X descent = atrial relaxation, y descent = early ventricular filling. Both are negative waveforms due to lowering of pressure.
So if pressure doesn't fall--waveform less negative (i.e blunted)
X descent can be normal or dominant: Tricuspid valve is pulled away "more" (due to less bld in RV)pressure is more negative.
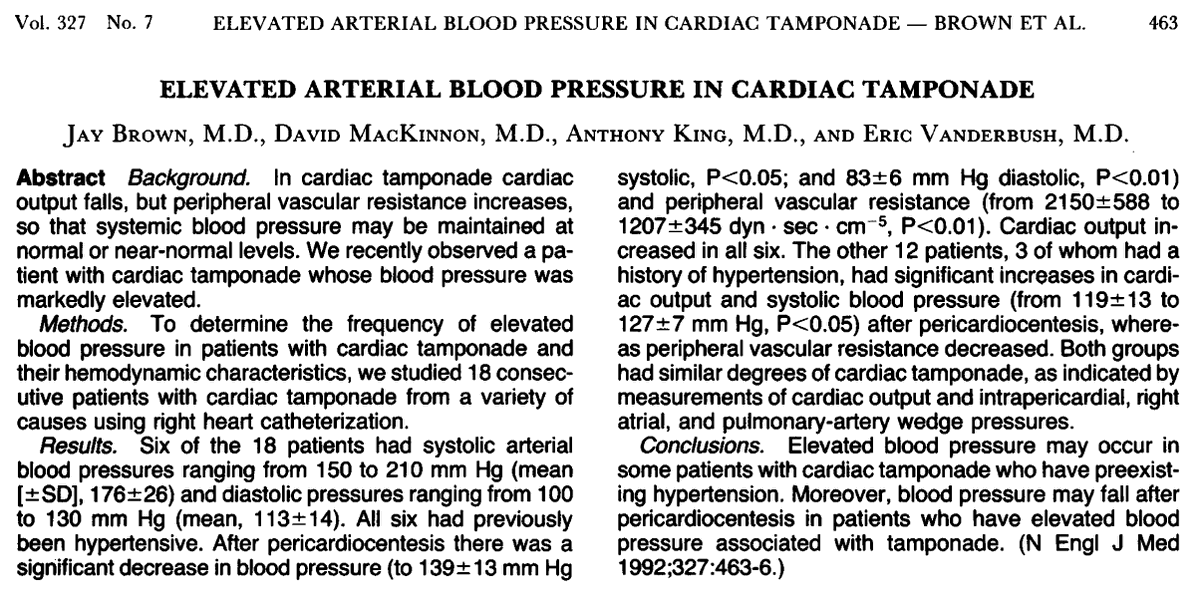
in arterial pressure of 10 mm Hg or more during
normal breathing. Not pathognomonic of PT.
Also seen with massive PE, status asthmaticus & hemmorhagic shock.
Absence of pulsus parodoxus seen in acute pericardial tamponade is seen in
Trivia buffs @pccm_doc may ask about Friedreich’s sign:
Deep y descent of the jugular venous waveform. Seen in constrictive pericarditis. A great video is in this link
ncbi.nlm.nih.gov/pmc/articles/P…
Echo/Pocus:
RA collapse (more specific if collapse > 30% cardiac cycle)
RV collapse (less sensitive, more specific)
Plethoric IVC. MV inflow variation >25% +effusion
EKG: Sinus tach, low QRS, electrical alternans
About alternans-
If for boards they give Cath data:
All 4 chambers = same pressures
Needle paracentesis (pericardiocentesis) under echo guidance at the bedside in the PICU.
Consult cardiology/CICU attending, Avoid intubation (ketamine +fentanyl/versed for sedation), RT to hold jaw thrust/CPAP. Wouldn't make this a 1st year fellow procedure.
pubmed.ncbi.nlm.nih.gov/12917306/
Pt with raised JVP, or AKI or hepatic dysfunction (transaminitis): heart evaluated (CXR, EKG, ECHO). Any Pt with dyspnea who cannot lay supine, fluid overloaded patients (pts with renal failure, nephrotics, lupus, transplant etc) deserve a cardiac eval.
@KerrynRoome
Know conditions where there is no hypotension or pulsus paradoxus is absent. Not a sign of weakness to call for help (CICU/cards/RTs/other colleagues etc. prior to drainage)
@MKIttlesonMD @pccm_doc @GirishGDeshpan1 @FortenberryMD @hyguruprep @yoncabulutmd @agstormorken @AlexRotta #MedTwitter #AcademicTwitter @ChecchiaPaul @brownam130 @abusultaneh @JWilliamsonDO