A #TWEETORIAL for #radres and referring clinicians alike
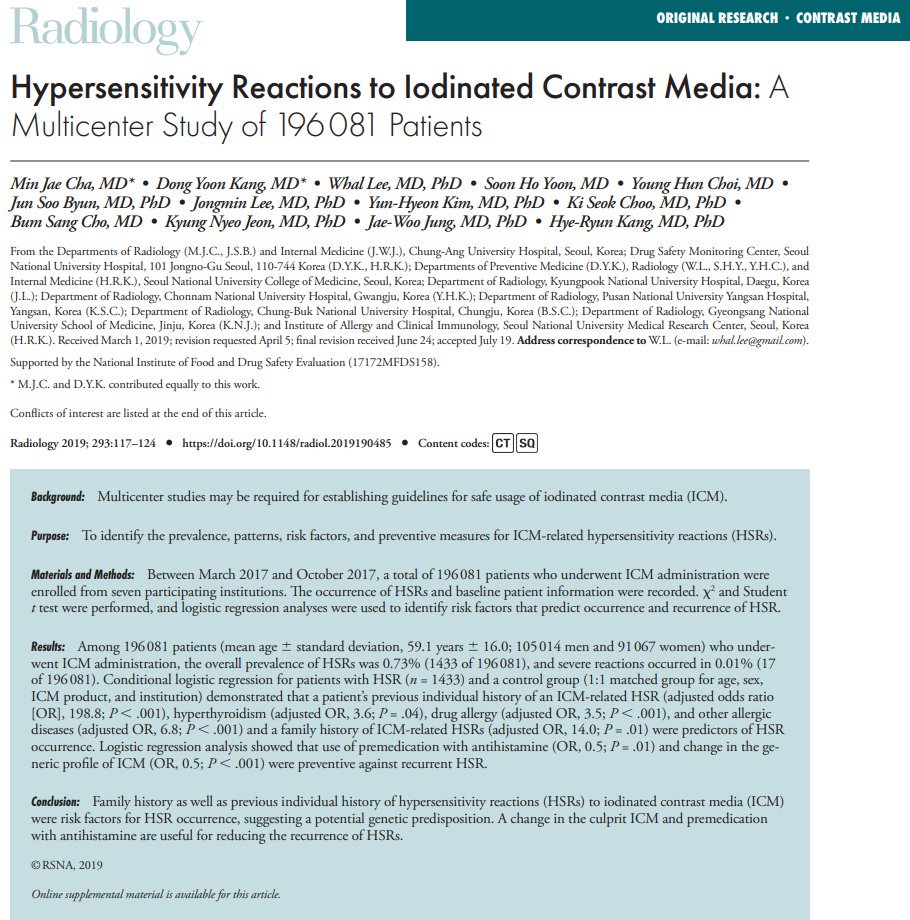
Inspired by a recent paper in @Radiology_RSNA by Cha MJ, Kang DY, et al. pubs.rsna.org/doi/10.1148/ra… 1/40ish
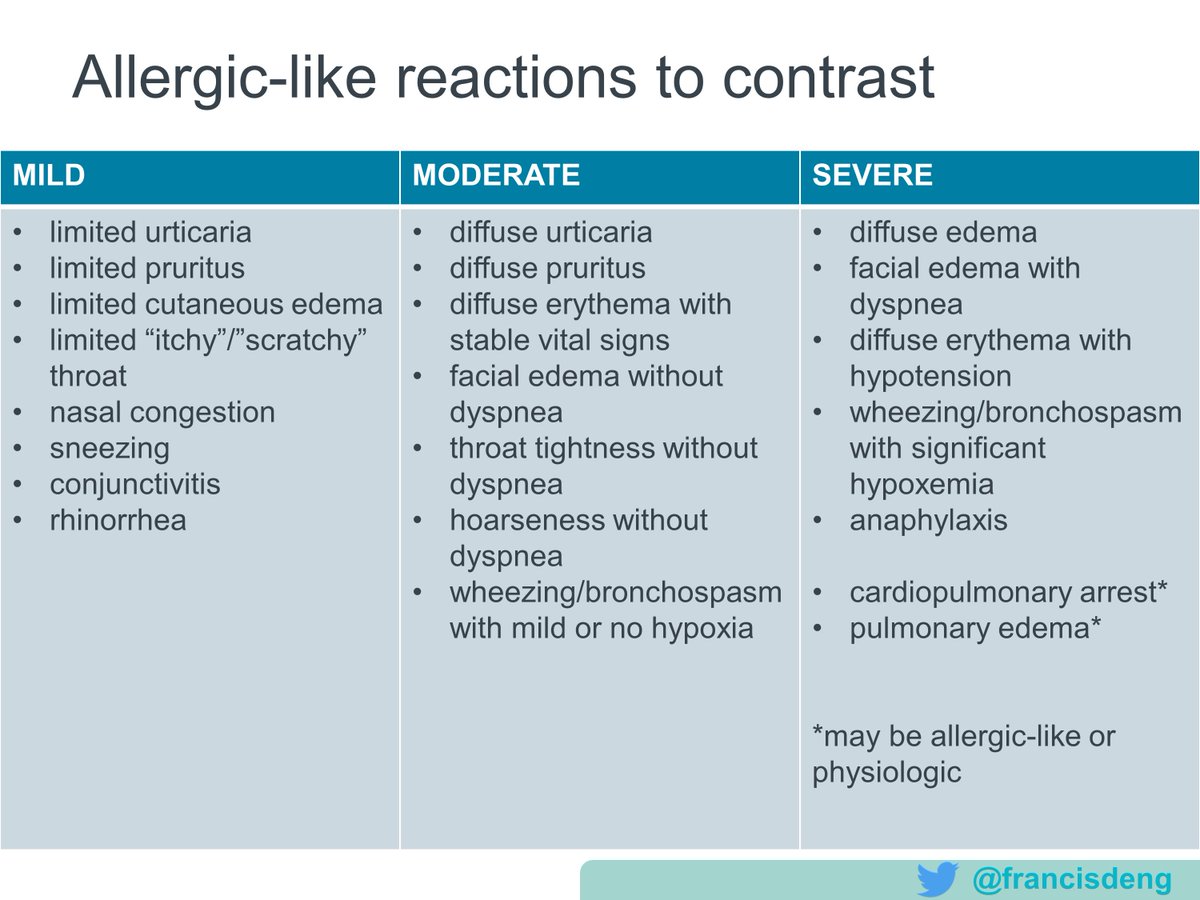
DEFINING ALLERGIC-LIKE REACTIONS
Which of the following is most likely to represent an allergic-like contrast reaction?
Mild: self-limited
Moderate: commonly requiring treatment
Severe: life-threatening
Here is a list of physiologic reactions.
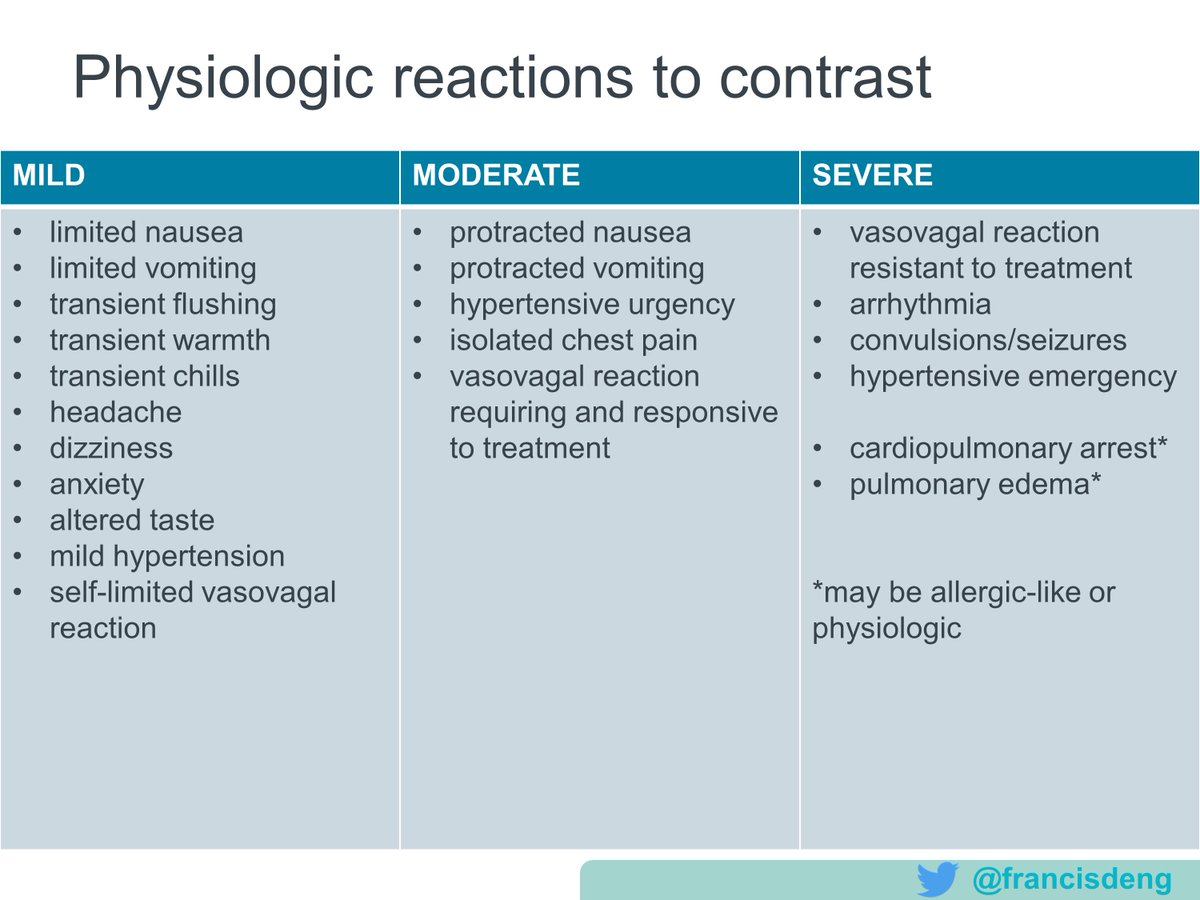
1) Patients with allergic-like reactions may require/benefit from premedication prior to future exposures, while those with physiologic reactions do not.
When do these reactions occur?
Nearly all life-threatening reactions happen immediately, within 20 minutes of contrast administration.
Which contrast agents are we talking about?
These days we use nonionic, tri-iodinated benzene rings with three variable side chains, in solutions that are 1-3x serum osmolality (called "low osmolality").
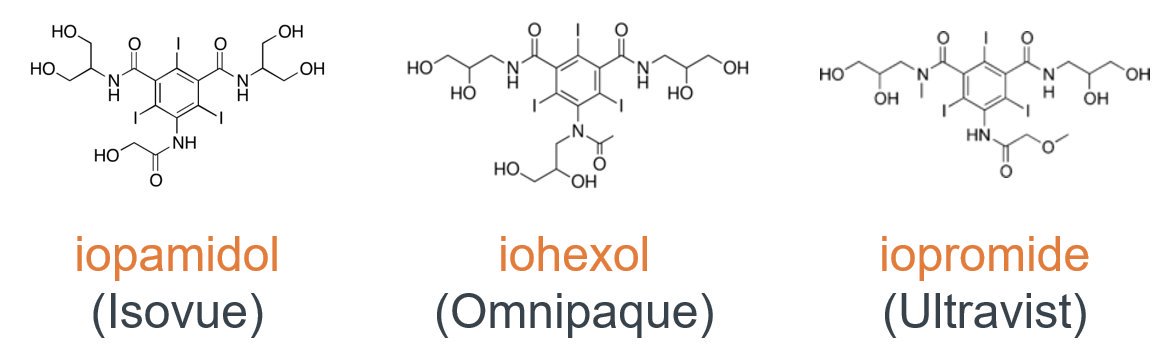
iopamidol
iopromide
iohexol
ioversol
io𝘥𝘪xanol (a 𝘥𝘪mer and iso-osmolal)
ioxilan
iobitridol
iomeprol
TRIVIA: Which of these is an iodinated contrast agent brand name (included in this paper)?
The point is, brand names are hard. In contrast (get it?), the generic names for current intravascular iodinated agents all start with "io-"!


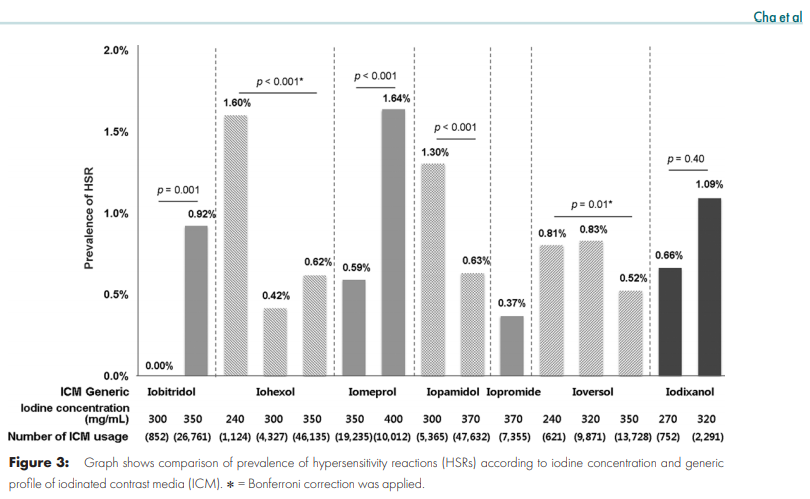
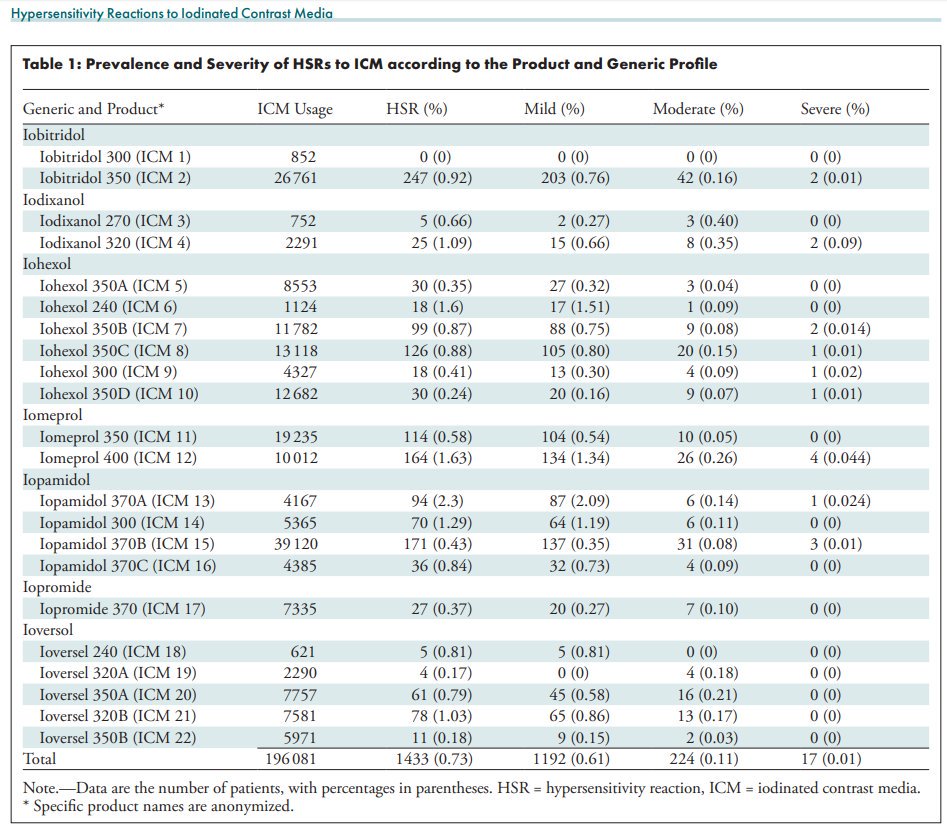
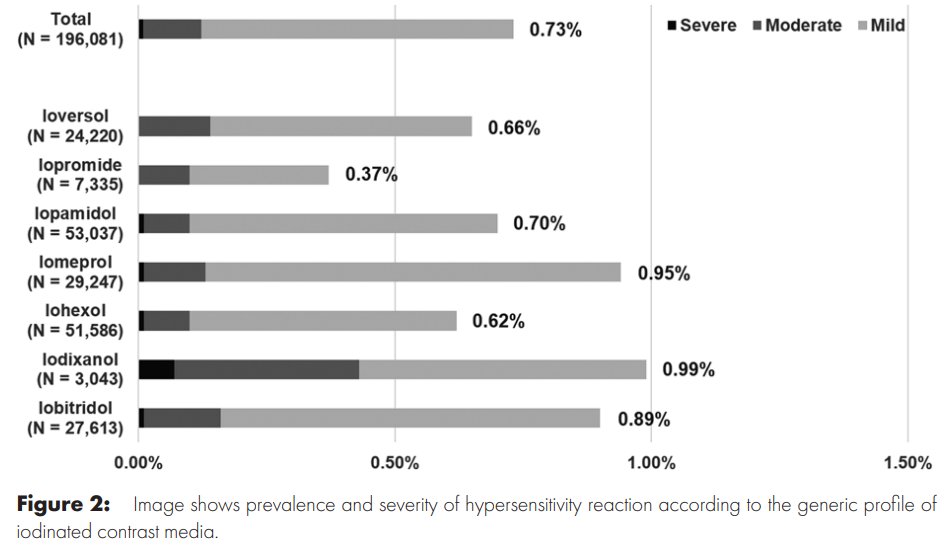
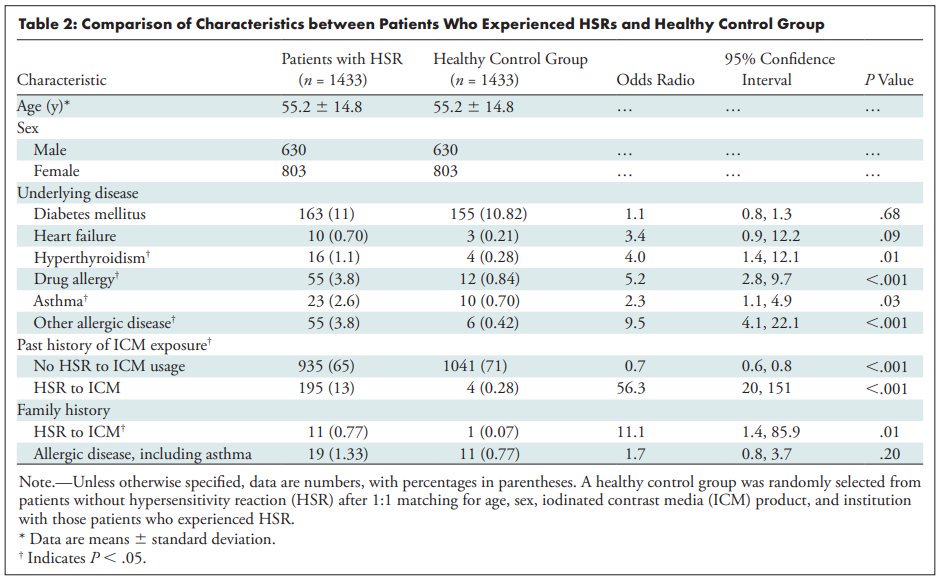
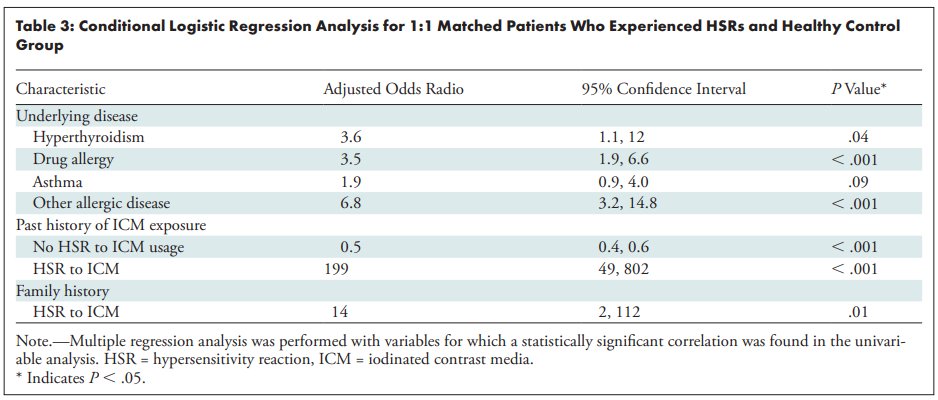
Cha et al. studied a registry of 196,081 patients who had contrast-enhanced CT at 7 institutions in Korea over 8 months. Here's some rounded figures based on this and other papers, which triangulate the teaching points.
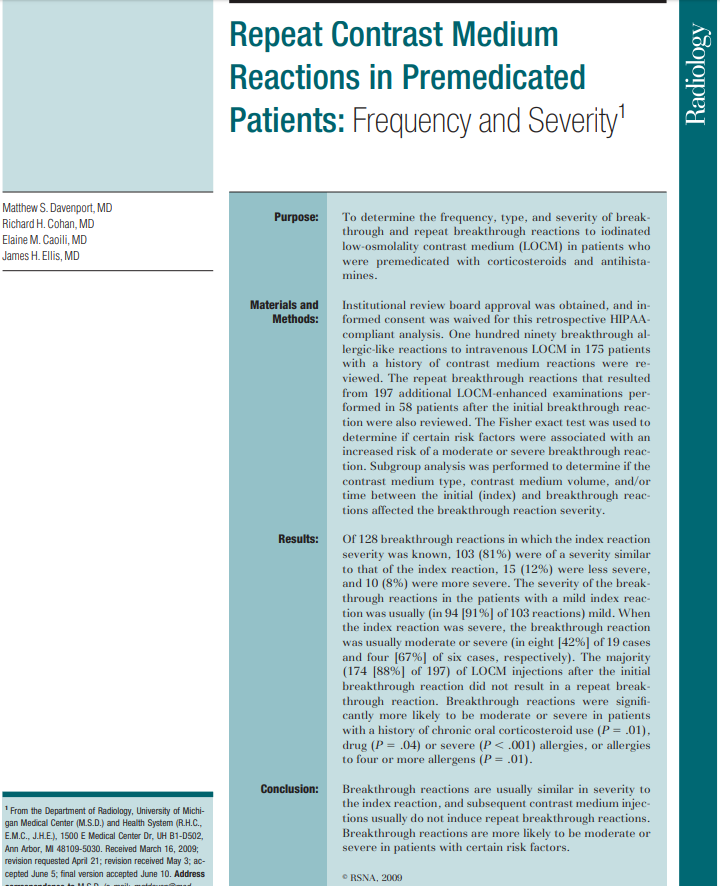
See Davenport et al. in Radiology 2009 dx.doi.org/10.1148/radiol…
See doi.org/10.1016/j.jaip…
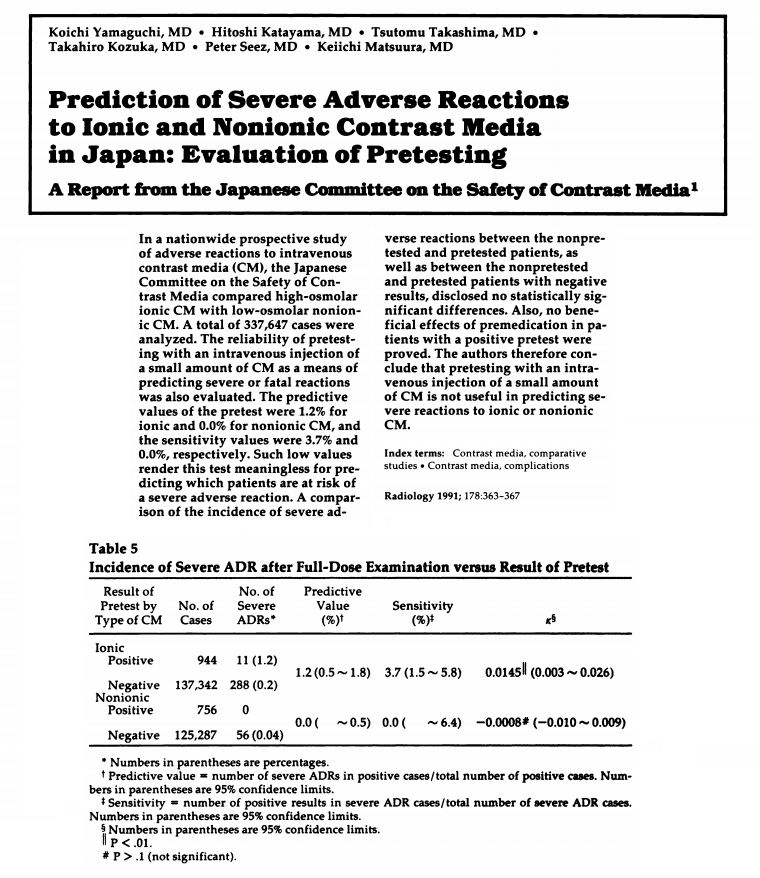
See Yamaguchi et al. Radiology 1991 doi.org/10.1148/radiol…
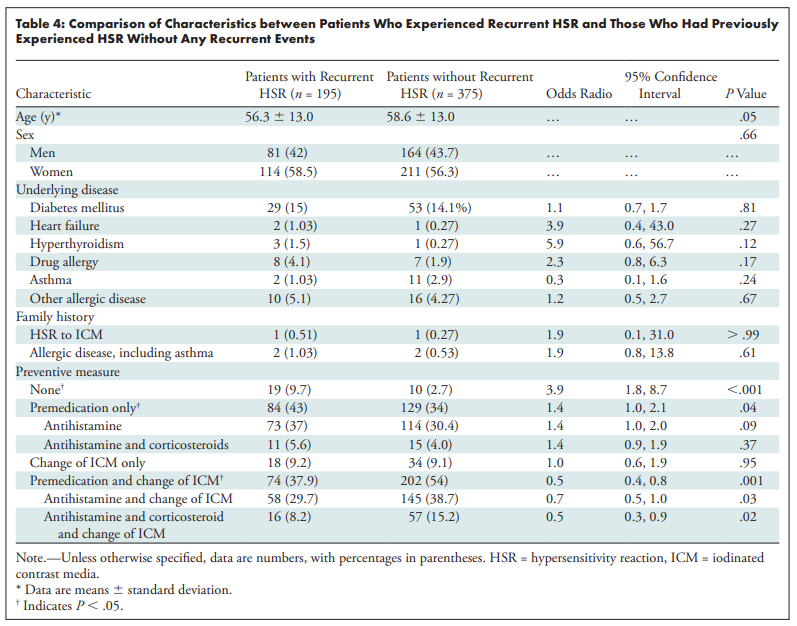
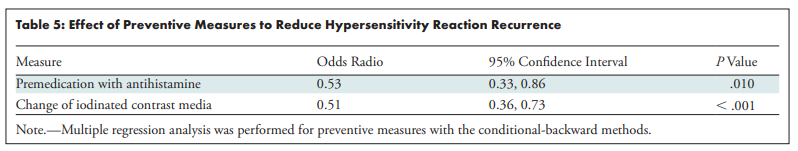
In patients who had an allergic-like reaction to iodinated contrast, there are three preventive measures to consider prior to another exam:
1) Avoidance
2) Premedication
3) Agent switching
This is why contrast names are important. If you know the culprit agent, don't pick the general entry your EHR offers like "Iodinated Contrast- Oral and Iv Dye".
Pt with hx hives+hypoxia+hypotension after iopamidol; needs CT in ED: ?appendicitis. What's most reasonable:
A)CT now w rectal diatrizoate, IV iopamidol
B)CT now w rectal barium, w/o IV
C)5h premed, CT w rectal+IV diatrizoate
D)13h premed, CT w rectal barium, IV ioversol
Elderly inpt w remote hx of "feeling hot" and "throwing up" following "IVP dye" in 1980. CT needed: ?acute PE. What do you do before CT pulm angio?
A) Test injection (small IV dose)
B) 13h premedication regimen
C) Allergy consult: ?skin testing
D) Nothing special
Pt has throat scratchiness + sneezing 15 min after 90 mL IV iopamidol 370 mg iodine/mL. Sx resolve spontaneously within 15 min. What allergy entry do you add?
A)Iopamidol
B)Iodinated Contrast- Oral and Iv Dye
C)Iodine and Iodine-containing Substances
D)None
In the same patient as above, which of the following is the best severity of reaction to document?
Case 1: The patient had a severe allergic-like reaction, a relative contraindication to reexposure to iodinated contrast. An alternative technique without iodinated contrast (B) (or US or MR) is appropriate and avoids diagnostic delay and risk of breakthrough reaction.
A) Without premedication or agent switching, there is an unacceptable risk of recurrent reaction -- first, do no harm.
D) With a long premedication regimen, the delay in diagnosis increases the risks of appendicitis complications (but balance varies by scenario)
C) An aggressive clinician and patient might accept the risk of breakthrough reaction despite prior severe reaction (depends on local standards) but I tipped the scale: diatrizoate (Gastrografin) shouldn't be administered IV due to higher risk of adverse reactions.
The patient most likely had a mild physiologic reaction to a high osmolality contrast agent. They would not be regarded as high risk for allergic-like reaction to low osmolality contrast. No special preventive action is needed (D), avoiding diagnostic delay.
A) The use of test injections is not evidence-based.
B) A full premedication regimen would only be indicated for prior allergic-like reaction and if the diagnosis does not need to be made on an emergency basis.
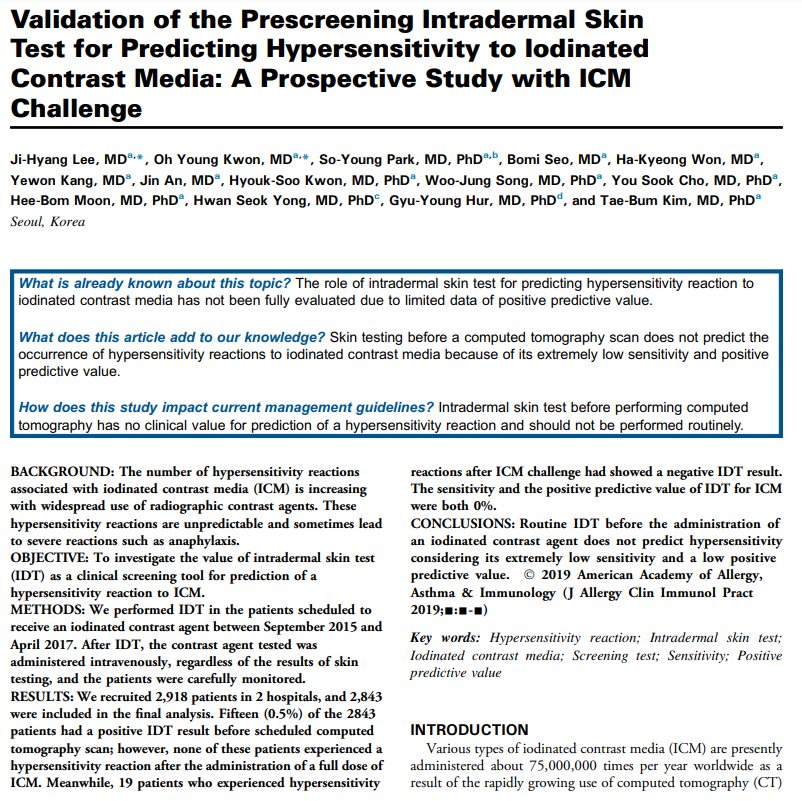
C) An allergist might help you sort out the story to see if it seemed allergic-like, but skin testing for contrast media is not currently an evidence-based practice
My assessment is that the patient had a mild, self-limited allergic-like reaction to iodinated contrast. The culprit and reaction should be documented in detail, including the name of the agent when it is known.
Case 3A: answer is A
Case 3B: answer is A
Maybe in a future tweetorial, we'll dive into the evidence on premedication + agent-switching. How much benefit? What's the risk of breakthrough?