
Working through an interesting cardiopulmonary exercise test!
For any physiology fans or new pulmonary and cardiology fellows out there
#MedTwitter #cardiotwitter #physiology #exercise #CPET #FOAMed @EM_RESUS #CardioEd #Cardiology
Lets make sense of all this information:


For any physiology fans or new pulmonary and cardiology fellows out there
#MedTwitter #cardiotwitter #physiology #exercise #CPET #FOAMed @EM_RESUS #CardioEd #Cardiology
Lets make sense of all this information:


Starting off with the HPI:
70 yo M PMH of HF(45% EF), LAD, PDA coronary disease requiring PCI and coronary stenting. Now reports dyspnea on exertion that has been progressive for the past 8 years. First noted when golfing but now even on mild-moderate exertion.
70 yo M PMH of HF(45% EF), LAD, PDA coronary disease requiring PCI and coronary stenting. Now reports dyspnea on exertion that has been progressive for the past 8 years. First noted when golfing but now even on mild-moderate exertion.
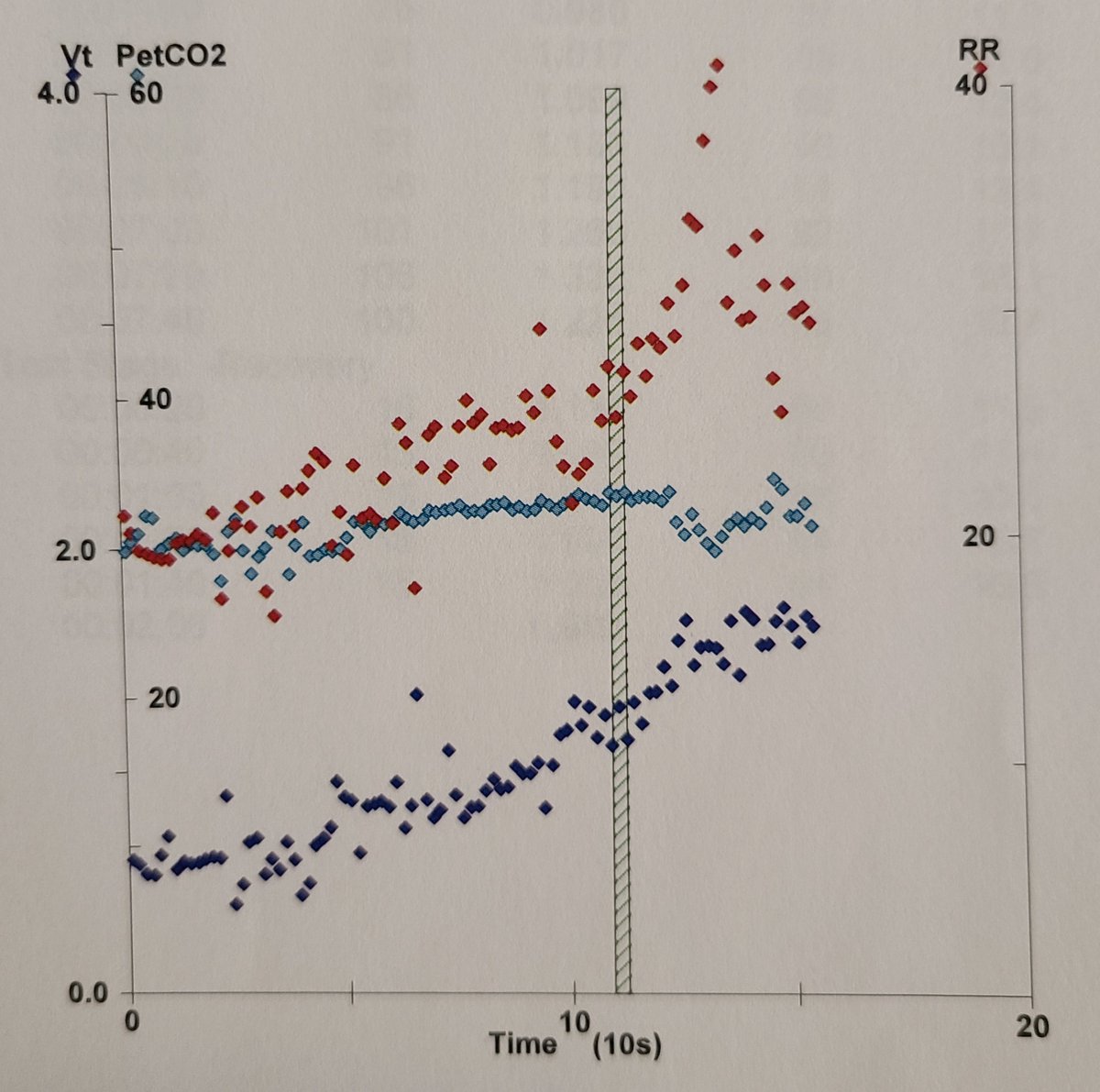
These were the results obtained from our CPET. The patient’s maximum oxygen consumption (VO2 max) was only 73% of predicted (LOW) 



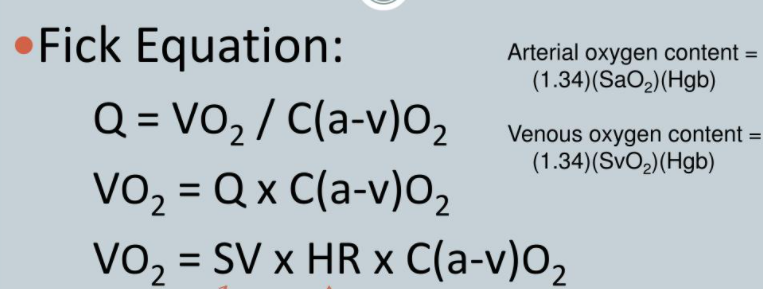
To understand the crux of the issue lets look at the Fick equation:
Oxygen consumption is dependent on our cardiac output as well as arterial and venous oxygen content. The CPET looks at all these determinants to figure out why we have a reduced VO2 max (presenting as dyspnea)
Oxygen consumption is dependent on our cardiac output as well as arterial and venous oxygen content. The CPET looks at all these determinants to figure out why we have a reduced VO2 max (presenting as dyspnea)
We roughly divide the causes of reduced VO2 max into 3 categories
1) Pulmonary
2) Cardiac
3) Metabolic, myopathic or neuromuscular.
With pulmonary causes we look at whether there was a
A) Ventilatory
B) Gas exchange or
C) Diffusion abnormality
1) Pulmonary
2) Cardiac
3) Metabolic, myopathic or neuromuscular.
With pulmonary causes we look at whether there was a
A) Ventilatory
B) Gas exchange or
C) Diffusion abnormality
Ventilatory limitations would present as reduced VO2 max despite reaching a maximal voluntary ventilation (MVV) which is the total volume of air exhaled during 12 seconds of rapid deep breathing or estimated as patient’s FEV1 x 40
Our patient achieved 59.1 L/min or 62% of his MVV at maximum exercise: Meaning that he has plenty of ventilatory RESERVE left at the time of terminating the test and hence was not the major limiting factor here. 

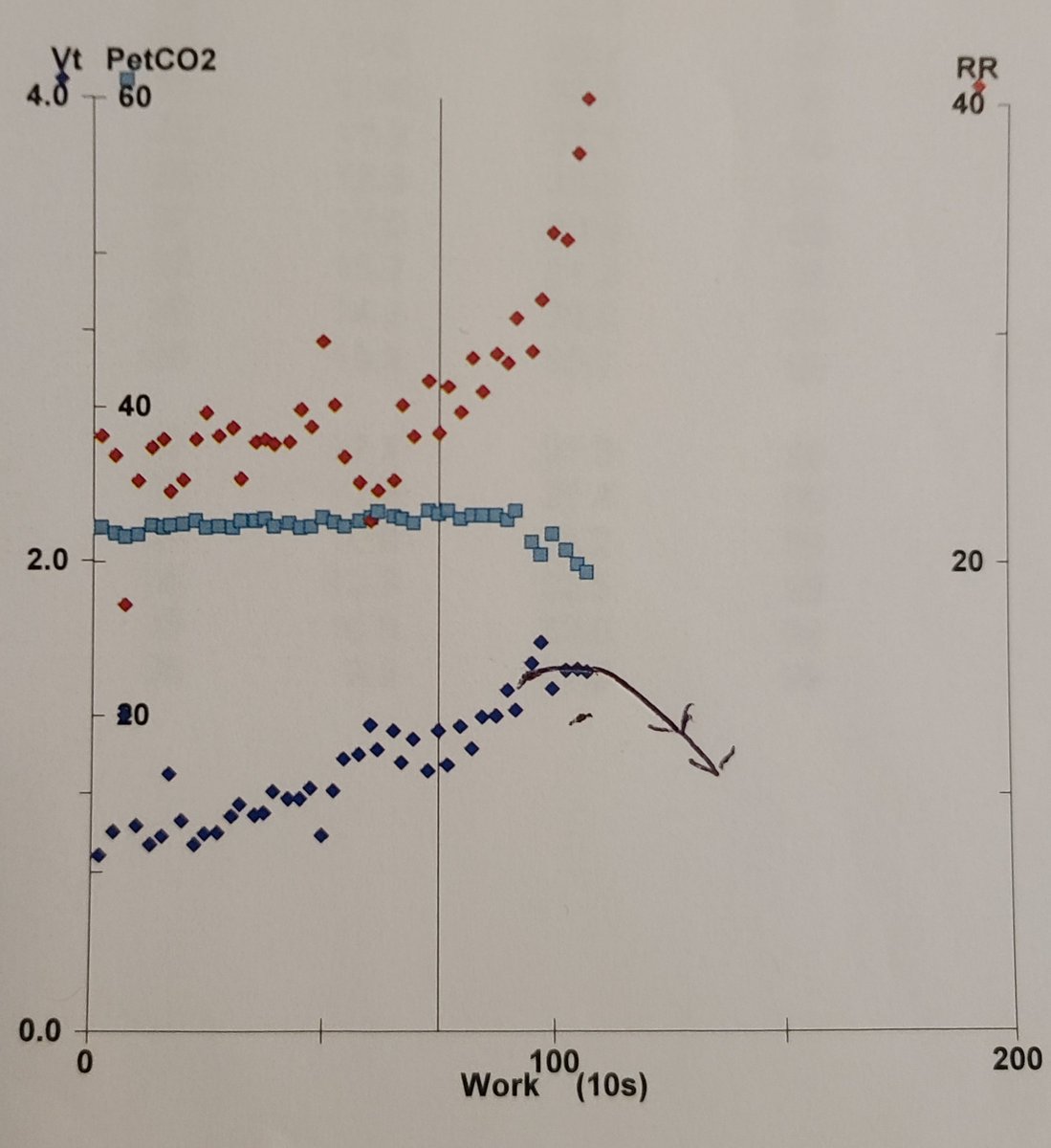
We also noted the patient was able to increase his tidal volume upto 3x his baseline (Normal =2x-3x during exercise) and his respiratory rate did not exceed 50/min (Reduced TV and increased RR noted in restrictive lung disease) 

We also assess for “Dynamic hyperinflation” i.e does the tidal volume drop with increasing respiratory rate (noted in obstructive lung diseases)
Here there is a consistent rise in TV with increasing RR and so no DH was present (arrow shows what that would look like and example)

Here there is a consistent rise in TV with increasing RR and so no DH was present (arrow shows what that would look like and example)

Is there a gas exchange abnormality? To assess this we look at whether our deadspace ratio (VD/VT) is elevated at anaerobic threshold (AT, the point at which the body switches to anaerobic respiration due to insufficient oxygen delivery)
Deadspace is volume of air in the lungs that does not participate in O2 or CO2 gas exchange and is usually elevated in cardiac (low CO) or pulmonary diseases (e.g obstructive)
VD/VT increases with VE/VCO2 (ventilatory equivalents of CO2) by rearrangement of this formula
VD/VT increases with VE/VCO2 (ventilatory equivalents of CO2) by rearrangement of this formula

Our patient had a VE/VCO2 of 34.5 at AT which is higher than predicted (33.6)!!! Although only marginally increased this may be an indicator of why he has an exercise limitation. 



Anaerobic threshold is the point at which the VE/VCO2 slope reaches its nadir, plateaus, and then starts to increase. Initially CO2 production ramps up till AT where the patient then increases their minute vent (due to anaerobic resp) and reverses the trend of the VE/VCO2 curve
Other markers of AT are a nadir and upslope of the VE/VO2 curve (showing an increase in minute vent compared to increases in oxygen consumption) and an up tick in end tidal O2 noted because of a drop of alveolar CO2 concentration driven by the rise in minute ventilation 

Is there a diffusion abnormality? Simple enough to check for that as we are looking for a >4% decrease in oxygen saturation during exercise
Our patient was able to maintain a saturation of 99% throughout
He also did not demonstrate post exercise reduction in FEV1 or bronchospasm

Our patient was able to maintain a saturation of 99% throughout
He also did not demonstrate post exercise reduction in FEV1 or bronchospasm


From a cardiac perspective! Lets examine the components of oxygen delivery!
Abnormalities in these components would explain our reduced VO2 Max
We already determined that the saturation remained normal throughout and our patient’s hemoglobin is acceptable at 13.1

Abnormalities in these components would explain our reduced VO2 Max
We already determined that the saturation remained normal throughout and our patient’s hemoglobin is acceptable at 13.1


Does the problem then lie in the patient’s ability to mount an appropriate Cardiac output? The VO2 at AT was normal but cardiac output may be a factor at maximum exercise
CO is usually increased by raising SV initially but late in exercise is raised by increases in HR
CO is usually increased by raising SV initially but late in exercise is raised by increases in HR
Looking the Fick equation again we can rearrange it such that assuming our differences in arterial and oxygen content are constant the stroke volume is directly proportional to the ratio between o2 consumption VO2 and HR, also known as the O2 pulse! 

Here for our patient we see a rise in the O2 pulse: linear increase in stroke volume with work load but without a significant increase in HR throughout the test. The patient achieves a HR of 94 (58% of his pred max) at maximum exercise at which point he had to terminate the test. 

We can ask our self whether the heart rate did not reach maximum because the patient did not give us a maximum effort but we have two strong points against this hypothesis
1) The patient was unable to continue the test further because of reduced pedal cadence: clinical parameter of max effort
2) RQ was >1.15 at maximum exercise which is considered a marker of significant anaerobic respiration and maximum effort (RQ normally 0.8 during aerobic resp)
2) RQ was >1.15 at maximum exercise which is considered a marker of significant anaerobic respiration and maximum effort (RQ normally 0.8 during aerobic resp)

His baseline EKGs demonstrated a left bundle branch block and 1st degree AV block.
We were convinced that the patient had chronotropic incompetence also supported by his baseline EKG findings which would suggest an inability to augment HR with exercise!
We were convinced that the patient had chronotropic incompetence also supported by his baseline EKG findings which would suggest an inability to augment HR with exercise!
His history also revealed he had developed hypotension in the past year due to which he was no longer able to tolerate his HF medical therapy and was weaned off his beta blocker and afterload reduction
It would make sense that he would have a hypotensive response to BB therapy
It would make sense that he would have a hypotensive response to BB therapy
There are so many more subtleties to CPET testing but I wanted to highlight the interesting findings in this case.
Many reference pictures here are taken from the ACCP CHEST video on CPET testing by one of my mentors Dr Zachary Morris. Link:
Many reference pictures here are taken from the ACCP CHEST video on CPET testing by one of my mentors Dr Zachary Morris. Link:
Loved learning all of this with Dr Lazar at @HFHPulmCC
Hope this helps any new fellows out there starting to look at their CPET tests
#MedTwitter #FOAMed #CardioEd #Cardiology
Hope this helps any new fellows out there starting to look at their CPET tests
#MedTwitter #FOAMed #CardioEd #Cardiology
• • •
Missing some Tweet in this thread? You can try to
force a refresh


