A short thread:
1/ There is a question of whether #TearGas could increase longer term susceptibility to #covid19 from the damaging effects on the respiratory system.
The author cites a study (next tweet) which suggests this may be possible.
npr.org/sections/healt…
1/ There is a question of whether #TearGas could increase longer term susceptibility to #covid19 from the damaging effects on the respiratory system.
The author cites a study (next tweet) which suggests this may be possible.
npr.org/sections/healt…
2/
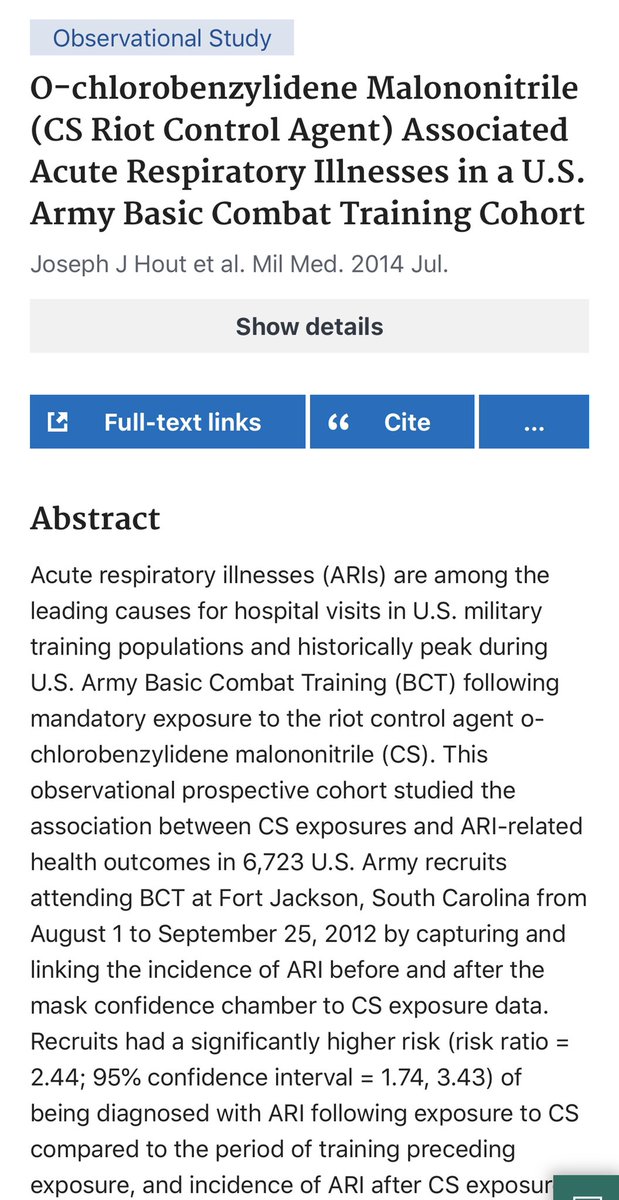
In this prospective cohort study, the risk of developing a viral respiratory illness was significantly higher after exposure to the riot control agent CS, & increased w/ the exposure dose as well.
pubmed.ncbi.nlm.nih.gov/25003867/
In this prospective cohort study, the risk of developing a viral respiratory illness was significantly higher after exposure to the riot control agent CS, & increased w/ the exposure dose as well.
pubmed.ncbi.nlm.nih.gov/25003867/
3/ @lisalsong wrote a great piece on this topic in @propublica.
In a conversation we had, the question came up: what about people who were not protesting but had tear gas exposure as it seeped into their homes?
propublica.org/article/tear-g…
In a conversation we had, the question came up: what about people who were not protesting but had tear gas exposure as it seeped into their homes?
propublica.org/article/tear-g…
4/ If in fact these people are now affected by the gas exposure, law enforcement really has even more responsibility on their hands.
The upshot is this: tear gas should not be used, & especially not in the middle of the #covid19 pandemic.
The upshot is this: tear gas should not be used, & especially not in the middle of the #covid19 pandemic.
• • •
Missing some Tweet in this thread? You can try to
force a refresh








