A lot of discussion recently about transmission dynamics, most of which are extrapolated from viral loads & estimates. What does contact tracing/community testing data tell us about actual probability of #COVID19 transmission(infection rate), high risk environments/age?
[thread]
[thread]
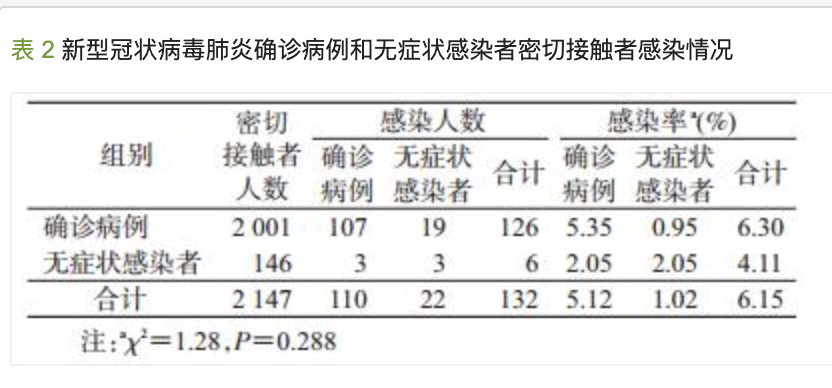
1/ 2147 close contacts of 157 #COVID19 cases were followed up: Overall infection rate was 6%, higher infection rate among friends (22%) and household (18%), and main risk factors include contact in household (13%), transport (11%), dining (7%).
html.rhhz.net/zhlxbx/028.htm (4/3/20)
html.rhhz.net/zhlxbx/028.htm (4/3/20)
2/ 445 close contacts of 10 #COVID19 cases were followed up, of those 54 (12%) developed symptoms, suggesting secondary attack rate of 0.45%, household attack rate of 10.5%. No other close contacts incl community members, HCWs were positive.
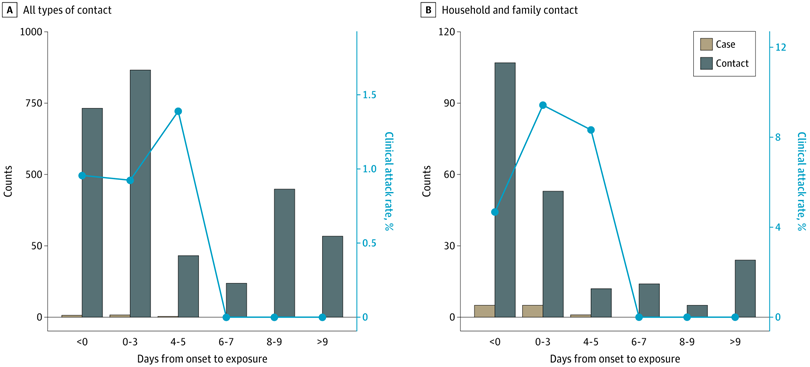
cdc.gov/mmwr/volumes/6… (6/3/20)
cdc.gov/mmwr/volumes/6… (6/3/20)

3/ Based on 1286 close contacts of 319 #COVID19 cases; household and transport contacts had higher risk of transmission (80% of infections caused by 9% of cases), household attack rate of 11.5%, children were as likely to be infected
thelancet.com/journals/lanin… (27/3/20)
thelancet.com/journals/lanin… (27/3/20)
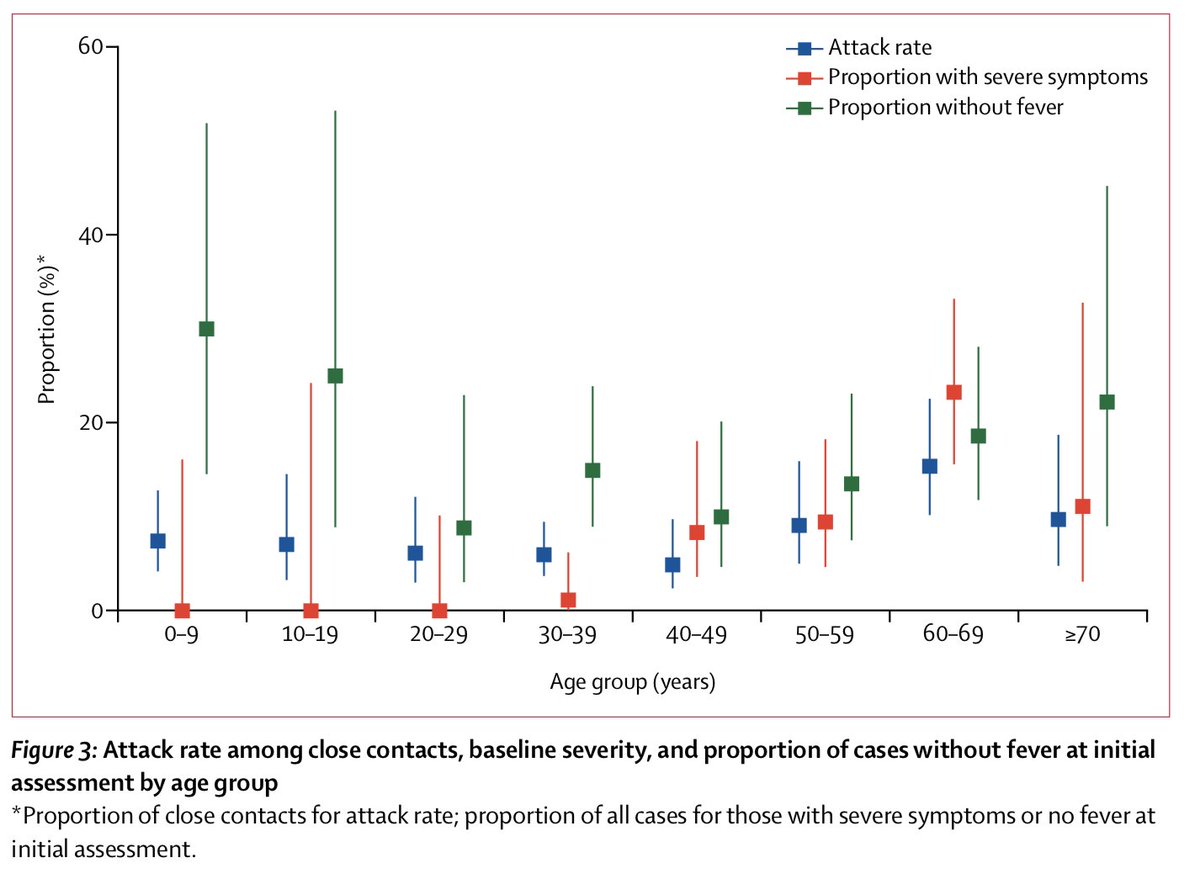
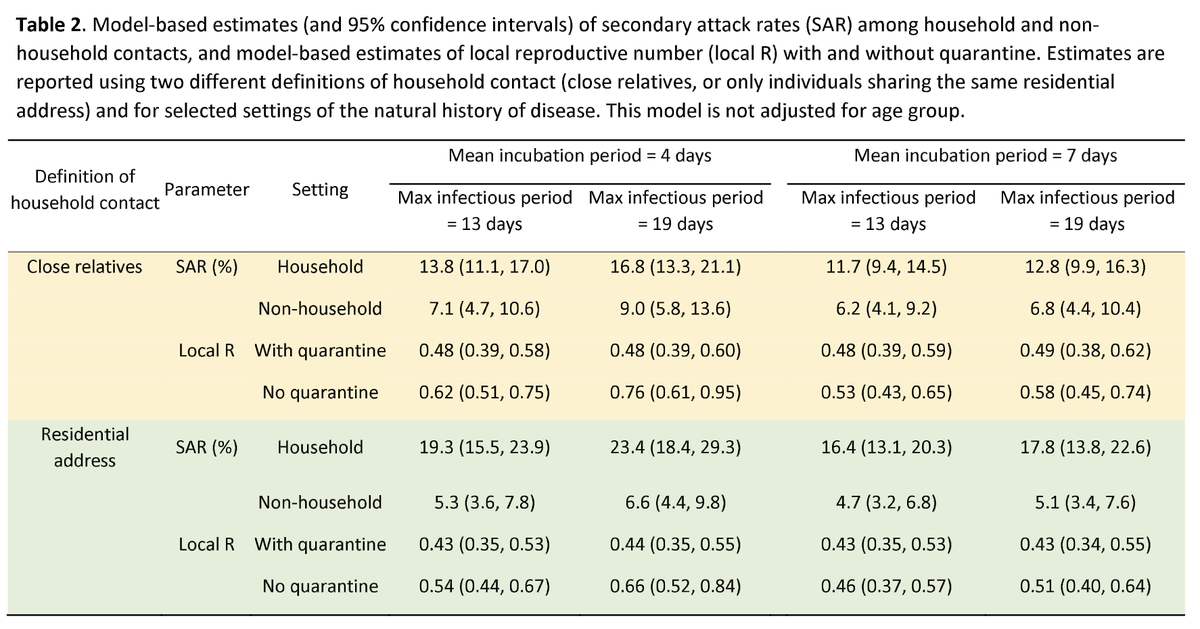
4/ Among 349 #COVID19 cases in 195 clusters, household attack rate was very high (17%), non-household attack rate 7%. Secondary attack rate was lower in <20y (5%) and highest in >60y (18%), suggesting susceptibility increases with age. medrxiv.org/content/10.110… (15/04/20) Preprint 
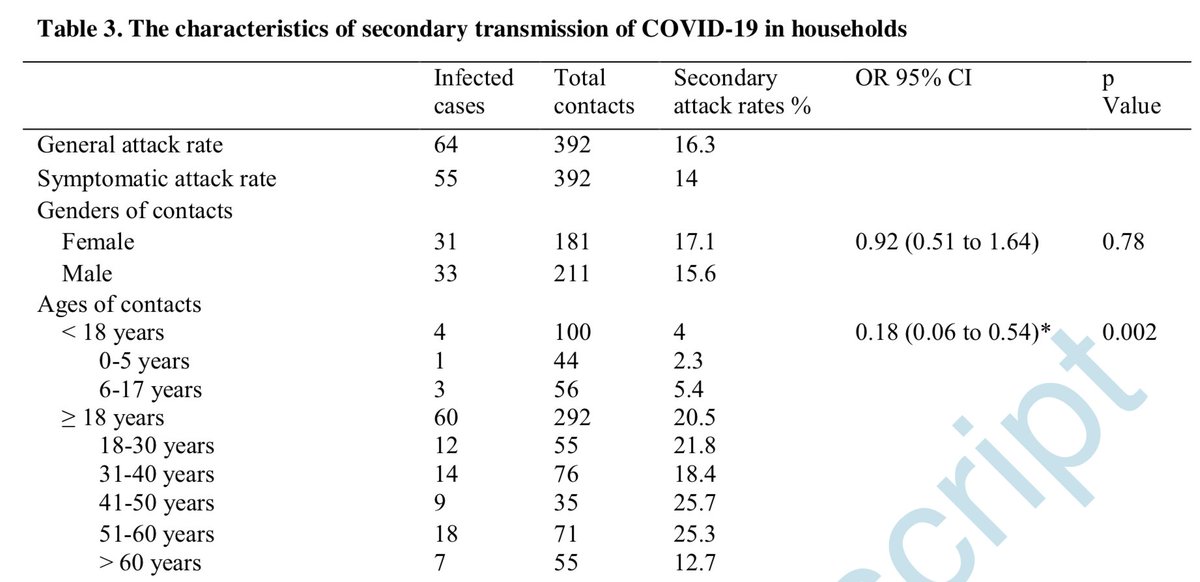
5/ Among 392 household contacts of 105 index #COVID19 cases, overall household attack rate was 16%, the secondary attack rate was highest in spouse (28%), all adults (17%) and was lower in <18 age group (4%).
academic.oup.com/cid/advance-ar… (17/4/20)
academic.oup.com/cid/advance-ar… (17/4/20)
6/ A symptomatic index #COVID19 case, her husband who subsequently acquired infection and their 350 close contacts were followed up, 43 developed symptoms, none tested positive, suggesting close & prolonged exposure is required for transmission.
thelancet.com/journals/lance… (13/3/20)
thelancet.com/journals/lance… (13/3/20)
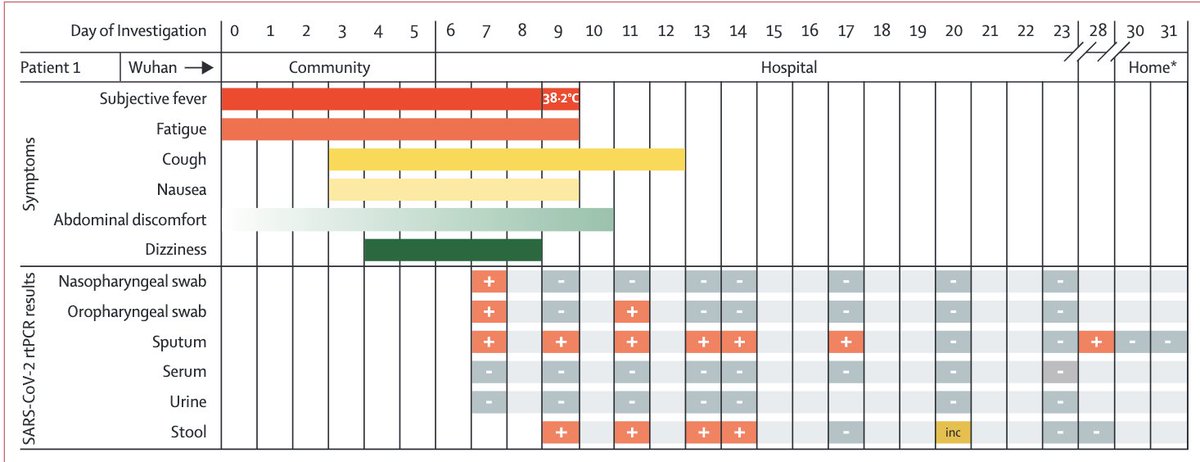
7/ Among 2761 close contacts of 100 confirmed #COVID19 pts in Taiwan, 22 secondary cases were identified, household attack rate was 4.7%, rates were higher in close family, >40y, if exposed within 5d after symptom onset (0 infection after 5d)
jamanetwork.com/journals/jamai… (1/5/20)
jamanetwork.com/journals/jamai… (1/5/20)
8/ In a French chalet cluster, 11/15 contacts tested positive (all adult), 75% attack rate. One child (9y) was negative, attended 3 schools & ski class while symptomatic, among 172 (73 tested) contacts, 1 had #COVID19, while 33% had influenza!
academic.oup.com/cid/advance-ar… (11/4/20)
academic.oup.com/cid/advance-ar… (11/4/20)
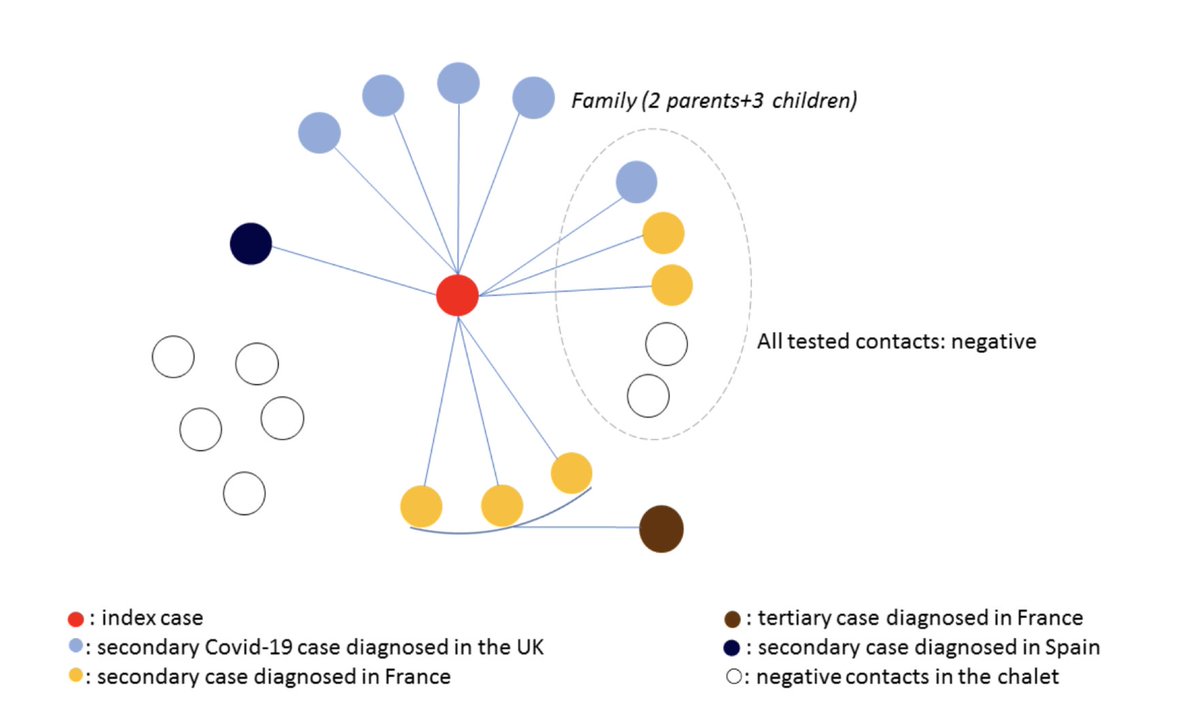
9/ Among 31 household transmission clusters, 9.7% (3/31) were identified as having a paediatric index case (none was identified in Singapore), suggesting that children are unlikely to be driving the household transmission. medrxiv.org/content/10.110… (30/3/20) Preprint 
10/ In a population-based study in Iceland in which 9199 were tested, of the 564 children <10y, 38 (6.7%) tested positive, vs 1183/8635 (13.7%) adolescents and adults tested positive, suggesting lower incidence in children. #COVID19
nejm.org/doi/full/10.10… (14/4/20)
nejm.org/doi/full/10.10… (14/4/20)

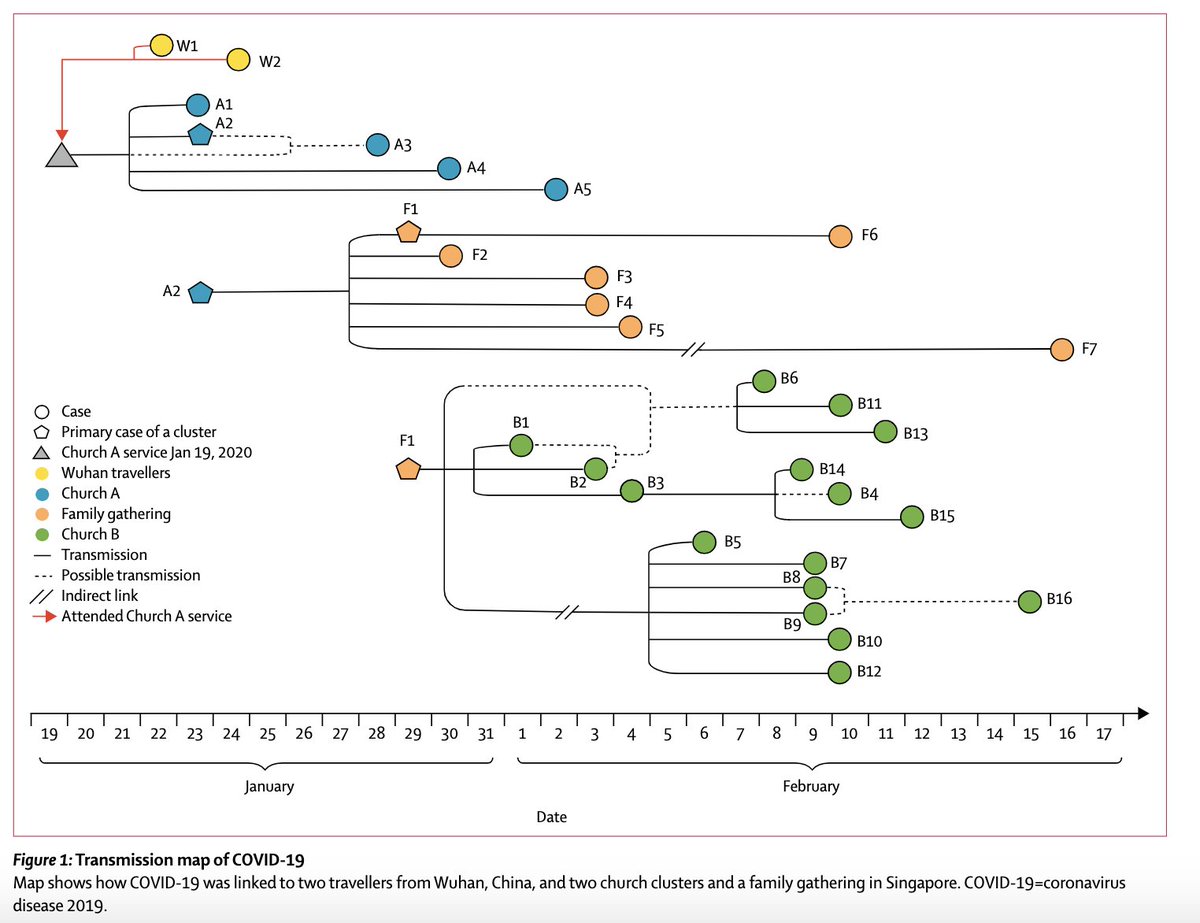
11/ In Singapore, 3 clusters of 28 cases were identified (2 churches, 1 family gathering). In all clusters, transmission accounted for 1 close contact w a symptomatic case, suggesting transmission largely occurs in close contact in congregation.
thelancet.com/action/showPdf… (21/4/20)
thelancet.com/action/showPdf… (21/4/20)
12/ 15 confirmed/probable cases were identified after the index #COVID19 case attended a funeral (3h), shared a meal (2h), birthday party while having mild symptoms, suggesting family gatherings likely plays an important role in transmission
tinyurl.com/yaswk4hh (17/04/20)
tinyurl.com/yaswk4hh (17/04/20)
13/ 408 individuals residing at the shelter over a 2-day period were tested, 36% were positive, suggesting infection could likely be transmitted within homeless shelter easily. In addition, the majority of individuals did not have symptoms.
jamanetwork.com/journals/jama/… (27/4/20)
jamanetwork.com/journals/jama/… (27/4/20)
14/ In a nursing home facility, 23d after the first resident with #COVID19, among 84 residents (76 tested), 48 were positive. This facilty had 64% prevalence of Covid-19 among residents. 50% of residents had no symptoms at the time of testing.
nejm.org/doi/full/10.10… (24/4/20)
nejm.org/doi/full/10.10… (24/4/20)
15/ In summary:
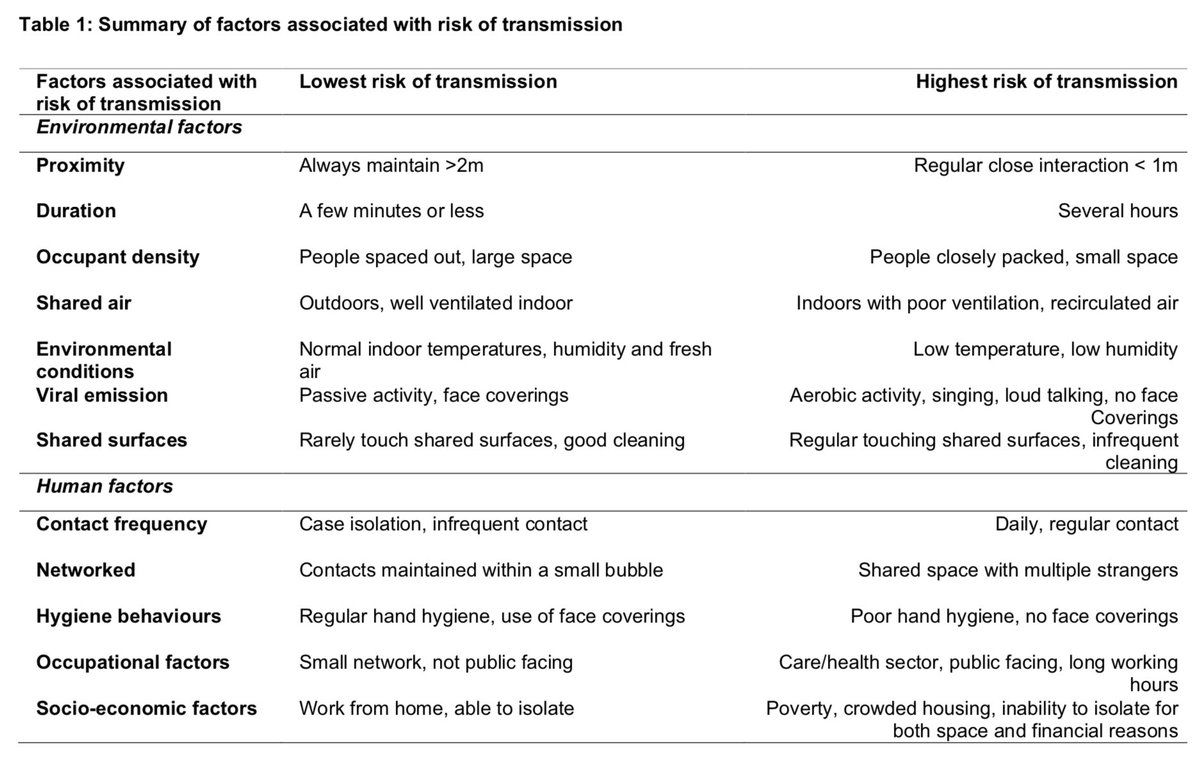
While the infectious inoculum required for infection is unknown, these studies indicate that close & prolonged contact is required for #COVID19 transmission. The risk is highest in enclosed environments; household, long-term care facilities and public transport.
While the infectious inoculum required for infection is unknown, these studies indicate that close & prolonged contact is required for #COVID19 transmission. The risk is highest in enclosed environments; household, long-term care facilities and public transport.
16/ High infection rates seen in household, friend & family gatherings, transport suggest that closed contacts in congregation is likely the key driver of productive transmission. Casual, short interactions are not the main driver of the epidemic though keep social distancing!
17/ Increased rates of infection seen in enclosed & connected environments is in keeping with high infection rates seen in megacities, deprived areas, shelters. A recent preprint demonstrates that #COVID19 epidemic intensity is strongly shaped by crowding
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
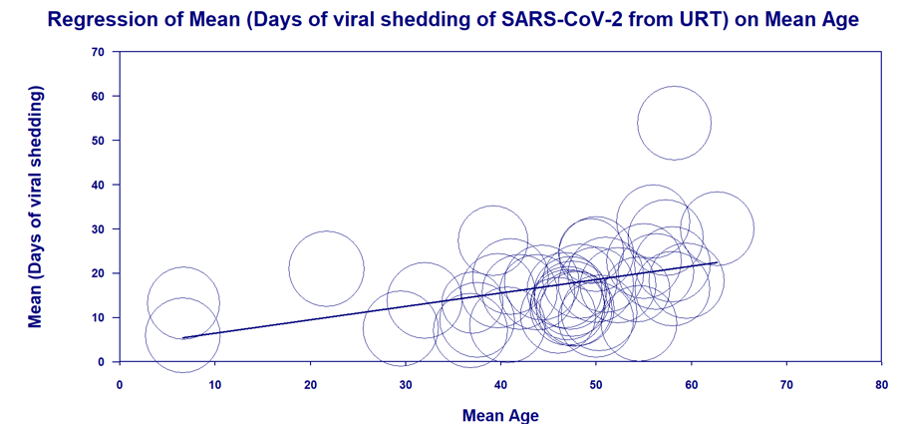
18/ Although limited, these studies so far indicate that susceptibility to infection increases with age (highest >60y) and growing evidence suggests children are less susceptible, are infrequently responsible for household transmission, are not the main drivers of this epidemic.
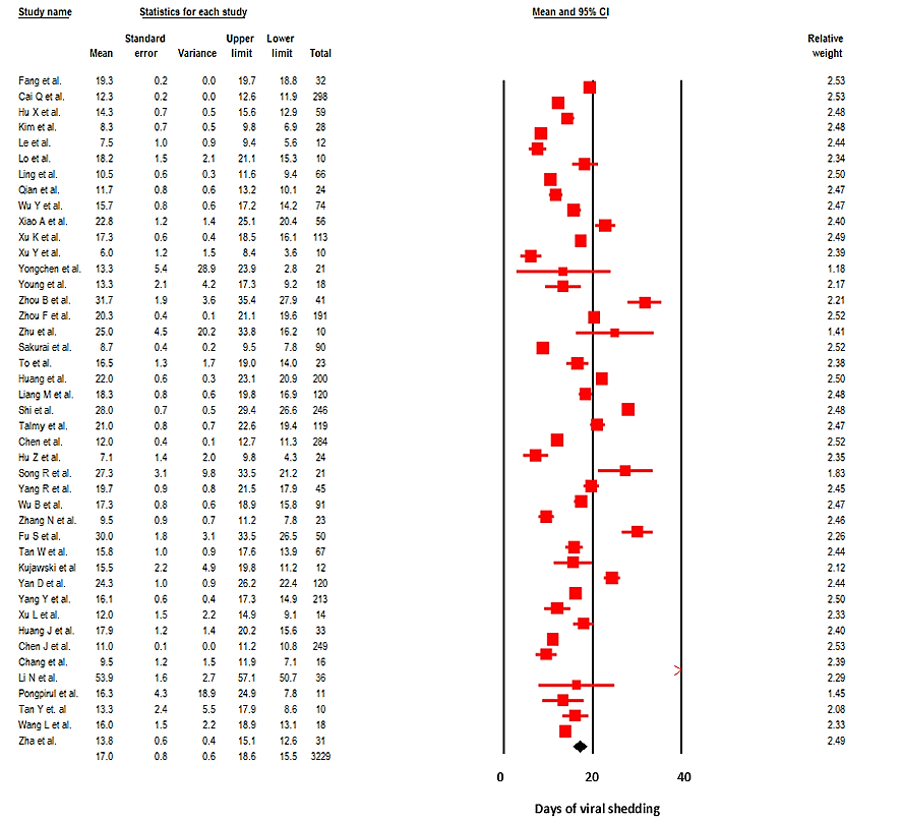
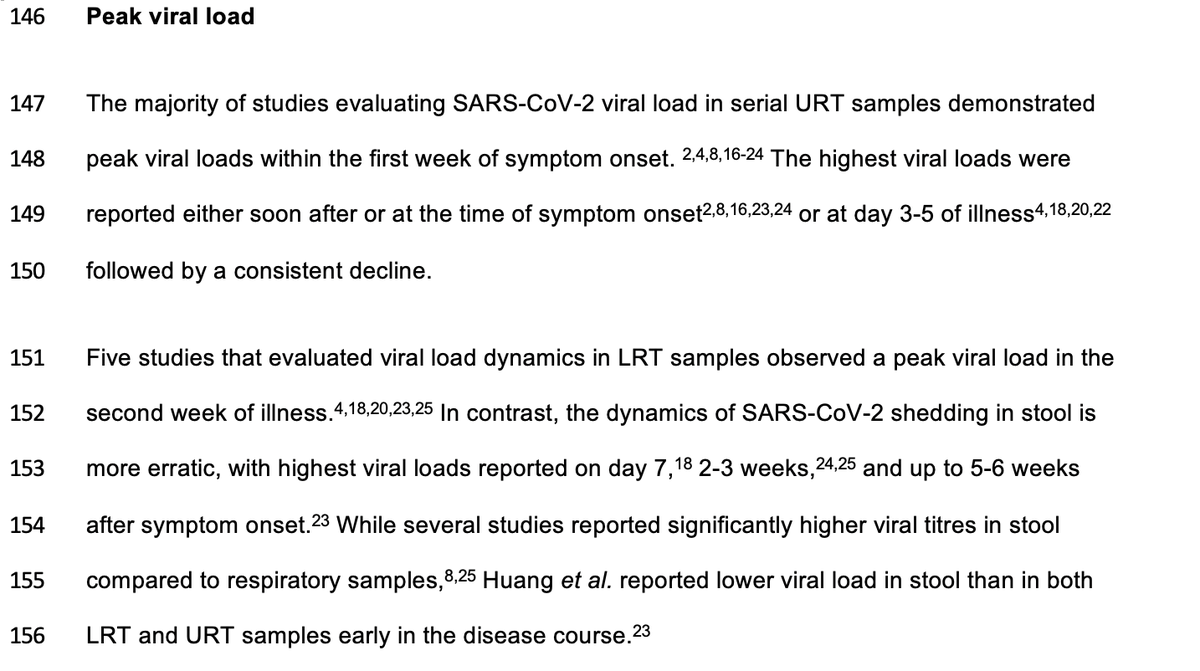
19/ Finally, these studies indicate that most transmission is caused by close contact with a symptomatic case, highest risk within first 5d of symptoms. To note: this preprint suggests that most infections are not asymptomatic during infection medrxiv.org/content/10.110…
20/ In conclusion, contact tracing data is crucial to understand real transmission dynamics. Cautionary note: This data & interpretation is based on the available evidence as of May 4th. Our understanding might change based on community testing/lifting lockdown measures. END
Addendum: While we have limited data, similar high risk transmission pattern could be seen in other crowded & connected indoor environments such as crowded office spaces, other workplace environment, packed restaurants/cafes, cramped apartment buildings etc.
Conclusion 2: (a) we need to redesign our living/working spaces & rethink how to provide better, ventilated living/working environment for those who live in deprived & cramped areas; (b) avoid close, sustained contact indoors & in public transport, & maintain personal hygiene.
• • •
Missing some Tweet in this thread? You can try to
force a refresh