It’s been written up here jamanetwork.com/journals/jama/…
And he did a superb webinar with @JAMA_current where he spoke directly from the front lines esicm.org/blog/?p=2626
They closed elective surgery and created surge ICU capacity ASAP
And then made sure their message was spread out to the world - GET READY
esicm.org/covid-19-updat…
To put that in perspective that’s 20% of their pre-surge ICU capacity
Average LOS 10-14 days jamanetwork.com/journals/jama/…
Separating of patients into COVID and non-COVID streams was key
onlinelibrary.wiley.com/doi/abs/10.111…
advancesinsimulation.biomedcentral.com/articles/10.11…
In the meantime here’s a personal perspective from @avkwong healthmanagement.org/c/icu/issueart…
Inhaled NO not so
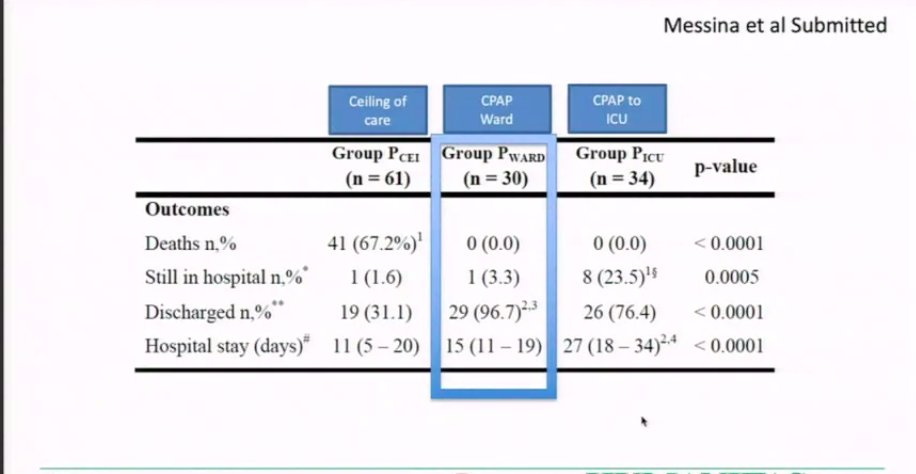
Their experiences with CPAP were interesting. A need for PS on top of CPAP was strong predictor of intubation
@DrMCecconi describes not changing his practice regarding selection of respiratory support for patients. Many of us have reached similar conclusions.
And warns us to “not be surprised twice”.
-increase ICU competencies
-have a “mobile ICU army”
-work in networks
-protect patients and staff
-do research
-continue to contain the disease in community and in hospitals
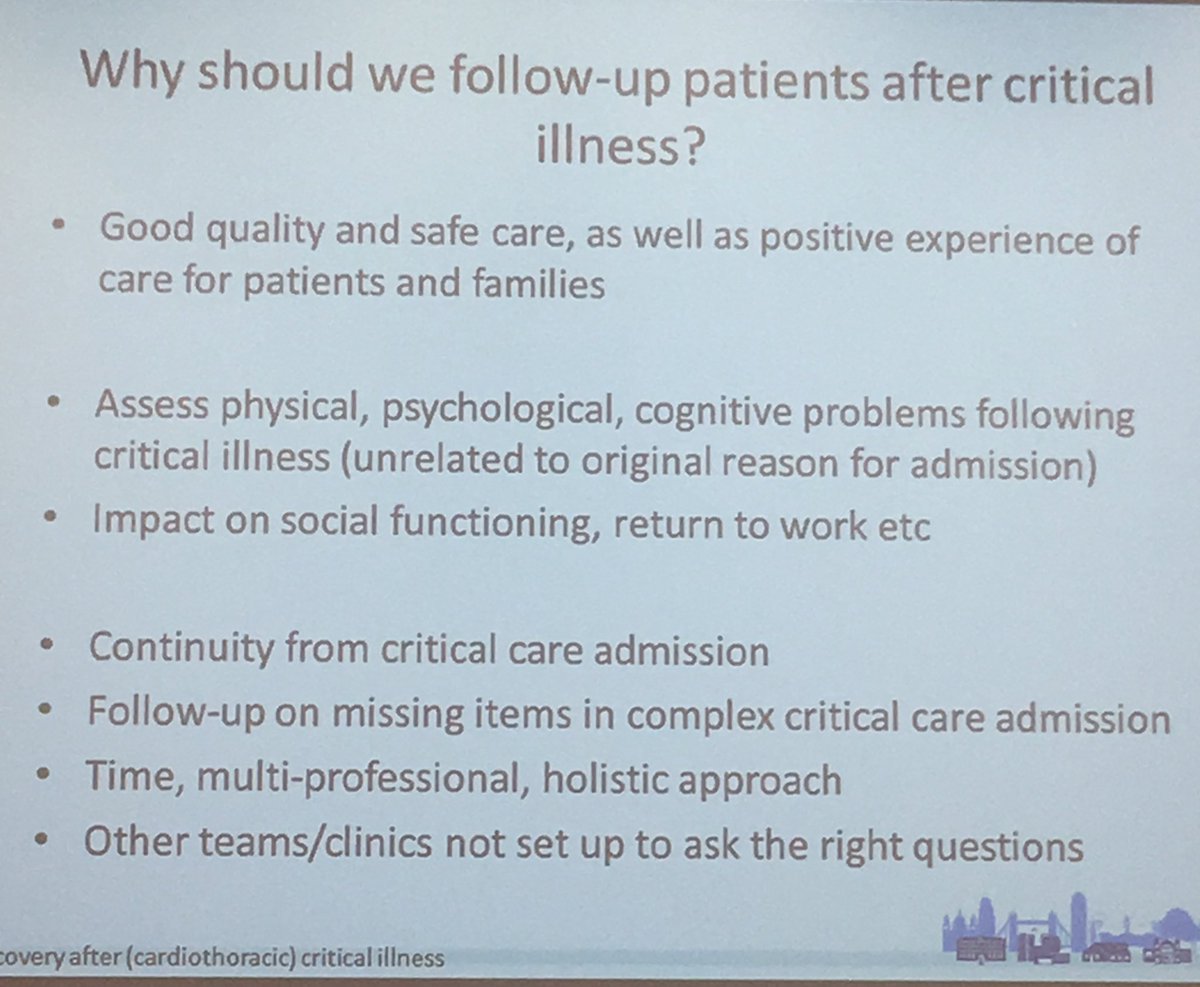
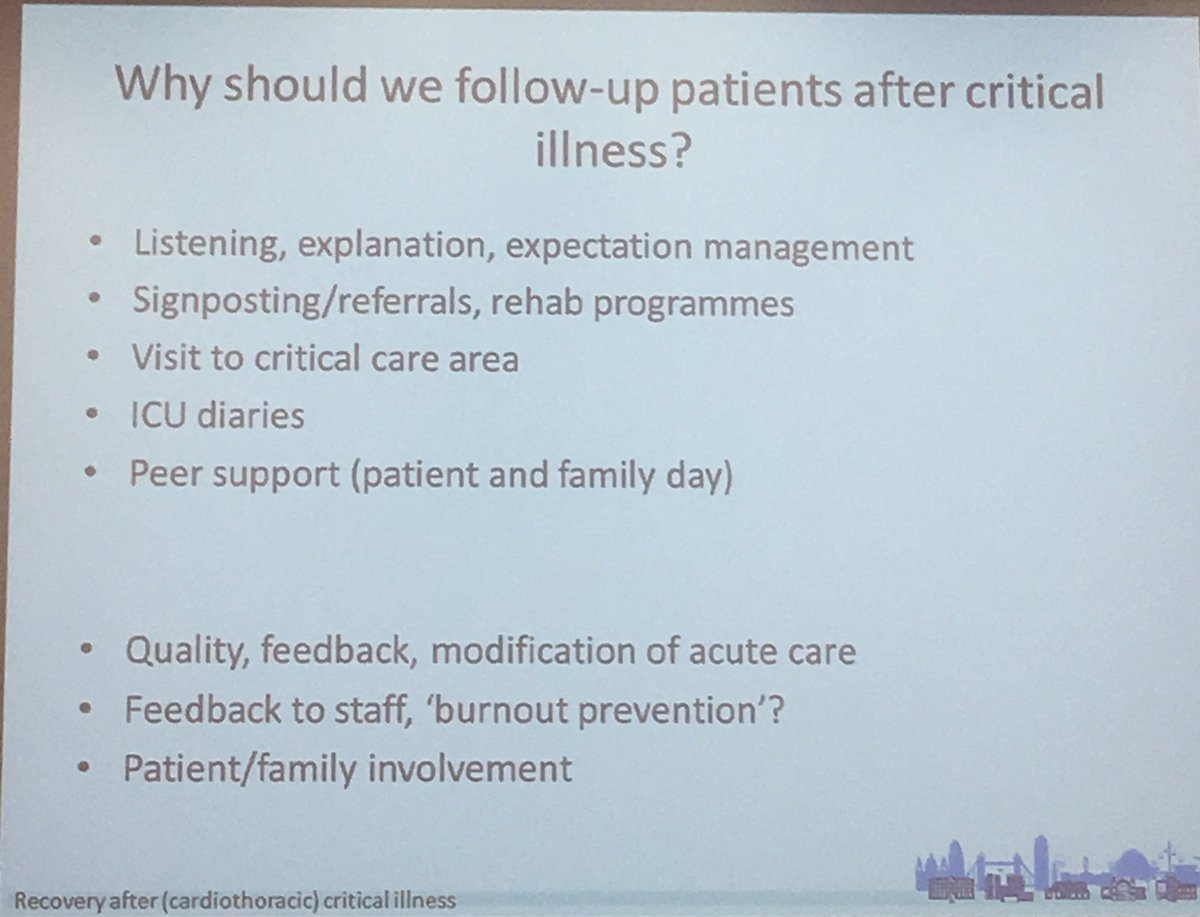
Over time ICU has moved from focusing on survival to looking at wellbeing of both patients and staff
Especially as we recognised that what we do on the unit has long term effects ncbi.nlm.nih.gov/pmc/articles/P…
Follow @HUMANIZALAUCI for more on this
journals.lww.com/ccmjournal/ful…
Sadly during #COVID19 a mix of surge capacity and the risk of cross infection made this very difficult.
Isolation distanced the patients from their families.
Delirium has been commonplace.
Some patients still have issues with physical function up to 5 years after
pubmed.ncbi.nlm.nih.gov/21470008/
We faced a new situation, making challenging decisions under extreme pressures
We were also worried about our health and those of our families/friends...
(I am still living with some effects of this).
Studies are coming out demonstrating the mental toll of acute care in #COVID19 potloc.com/blog/en/potloc…
Support them- psychologists on tap is very helpful.
Compassionate leadership helps.
Some great resources are available thanks to @DrJulie_H ics.ac.uk/ICS/Education/…
Debrief.
Prepare for a potential second peak.
-enhanced decision making (make difficult decisions as a team rather than as individuals)
-give time and space for clinicians to decompress
-try and keep consistent teams to create mutual support
Till next time!