COVID-19: An EBM Take Part 1 at #ACOEP20
-When to Change Practice
-N95 Reuse
-Corticosteroids
-Remdesivir
-Convalescent Plasma
#FOAMed #FOAMcc
-When to Change Practice
-N95 Reuse
-Corticosteroids
-Remdesivir
-Convalescent Plasma
#FOAMed #FOAMcc

When to Change Practice
Expedited thirst for info & rapidity of pandemic lead to abbreviated peer review, publication of unvalidated data, retraction, and dissemination through press release
When to change = multidisciplinary discussion to set standard care at each institution
Expedited thirst for info & rapidity of pandemic lead to abbreviated peer review, publication of unvalidated data, retraction, and dissemination through press release
When to change = multidisciplinary discussion to set standard care at each institution

N95 Decontamination and Reuse
Make sure technique kills virus BUT doesn't affect filtration or fit
Best options: Vaporized H202, UV Light 260 - 285nm, or Time based strategy
2nd Best options: Autoclave 121C or Dry Heat 70C
Not an Option: 70% Ethanol
Make sure technique kills virus BUT doesn't affect filtration or fit
Best options: Vaporized H202, UV Light 260 - 285nm, or Time based strategy
2nd Best options: Autoclave 121C or Dry Heat 70C
Not an Option: 70% Ethanol

Remdesivir = "An expensive Tamiflu"
-Decreases duration of symptoms, has no effect on mortality, and has side effects (i.e. AKI)
-$3100 per 5d course
-Small window of therapeutics (i.e. low flow O2)

-Decreases duration of symptoms, has no effect on mortality, and has side effects (i.e. AKI)
-$3100 per 5d course
-Small window of therapeutics (i.e. low flow O2)


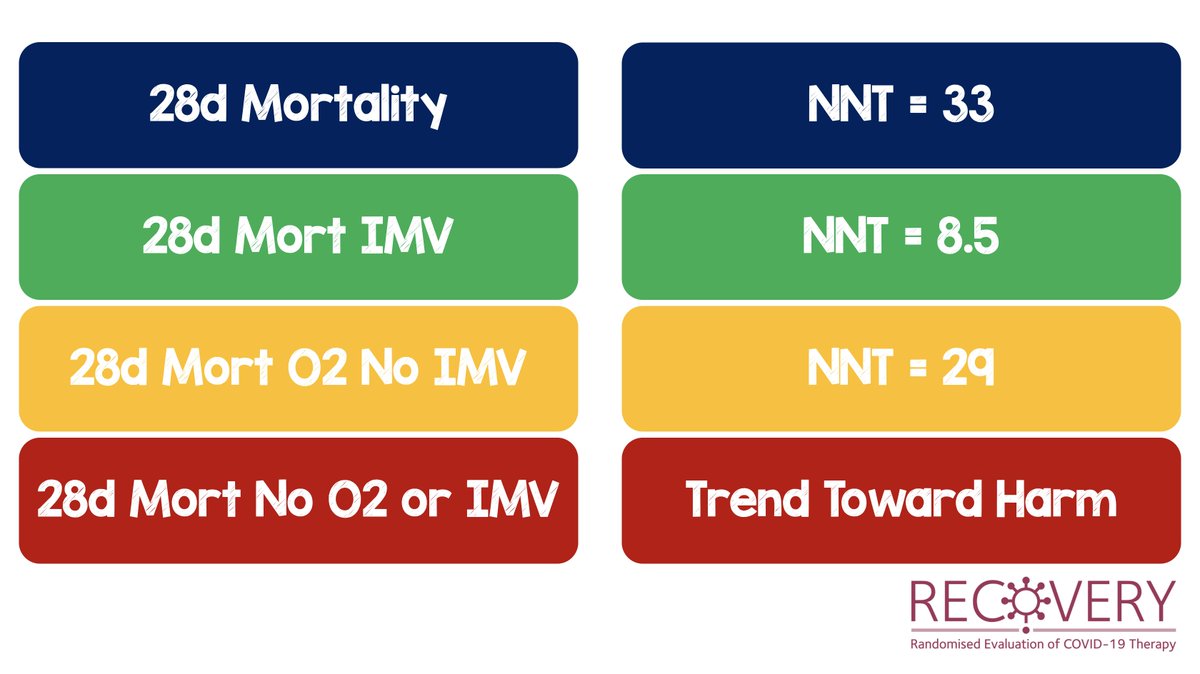
Corticosteroids Superior to Placebo in #COVID19
-Overall 28d Mortality NNT = 33
-IMV 28d Mortality NNT = 8.5
-O2 BUT no IMV Mortality NNT = 29
-No O2 or IMV Mortality = Trend Toward Harm
-Overall 28d Mortality NNT = 33
-IMV 28d Mortality NNT = 8.5
-O2 BUT no IMV Mortality NNT = 29
-No O2 or IMV Mortality = Trend Toward Harm
Convalescent Plasma in #COVID19
-US Expanded Access Program (>35k pts)
-No Placebo arm
-Earlier better than later
-Higher IgG titer better than lower IgG titer
-US Expanded Access Program (>35k pts)
-No Placebo arm
-Earlier better than later
-Higher IgG titer better than lower IgG titer

Interesting trends in #COVID19 from April 2020 to July 2020
-Decrease in IMV
-Decrease in HCQ use
-Increase in Remdesivir
-No Change in steroid use (although I suspect now this number would be higher)
-Decrease in IMV
-Decrease in HCQ use
-Increase in Remdesivir
-No Change in steroid use (although I suspect now this number would be higher)

• • •
Missing some Tweet in this thread? You can try to
force a refresh