For diseases that induce immunity, transmission wanes as fraction of population gets infected & recovered because infected people mostly contact immune people. At a certain level (the herd immunity threshold, HIT) cases shift from growing (Rt>1) to shrinking (Rt<1).
tl;dr HIT based on simple models (if R0=2.5, HIT=1-1/R0=60%) are too high but by how much isn't clear.
Yes, if:
1) seroprev is >10%
2) Rt (# cases/case) was <2 due to beh. change
or
Before assessing data for each let's remember, as @trvb nicely described, that COMBINATION of these can drive Rt<1
On to the data!
Even w/ overshoot would need R0>>2.5 to get NYC seroprev if HIT=10%.
Lockdown is much more likely explanation for stop in NYC epidemic.
Data: Very plausible. Rise in cases post-lockdown in most states has been nowhere near as fast as the rise in March. As @trvrb points out Rt estimates are much lower. epiforecasts.io/covid/posts/na…
(much better source than rt.live)

Data: Uncertain.
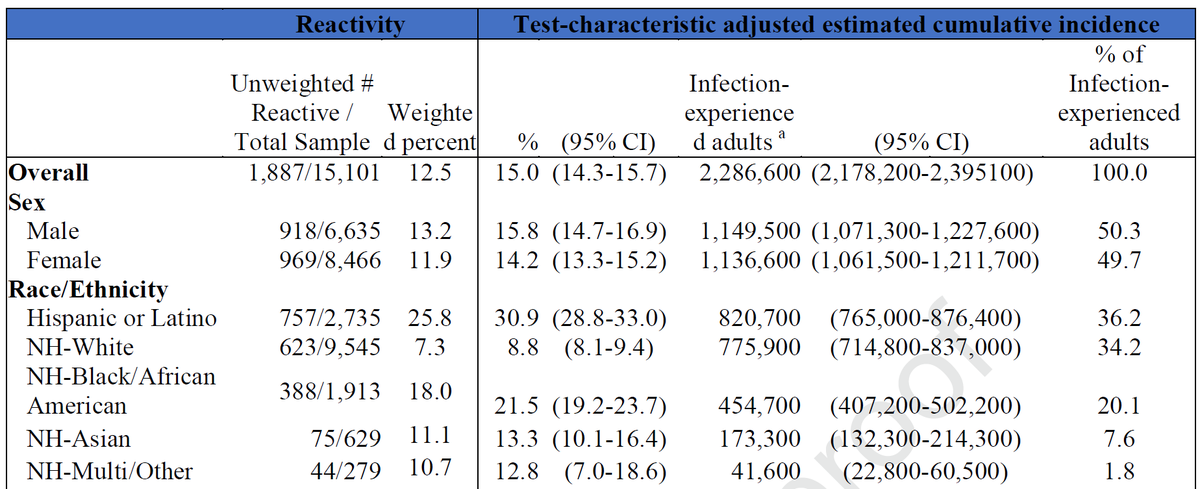
@trvrb & others @youyanggu use back of envelope multipliers of cases to get estimates of # of infections & then divide by pop to get seroprev or frac infected. Early in epidemic we all guessed & used 10x. @trvrb uses 8x. Is it right?
If we had sequential seroprev estimates we could know.
thelancet.com/journals/lance…

These are high numbers. So high, in fact that a very small serosurvey could accurately characterize seroprevalence & distinguish b/w them (& from lower #s like 10%).
But I think it'd be very good to use @trvrb 's simple calculations to argue it's important to measure seroprev across FL repeatedly.
So, meet outside, give space, & wear a mask!