24y man no PMH. 3-4 days myalgias, freq diarrhea. 2L saline given on med floor -> hypox/tachypnea. COVID pend.
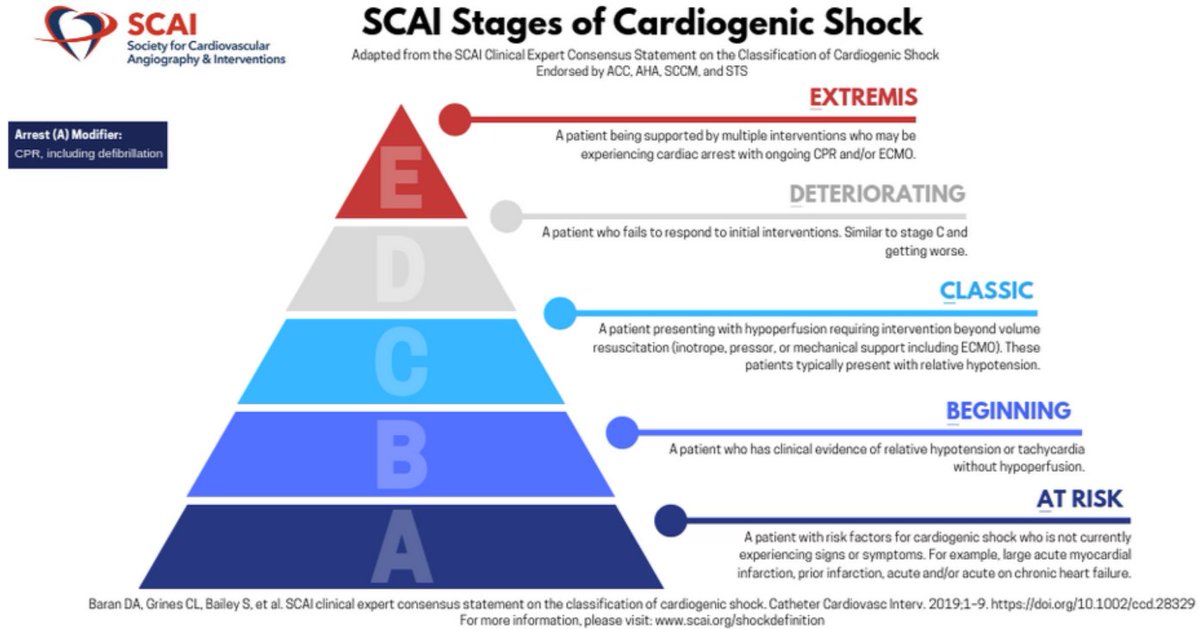
A 👍
B RR30-34, SpO2 92% 5L NC
❤️ MAP 90, HR 110s ->150s over 12 hrs
D Avpu
E Anxious
L CRP 58 (ULN 0.9), Cr 1.4 (no baseline), Lact 4.8

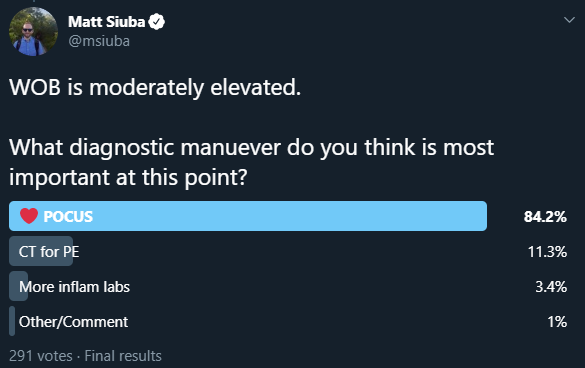
What diagnostic manuever do you think is most important at this point?
More case details to follow tomorrow!
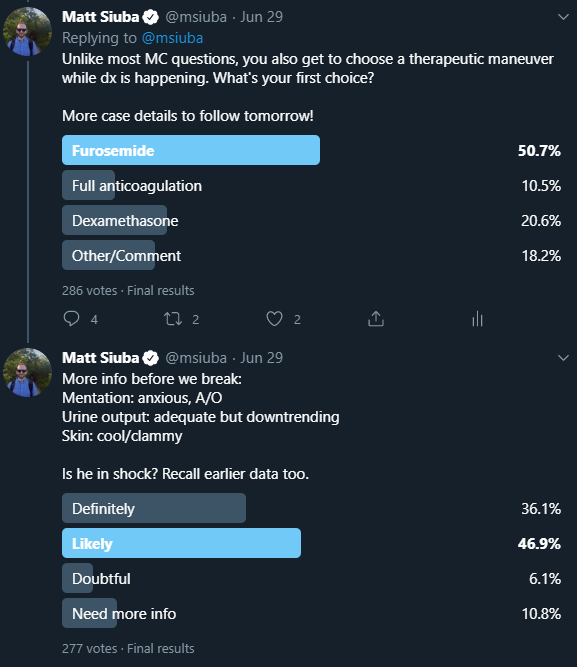
Mentation: anxious, A/O
Urine output: adequate but downtrending
Skin: cool/clammy
Is he in shock? Recall earlier data too.
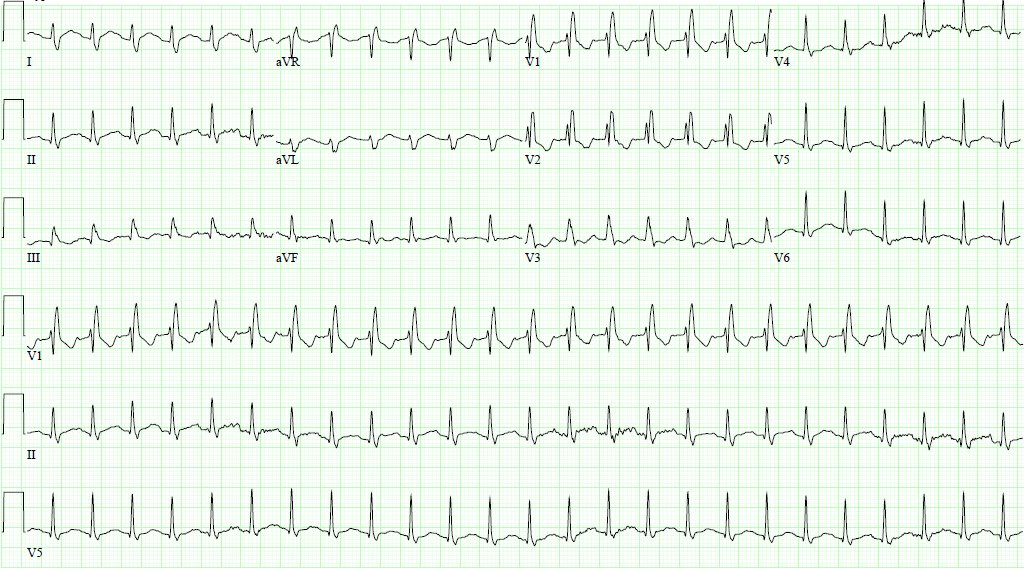
Before you move on in the case, the RN brings you this EKG done for tachycardia. Next step (poll following)?
The vast majority felt #POCUS #echofirst was needed, and that, more likely than not, this patient is in shock.
More of a mix for therapeutic choice, but the #DiuresisJedi crew outvoted the steroid crew.
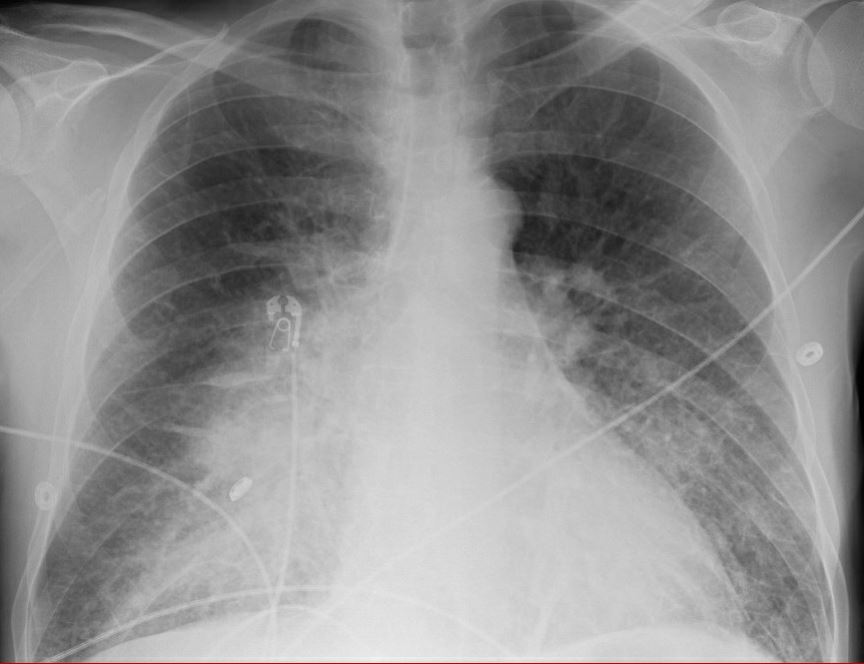
How about that echo?
You're starting to worry that this patient's cardiac output might be dependent on the heart rate of 150.
He is progressively anxious, now prefers to sit upright for respiratory comfort.
Vitals: MAP 100-110, HR 150s, 92% on 5L NC, RR still 30-34
PAPi (measure of RV performance) only 1.25.
More on PAPi here: pubmed.ncbi.nlm.nih.gov/29597051/
Pt has a good deal of MAP room as @Thind888 suggested. As the RN is stringing up nitroprusside, the rapid #COVID19 test comes +
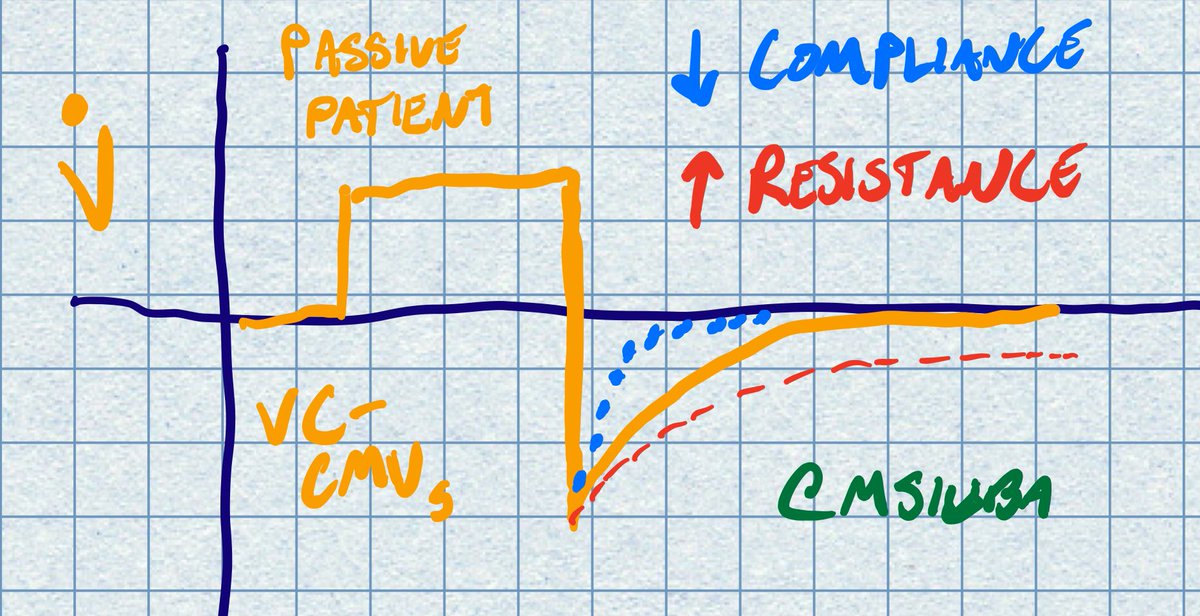
Nitroprusside is pushed to max dose, filling pressures improve a bit, but MvO2 is stable at 48. Lactate still 4.9
Next step?
Dobutamine was started at 5 mcg/kg/min, within 5-10 min frequent PVCs/non-sust VT were seen, so dose cut to 2.5.
Over about an hour, HR began to improve to 120s-130s. MvO2 modestly improved to 54.
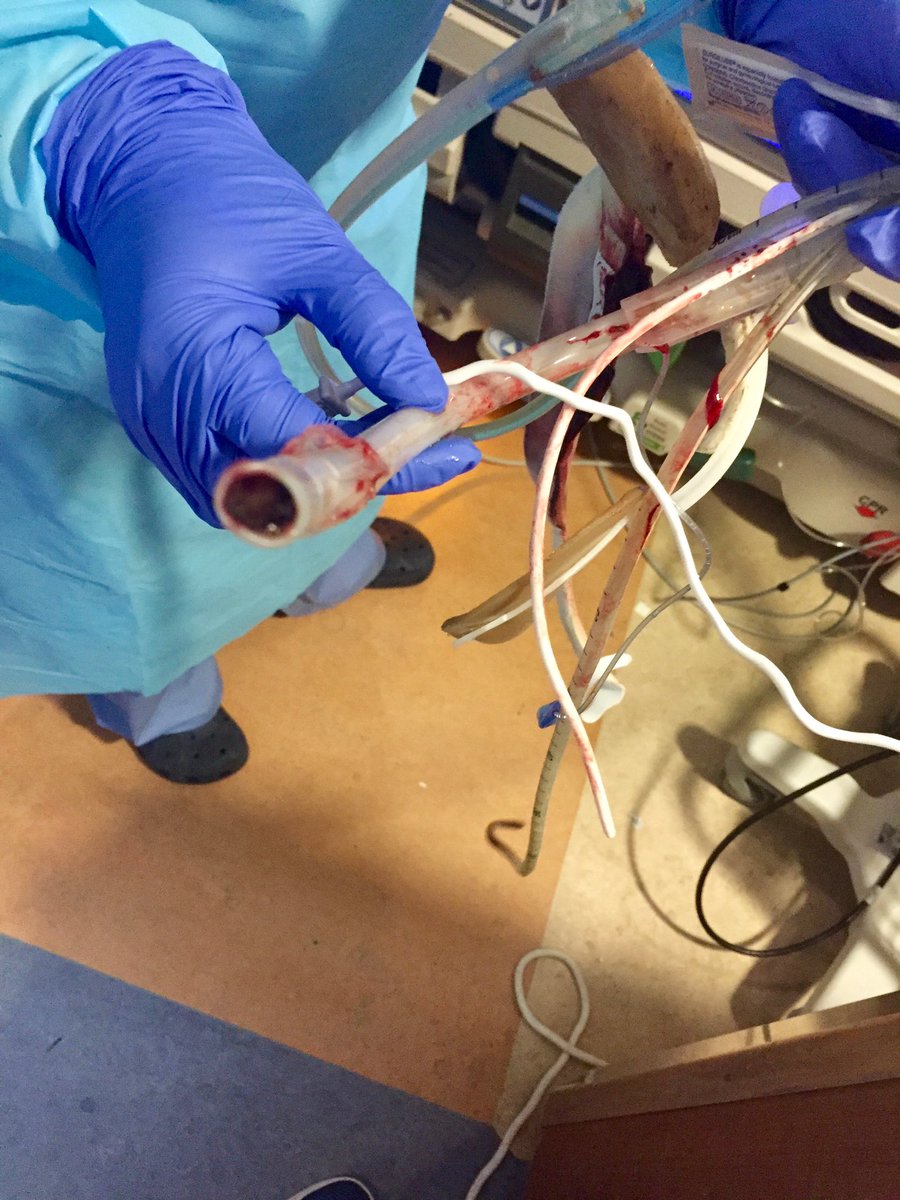
He was intubated and experienced brief PEA arrest in the aftermath.
After prompt transfer to CCU, LVEF had fallen to 10%. VA-ECMO and pLVAD were placed quickly
After several days, LV/RV function recovered to normal levels. He was decannulated and able to leave the hospital, neurologically intact, within 10 days.
Here's an ESC video on it from March, which at this point could be considered outdated:
youtube.com/watch?time_con…
- It is your obligation as a clinician to explain tachycardia. This patient's cardiac output was completely dependent on it in light of such a low SV. Giving fluids or beta blockade here would have certainly been deleterious.
- Know the resources of your institution, and when someone needs to move out ASAP. Delays can be deadly 2/x
- If you practice acute care, *please* learn #POCUS. Waiting for formal studies in patients like this is too costly. 3/3