Over the last 6 months, we've learned a lot about how SARS-CoV-2 spreads🦠
What does the evidence so far tell us about SARS-CoV-2 transmission dynamics, high-risk activities and environments? Thread 🧵 (1/n)
papers.ssrn.com/sol3/papers.cf…
What does the evidence so far tell us about SARS-CoV-2 transmission dynamics, high-risk activities and environments? Thread 🧵 (1/n)
papers.ssrn.com/sol3/papers.cf…
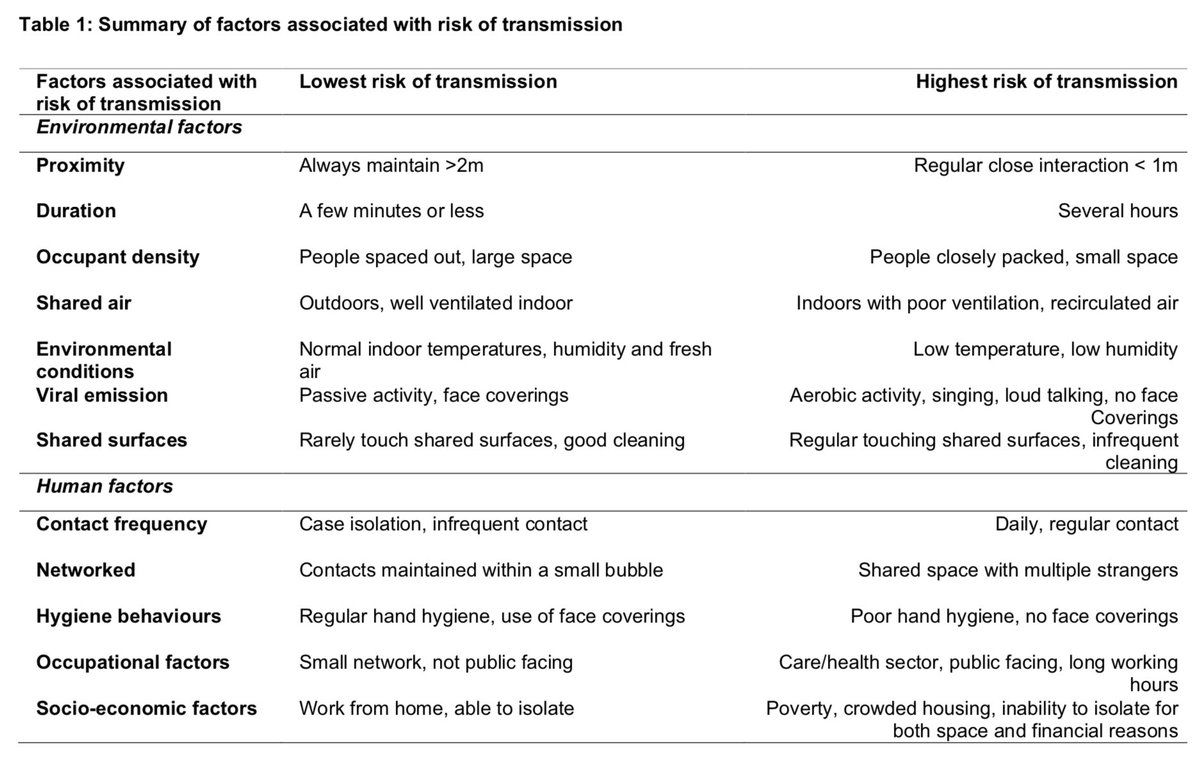
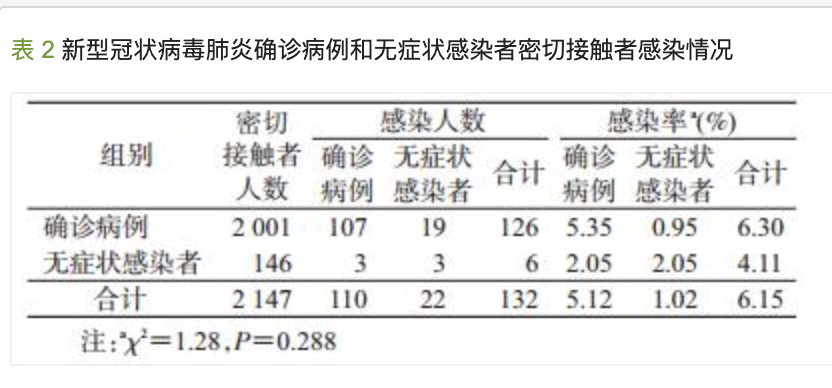
The risk of transmission is complex and multi-dimensional. It depends on many factors: contact pattern (duration, proximity, activity), individual factors, environment (i.e. outdoor, indoor) & socioeconomic factors (i.e. crowded housing, job insecurity). (2/n) 
Contact pattern:
We now know that sustained close contact drives the majority of infections and clusters. For instance, close family/friend contacts and gatherings are a higher risk for transmission than market shopping or brief community encounters. (3/n)
We now know that sustained close contact drives the majority of infections and clusters. For instance, close family/friend contacts and gatherings are a higher risk for transmission than market shopping or brief community encounters. (3/n)
https://twitter.com/mugecevik/status/1257392347010215947?s=20
Even in the same household being a spouse/partner, sleeping in the same room or sharing the same sleeping space, frequent daily contact with the index case, and dining in close proximity has been associated with increased risk of transmission. (4/n)
For non-household contacts, engaging in group activities such as dining together or board games have been found to be high risk for transmission. So, the risk increases with longer & frequent exposure, close proximity, # of contacts, and group activities especially dining (5/n)
Individual factors:
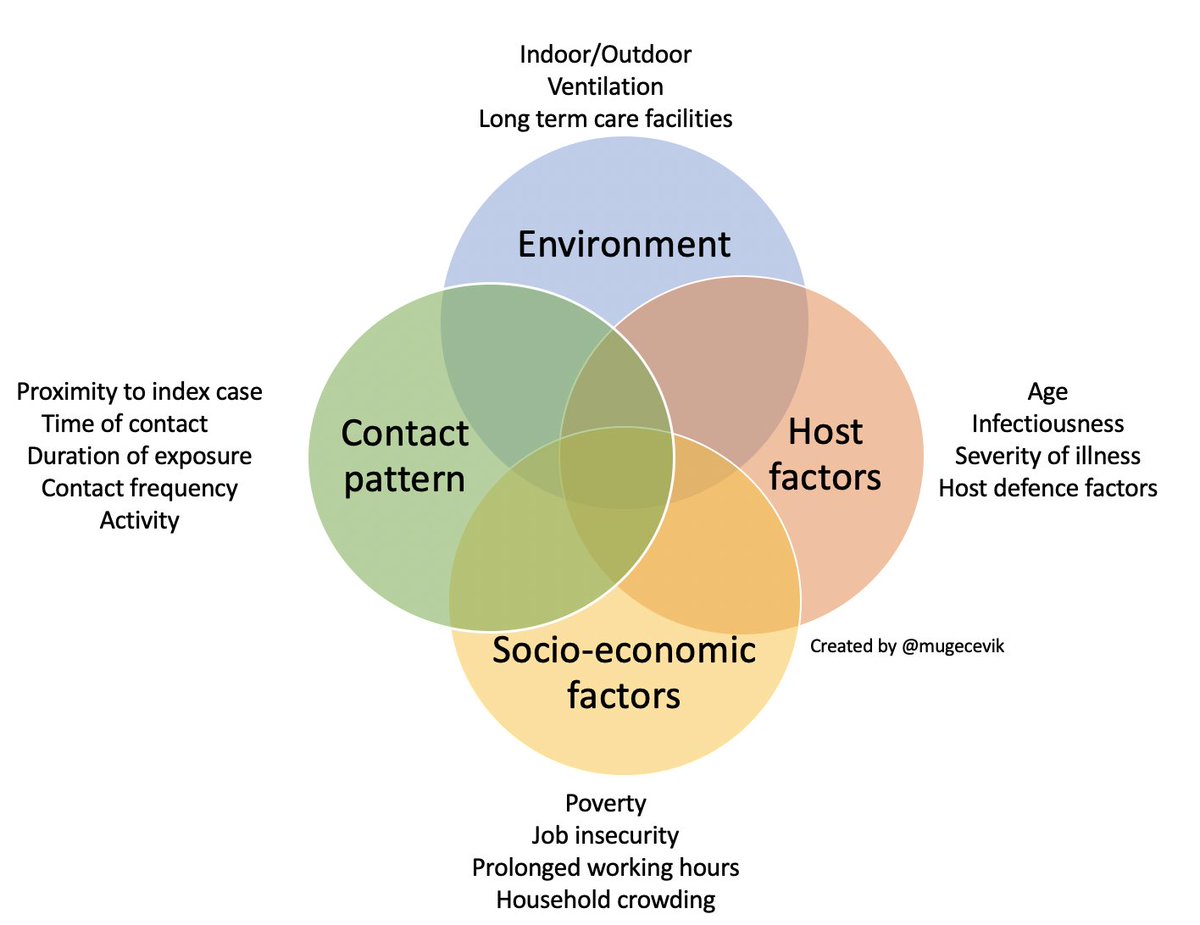
Many ppl either do not infect anyone or infect a single person, and a large number of secondary cases are caused by a small # of infected ppl. Although this also is related to other factors, individual variation in infectiousness plays a major role.(6/n)
Many ppl either do not infect anyone or infect a single person, and a large number of secondary cases are caused by a small # of infected ppl. Although this also is related to other factors, individual variation in infectiousness plays a major role.(6/n)
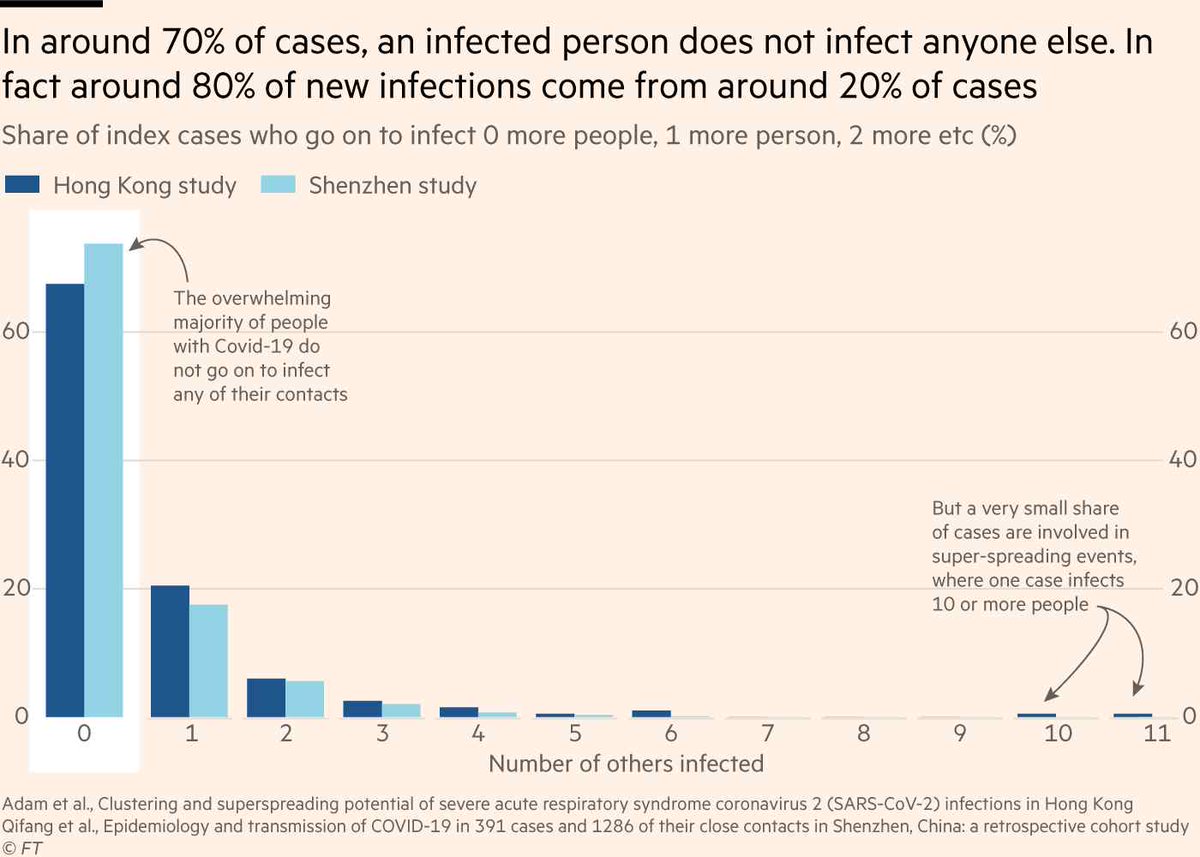
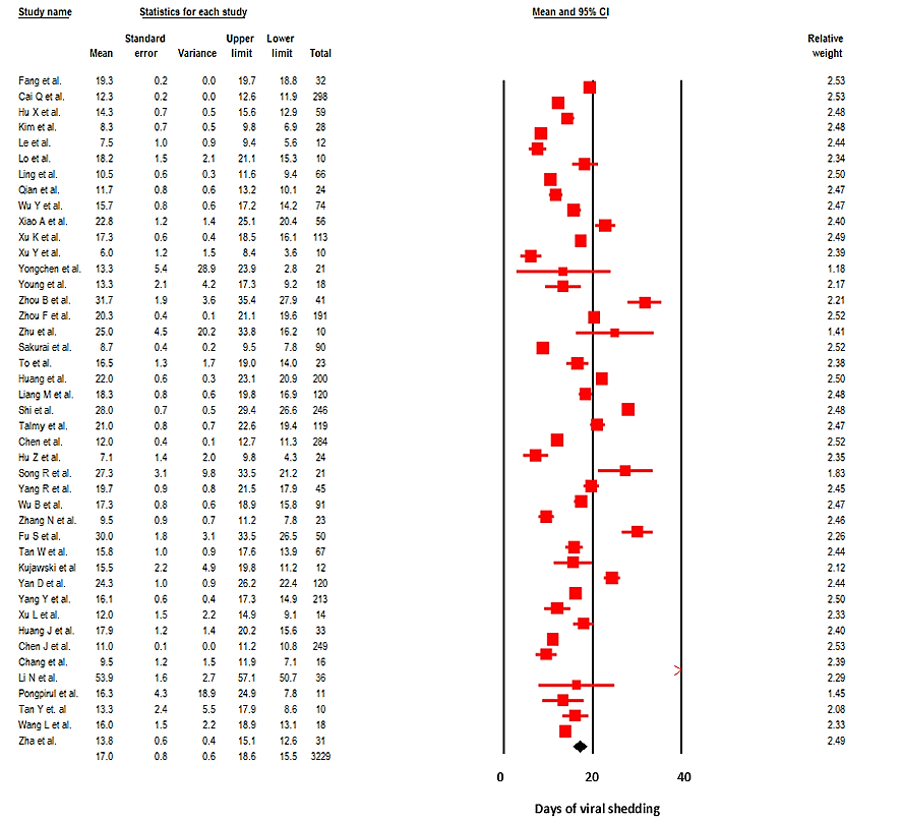
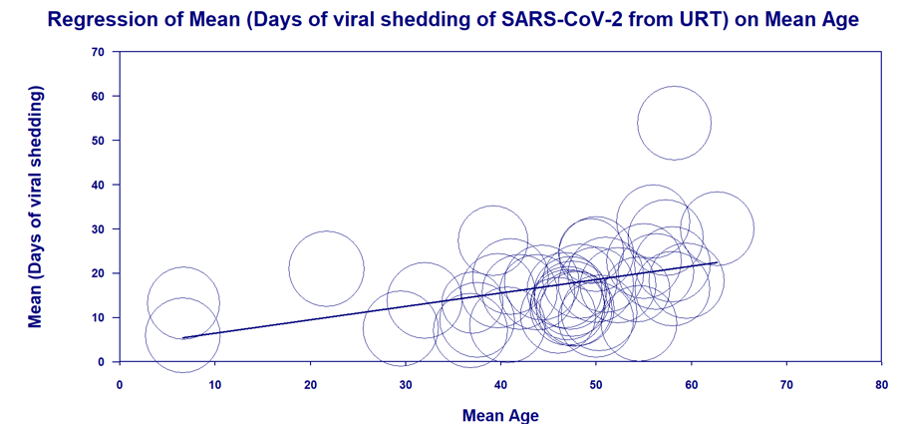
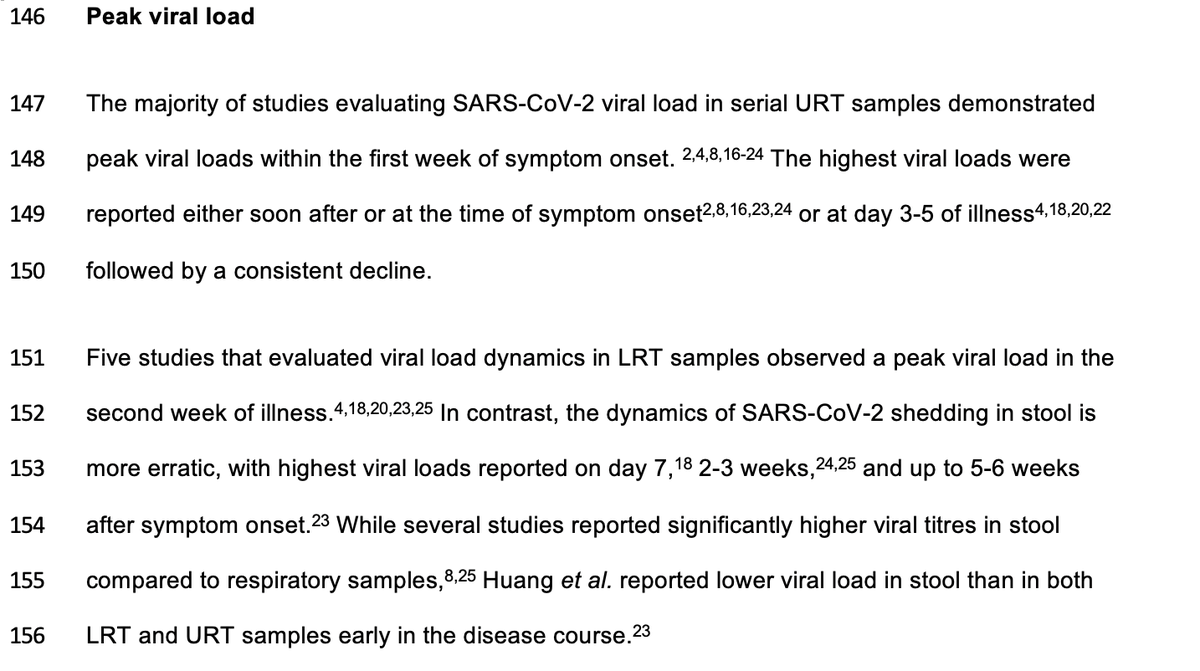
When we look at the viral load dynamics & contact tracing studies, those who are infected are very infectious for a short window, likely 1-2 days before and 5 days following symptom onset. No transmission documented so far after the first week of symptom onset. (7/n) 
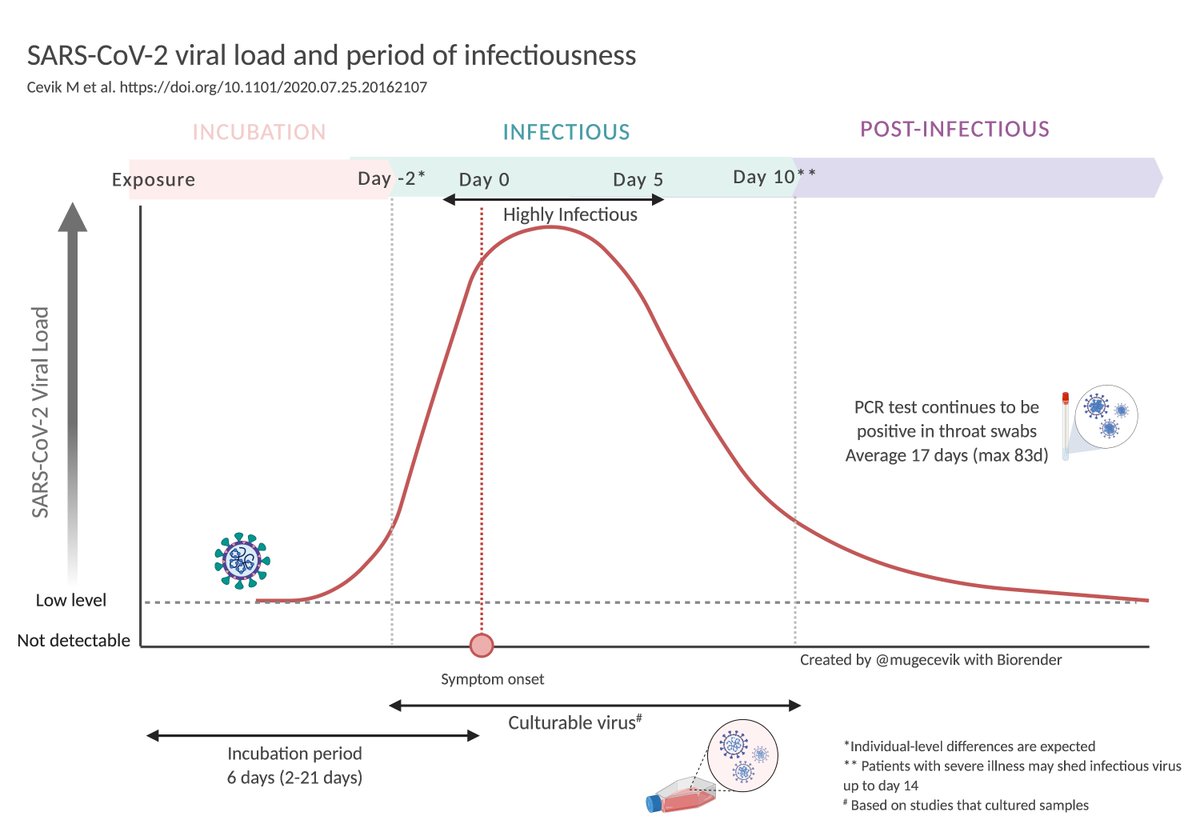
While asymptomatic patients can transmit the virus to others, emerging evidence suggests that asymptomatic index cases transmit to fewer secondary cases. Attack rates are highly correlated with symptom severity (8/n)
(medrxiv.org/content/10.110…) and (medrxiv.org/content/10.110…)
(medrxiv.org/content/10.110…) and (medrxiv.org/content/10.110…)
Transmission is also affected by other host factors, including host defence mechanisms and age. For instance, given the same exposure, susceptibility to infection increases with age, higher in > 60yo compared to younger or middle-aged adults. (9/n)
(medrxiv.org/content/10.110…)
(medrxiv.org/content/10.110…)
Environment:
Contact pattern also depends on the setting of the encounter. Contact tracing studies suggest an almost 20x higher risk of transmission indoors compared with outdoor environments. (10/n) (ft.com/content/2418ff…)
Contact pattern also depends on the setting of the encounter. Contact tracing studies suggest an almost 20x higher risk of transmission indoors compared with outdoor environments. (10/n) (ft.com/content/2418ff…)
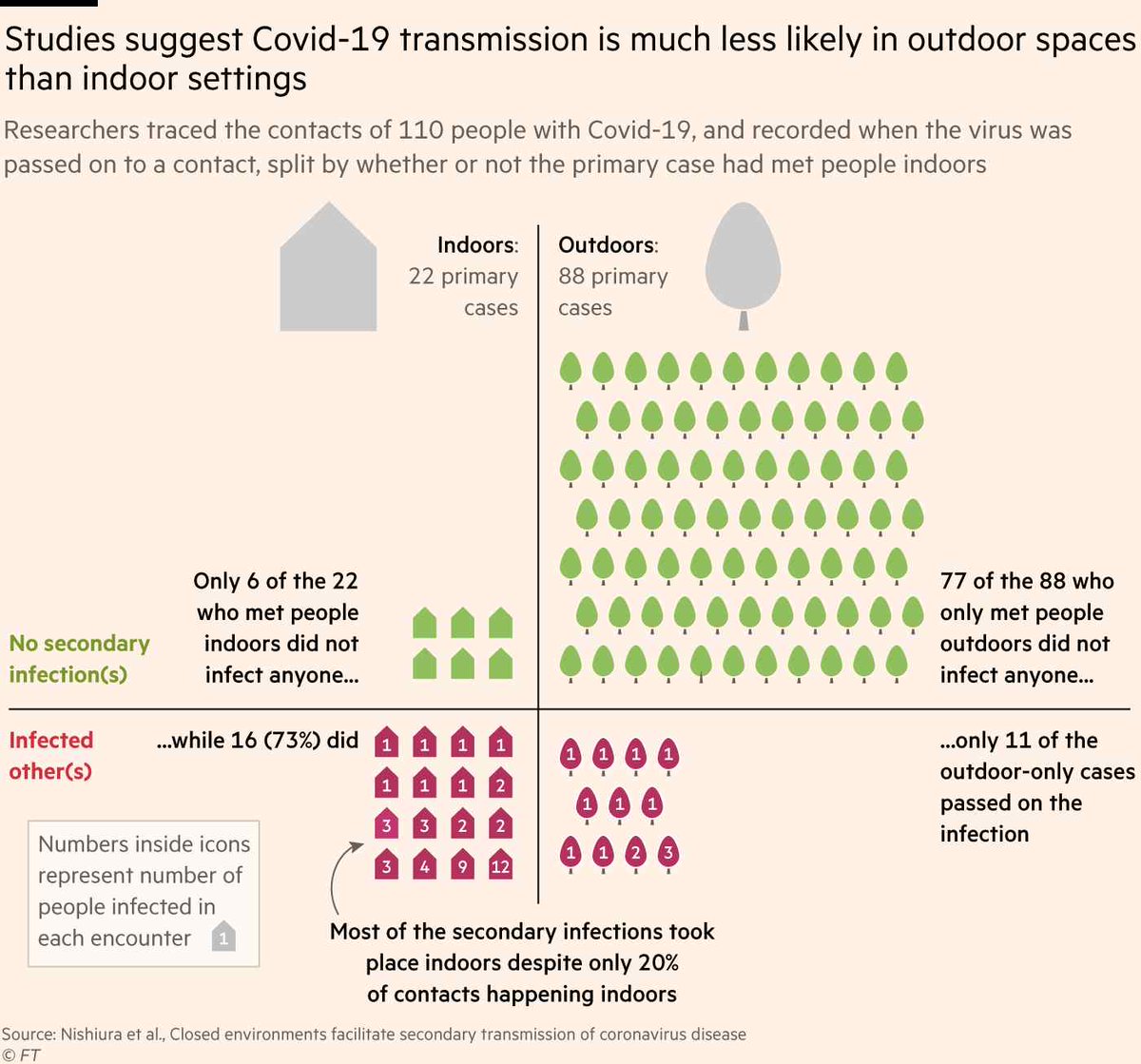
Prolonged indoor contact in a crowded and poorly ventilated environment increases the risk of transmission substantially. But decreasing occupancy and improving ventilation through opening windows/doors can lower the risk. (11/n) 
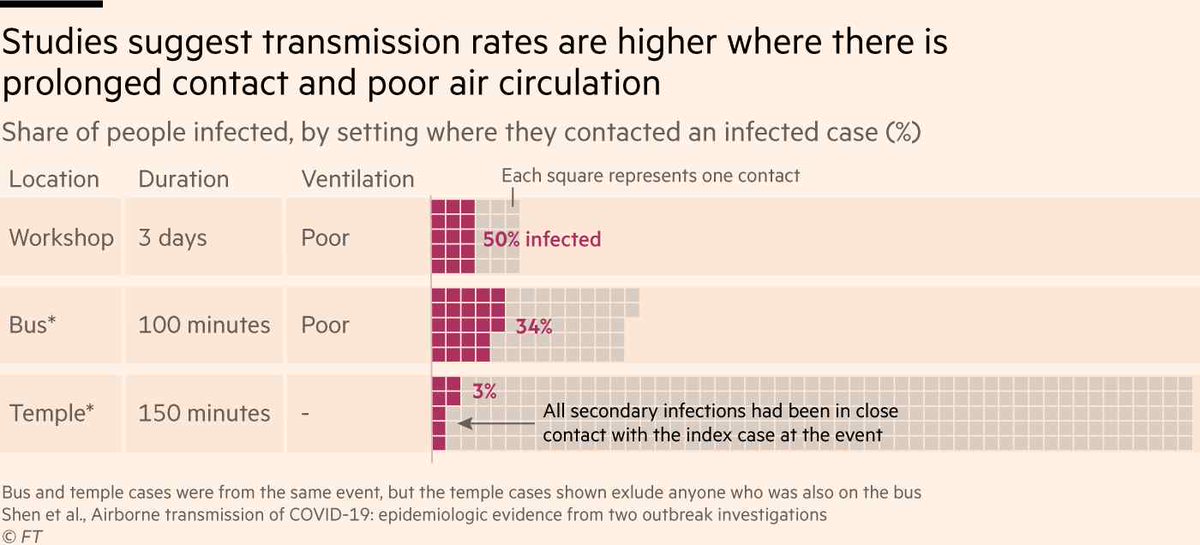
Much worryingly the largest outbreaks from across the world are reported in long term care facilities such as nursing homes, homeless shelters, prisons, and meat-packing plants where many people spend several hours working, living together, and share communal spaces. (12/n)
The largest clusters of cases observed in the USA have all been associated with prisons or jails. In the largest meat packing plant in Germany, while the common point of potential contact was workplace, risk was higher for a single shared apartment, bedroom and carpool. (13/n)
Socioeconomic factors and racial/ethnic disparities:
Global figures suggest that COVID-19 pandemic is strongly shaped by structural inequities, adverse living and working conditions and structural racism that drive household and occupational risks. (14/n)
Global figures suggest that COVID-19 pandemic is strongly shaped by structural inequities, adverse living and working conditions and structural racism that drive household and occupational risks. (14/n)
People in lower-paid occupations are often classified as essential workers who must work outside the home and may travel to work on public transport. These occupations often involve greater social mixing, exposure risk due to prolonged working hours and job insecurity. (15/n)
Households in socioeconomically deprived areas are more likely to be overcrowded, increasing the risk of transmission within the household. These disparities also shape the strong geographic heterogeneities observed in the burden of cases and deaths. (16/n)
PHE surveillance report shows that while the number of infections is increasing mainly in 20-29, 30-39 ages in England, SARS-CoV-2 is spreading most in highly deprived areas - where people are in poorly paid work and can't afford to isolate. (17/n) assets.publishing.service.gov.uk/government/upl… 
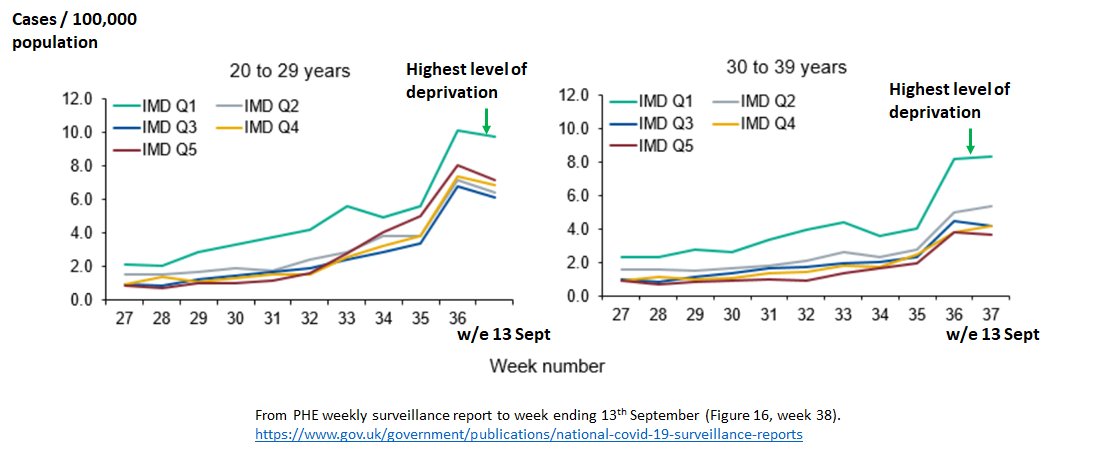
In Madrid, 37 neighbourhoods are seeing the highest incidence, 4 x the Spanish average. Common factors: these areas are poorer, denser and have a high proportion of immigrant population. (18/n)
(elpais.com/sociedad/2020-…)
(elpais.com/sociedad/2020-…)
Previous research suggests that although social distancing during the 2009 H1N1 pandemic was effective in reducing infections, this was most pronounced in households w greater socioeconomic advantage. Similar findings are emerging for COVID-19. (19/n) (pnas.org/content/117/33…)
Covid-19 could now be endemic in some parts of England that combine severe deprivation, poor housing and large BAME communities, national lockdown in these parts of the north of England had little effect in reducing the level of infections (20/n) (theguardian.com/world/2020/sep…)
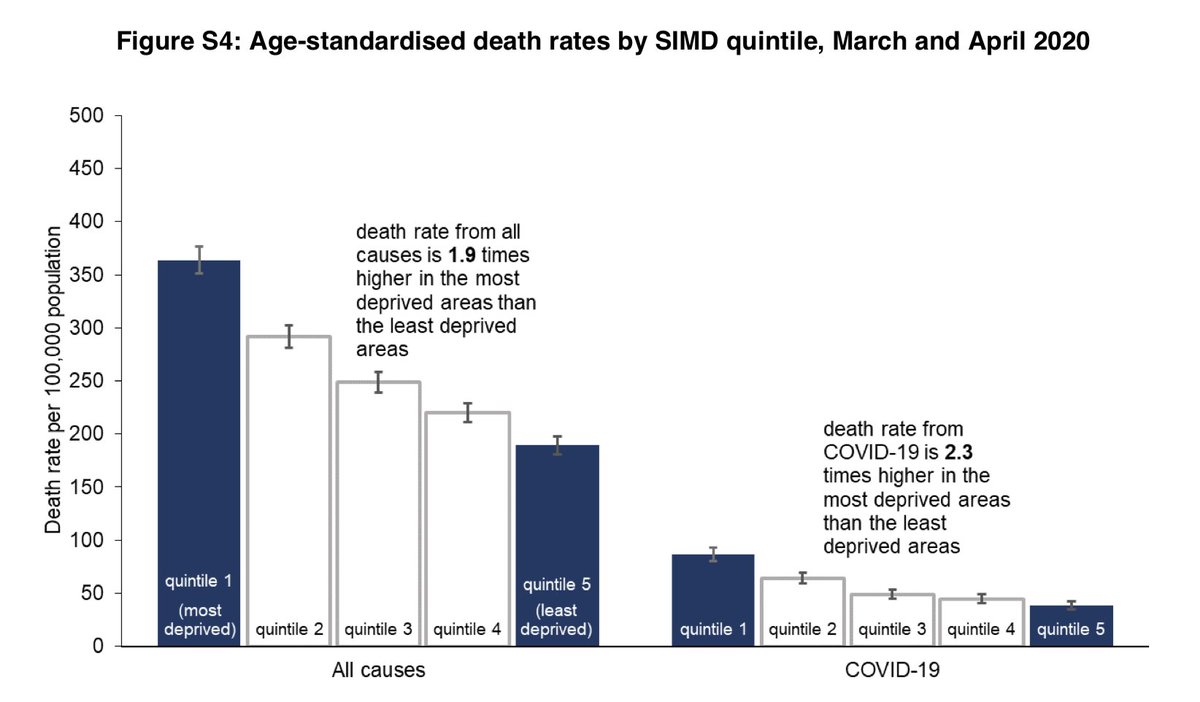
A real overlap in the causes of mortality and deprivation can be seen here. The age-standardised rate of deaths involving COVID-19 in the most deprived quintile was more than double (2.3 times higher) than in the least deprived quintile in Scotland. (21/n) nrscotland.gov.uk/files/statisti… 
In summary:
The disproportionate impact of COVID-19 on households living in poverty, and the racial and ethnic disparities observed in many countries, emphasize the need to urgently update our definition of "vulnerable" populations for COVID-19 & address these inequities. (22/n)
The disproportionate impact of COVID-19 on households living in poverty, and the racial and ethnic disparities observed in many countries, emphasize the need to urgently update our definition of "vulnerable" populations for COVID-19 & address these inequities. (22/n)
These include social and income protection and support to ensure low paid, non-salaried and zero-hours contract workers can afford to follow isolation and quarantine recommendations, provision of protective equipment for workplaces and community settings. (23/n)
Early viral load peak in the disease course indicates that preventing onward transmission requires immediate self-isolation with symptom onset (for a min of 5 days). Messages should prioritise isolation practices, and policies should include supported isolation. (24/n)
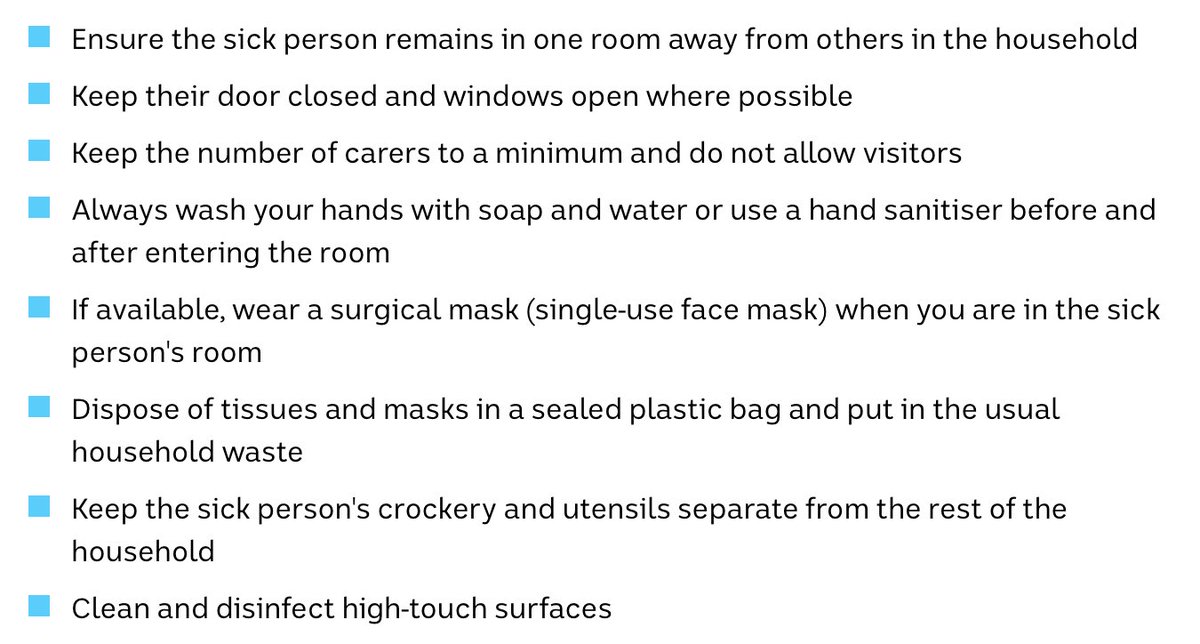
There are many things that could be done within families to decrease transmission. We need to provide clear instructions, and means of support to enable those with symptoms/positive test and their contacts to isolate. (25/n) abc.net.au/news/2020-09-1… 
Policymakers and health experts can help the public differentiate between lower-risk and higher-risk activities and environments and public health messages could convey a spectrum of risk to the public to support engagement in alternatives for safer interaction (26/n)
Avoid crowded indoor poorly ventilated environments. Spend more time outdoors. Maintain your distance (more is better but 2 metre is not a panacea). Improve ventilation: open windows/doors. Wear a mask indoors. Wash hands. (27/n) (vox.com/science-and-he…) 

Public health strategies will be needed to mitigate transmission in nursing homes, prisons and jails, shelters, meat-packing plants such as personal protective equipment and routine testing to identify infected individuals early in the disease course. (28/n)
This thread is based on our new paper with @JuliaLMarcus Caroline Buckee and @aetiology
Accepted in CID - preprint version can be accessed here: (papers.ssrn.com/sol3/papers.cf…)
Accepted in CID - preprint version can be accessed here: (papers.ssrn.com/sol3/papers.cf…)

Our article is now published online.
We argue that SARS-CoV-2 transmission dynamics should inform policy decisions about mitigation strategies for targeted interventions.
academic.oup.com/cid/advance-ar…
We argue that SARS-CoV-2 transmission dynamics should inform policy decisions about mitigation strategies for targeted interventions.
academic.oup.com/cid/advance-ar…

• • •
Missing some Tweet in this thread? You can try to
force a refresh