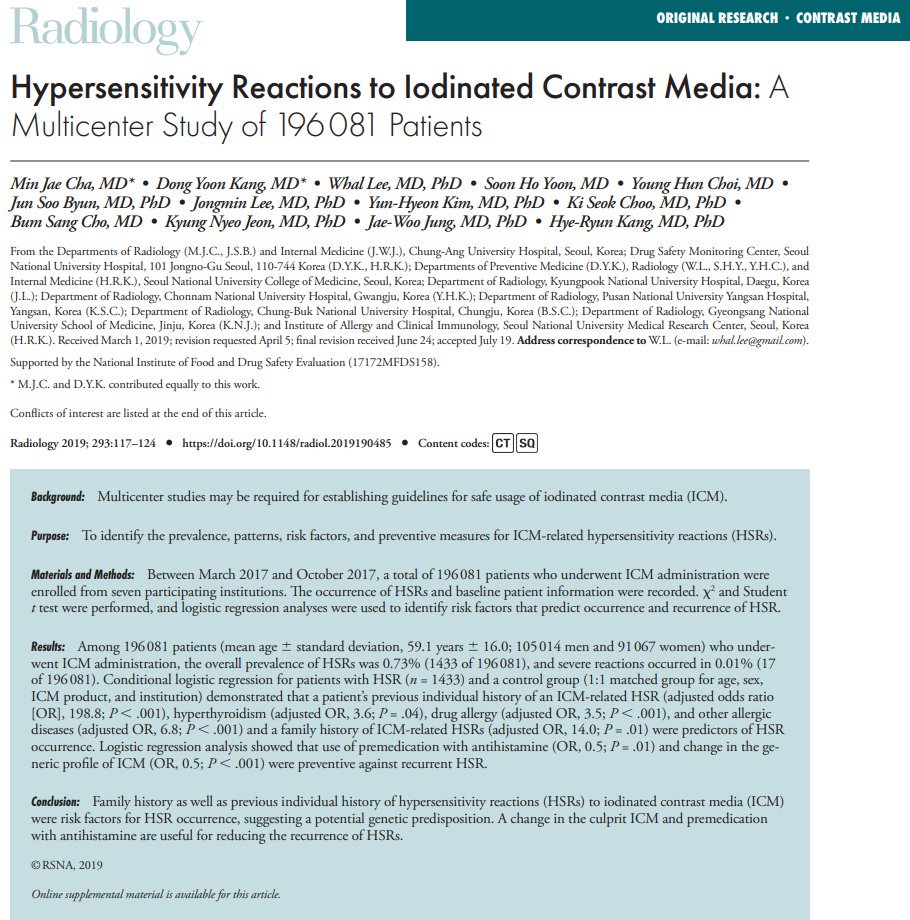
Should my patient with COVID-19 get CXR or CT?
CT is more sensitive for early disease, progression, and alternative diagnoses. However, portable CXR may be good enough or preferred considering local resource constraints/infection control measures. No strong recs
No. CXRs should be on-demand for clinical changes. Help limit exposure to rad techs and conserve PPE.
YES. Distinguish expected sequelae of infection/ARDS from alternative potentially treatable diagnoses.