1/ Have you ever heard your friendly pulmonologist use the terms “entrapped” or “trapped” lung and were confused about the terminology? If so you are not alone and this is the tweetorial for you! #MedTwitter #tweetorial @crit_caring_MD @lkbrath @VCU_PCCM @PSinkam 


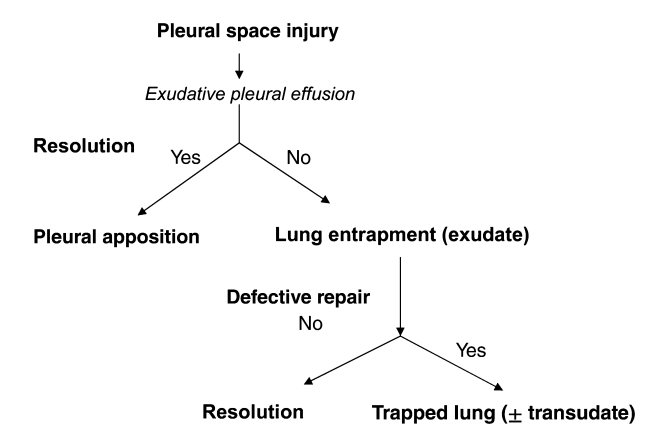
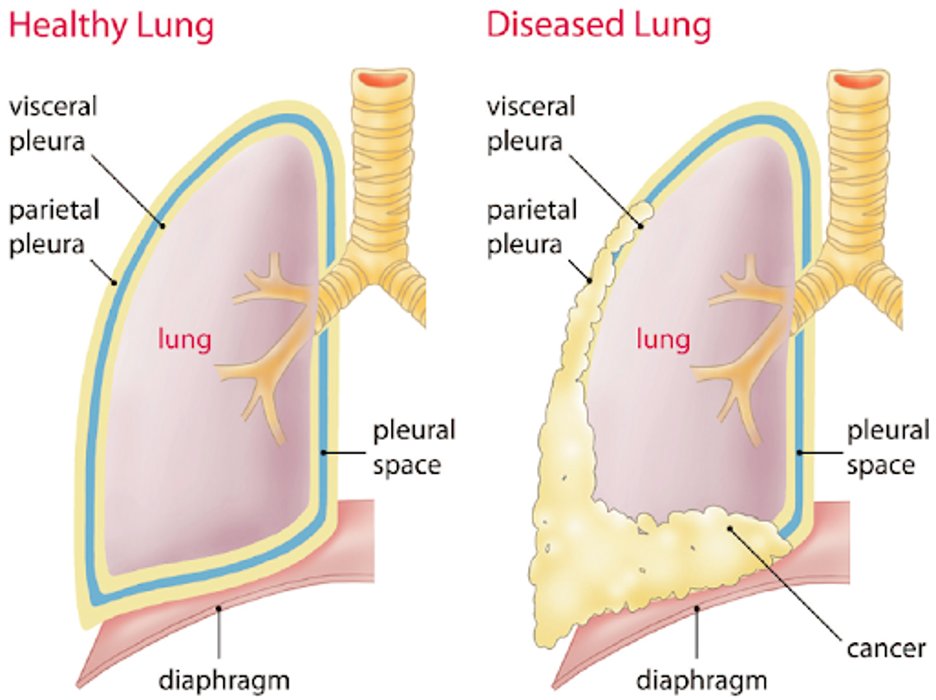
2/Let’s first start with some definitions. The term “non-expandable lung” is an umbrella term that is used to describe when the lung is unable to expand to the chest wall in order to achieve visceral and parietal pleura apposition. @AvrahamCooperMD @michellebr00ks @mdlizs 

3/There are two pleural diseases that result in the “non-expandable lung”:
1⃣Lung Entrapment
2⃣Trapped Lung
@cjchiu @mkashiouris @AdamRodmanMD @ptfaddenMD @rabihmgeha @DxRxEdu @VCU_IMRes
1⃣Lung Entrapment
2⃣Trapped Lung
@cjchiu @mkashiouris @AdamRodmanMD @ptfaddenMD @rabihmgeha @DxRxEdu @VCU_IMRes
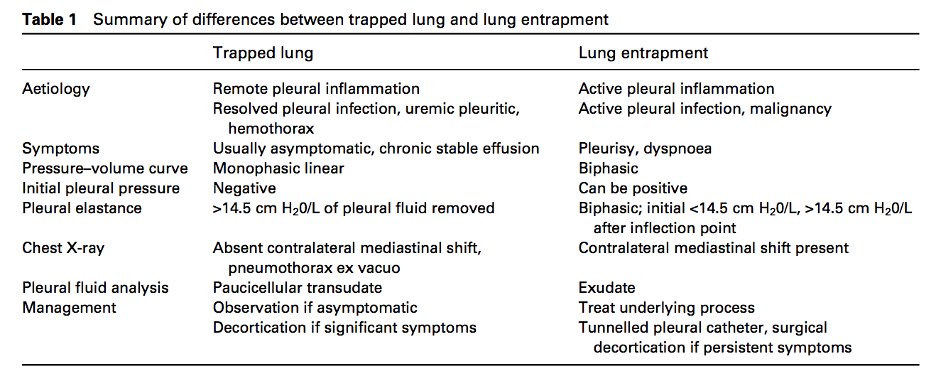
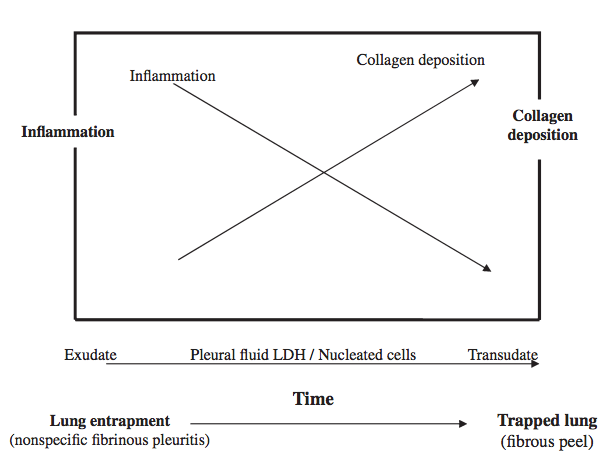
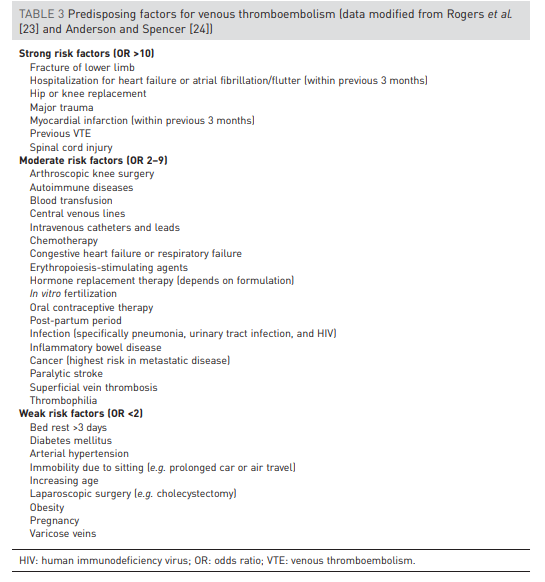
4/Lung entrapment is when the lung cannot fully expand due to an active disease that restricts the expansion of the lung and/or visceral pleura. This is typically associated with an exudative effusion. @tony_breu @KevinSwiatek 
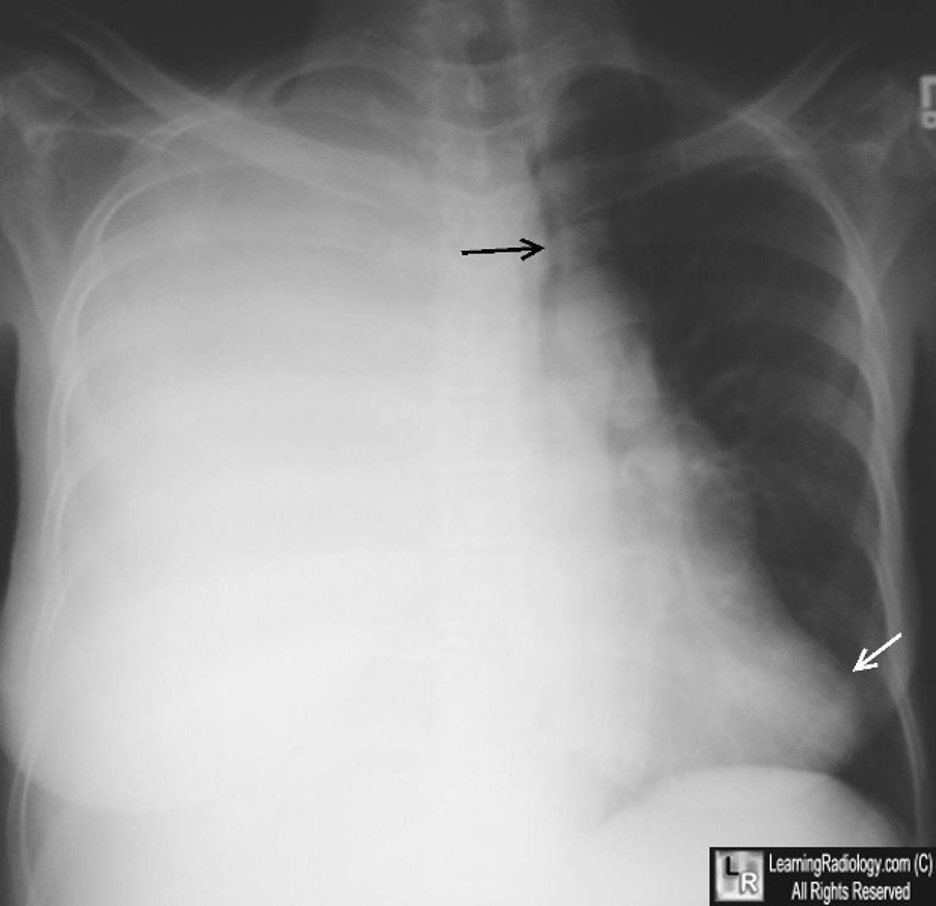
5/ Trapped lung is when the lung cannot expand due to a remote inflammatory condition that leaves a collagenous or fibrinous peel on the viscera pleura that prevents lung expansion. The pleural fluid can be transudative or exudative. @scall1200 @cderekleiner @rva_IntMedPD 

6/Let’s dive into lung entrapment. The most common cause of lung entrapment is due to pleural malignancy with an estimated 30% of malignant effusions leading to lung entrapment. However, pleural infections or inflammation can also lead to lung entrapment. 
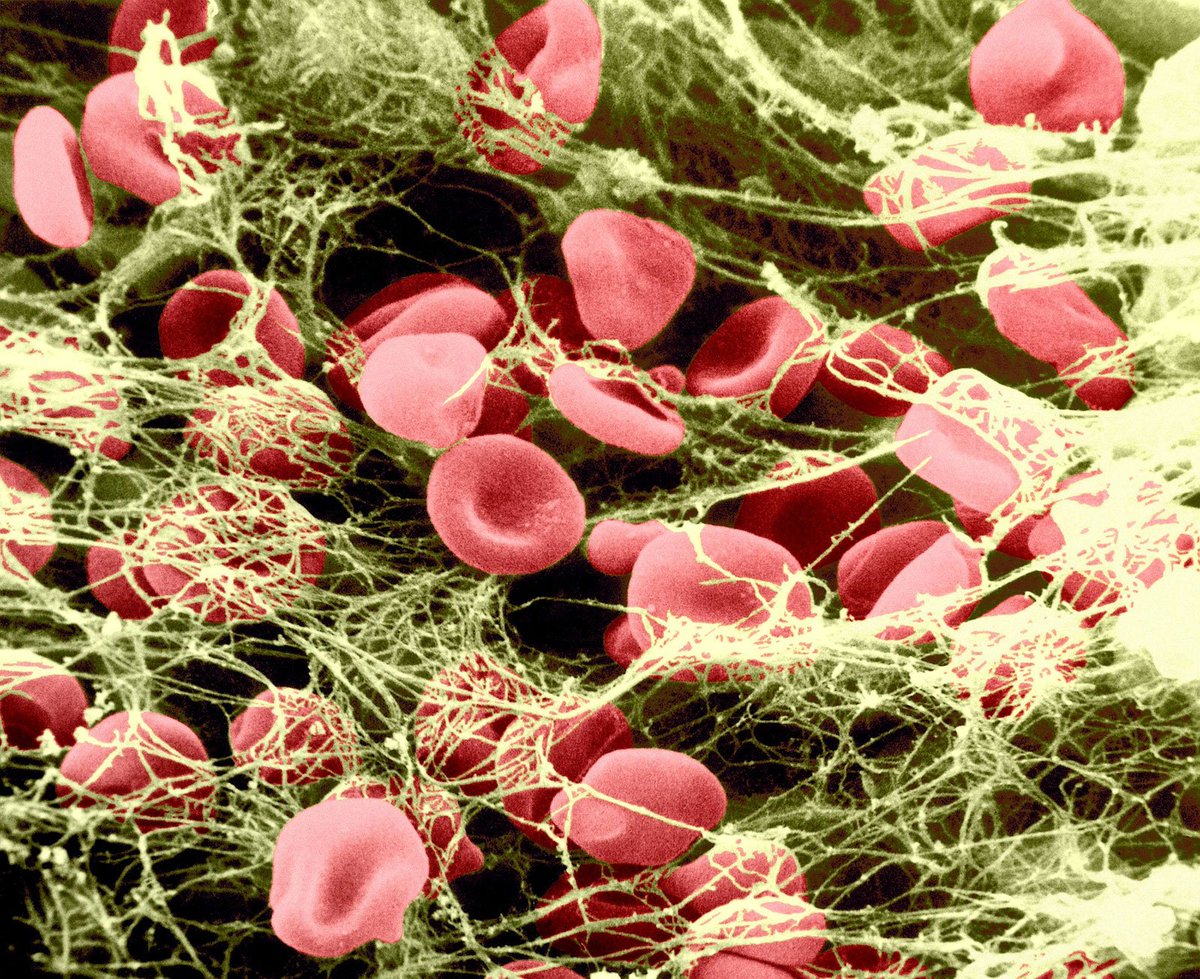
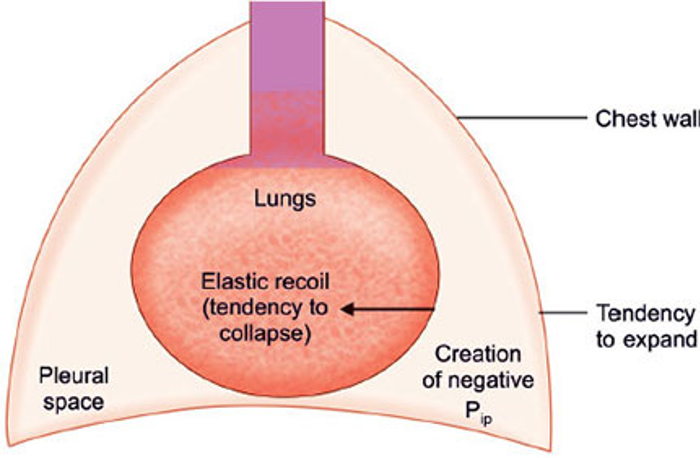
7/In pleural malignancy, there is an ⬆️in capillary leakiness with ⬇️ clearance by the lymphatics located on the parietal pleura due to malignant infiltration. Fluid will continue to accumulate until there is an equilibrium of oncotic and hydrostatic pressures across the pleura. 
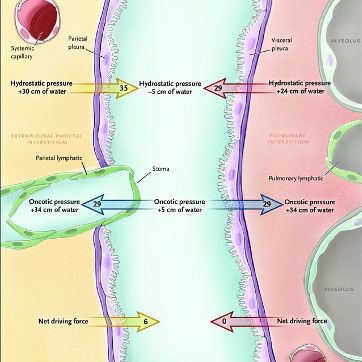
8/ Lung entrapment secondary to an infectious process is typically due to an increase in the elastic recoil of the atelectatic/consolidated lung with an increase in pleural fluid production from the visceral pleura. 
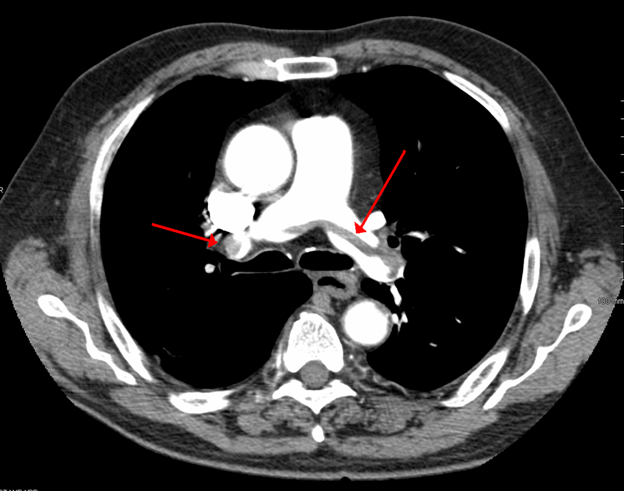
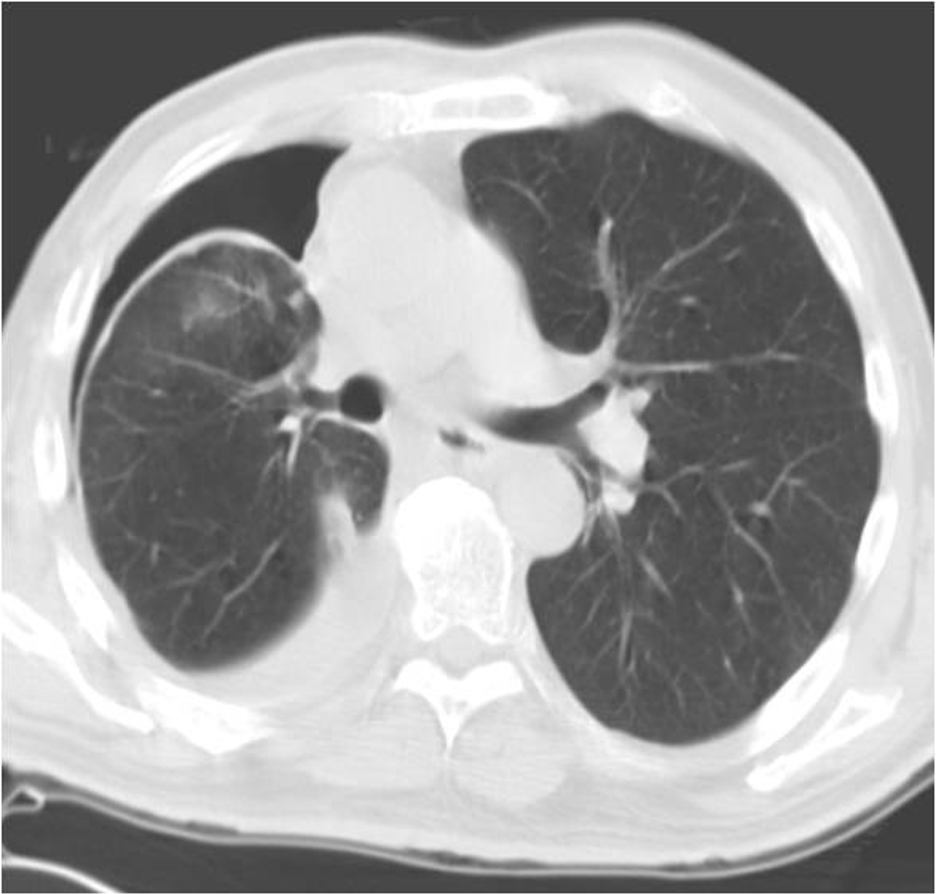
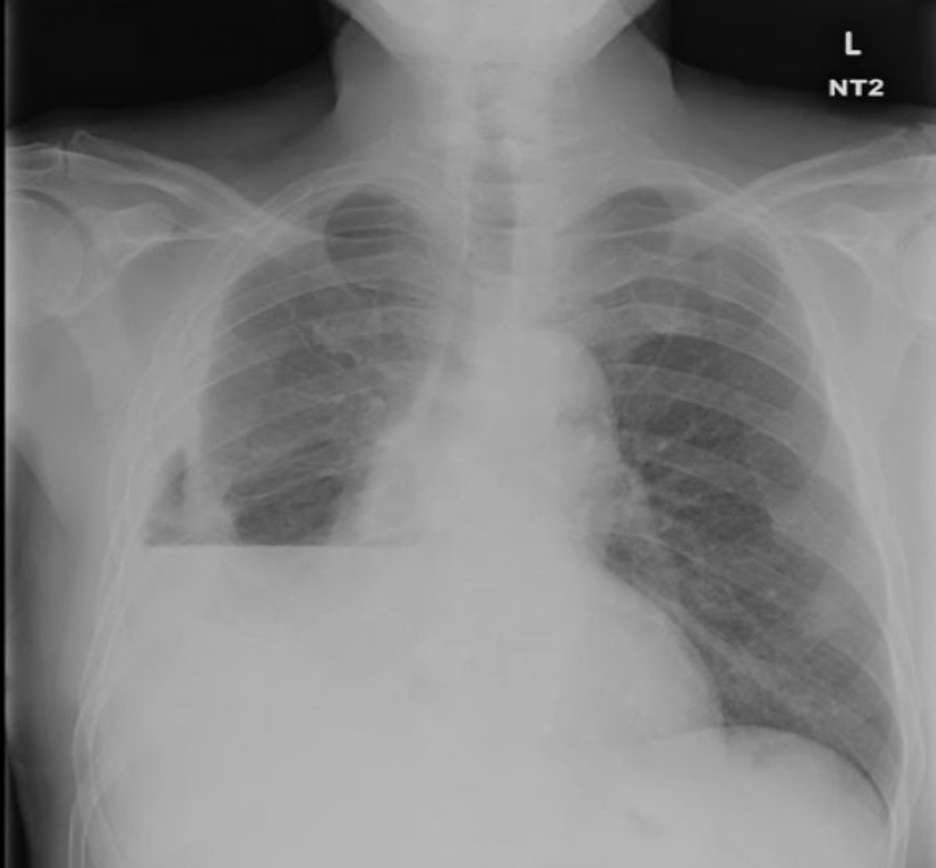
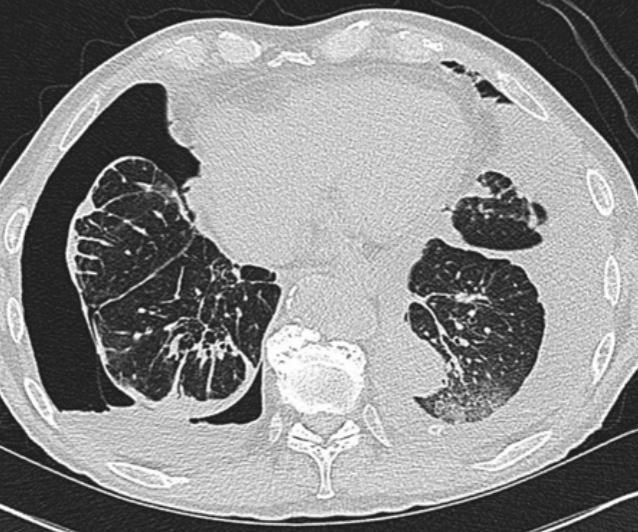
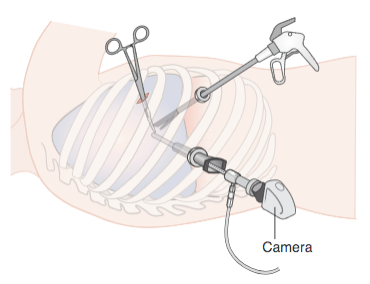
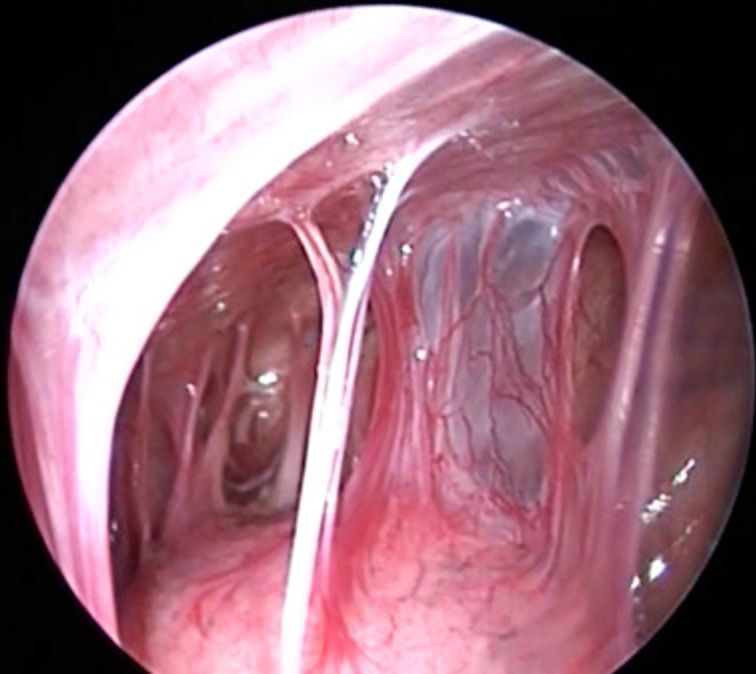
9/ One of the 🔑 features of lung entrapment is an improvement in dyspnea following a thoracentesis. However, the lung does not fully expand radiographically following the procedure. CT imaging may show a visceral pleura that appears thickened, nodular, or hyperechoic.
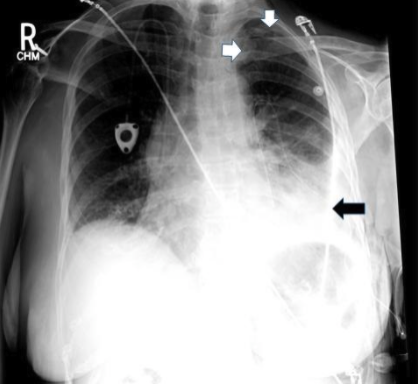
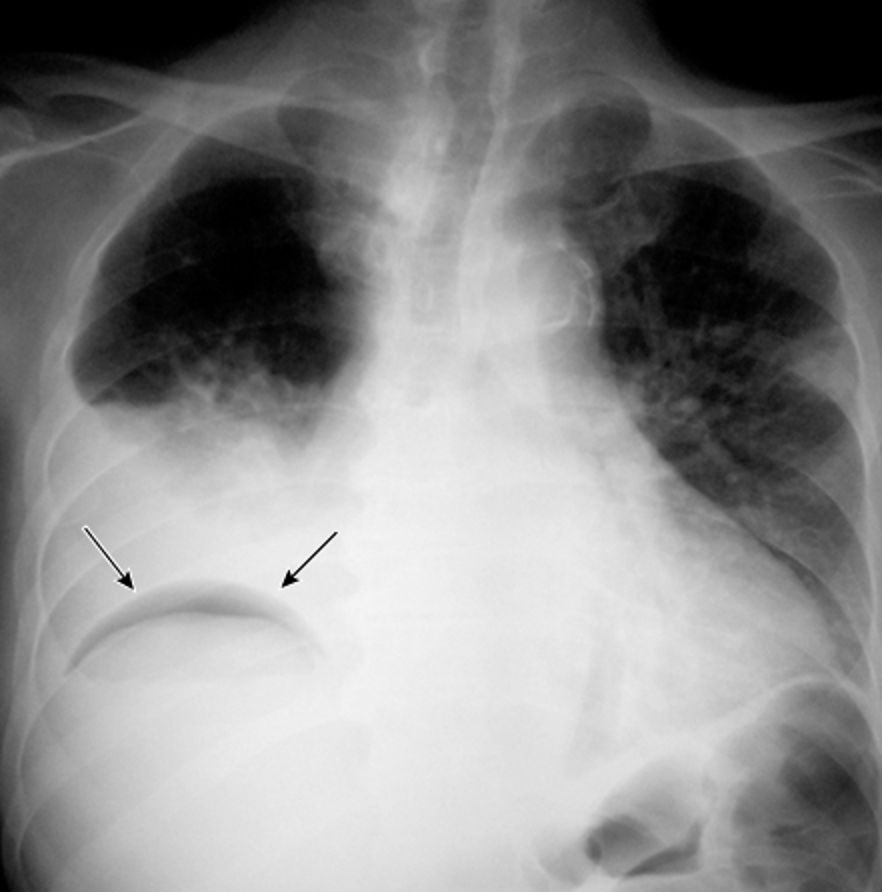
10/ With large pleural effusions, you typically get a contralateral shift of the mediastinum. However, with lung entrapment you will typically see the mediastinum shift ipsilaterally of the effusion or no shift at all. @CritCareMed @PulmCrit @MedEdPGH @gradydoctor 

11/ The overarching goal of treatment for lung entrapment is to treat the underlying cause, i.e. infection, inflammation, or malignancy as most lung entrapment will resolve with treatment.
12/In trapped lung, the fibrotic process affecting the visceral pleura causes an increase in the negative pleural pressure resulting in fluid accumulation and reduction in the removal of fluid by pleural lymphatics. @UpToDate @gsmartinmd @jackpenner 
13/Interestingly, most patients with trapped lung do not have symptoms related to their pleural effusion and will typically have discomfort throughout a thoracentesis due to further reductions in their intrathoracic pressure. @bqueenhoo @palettala @TheRealDSrini
14/Imaging of trapped lung will typically show pleural thickening and loculation. An air contrasted CT can be used to better visualize the visceral pleura rind or you can use direct visualization with video-assisted thoracoscopy. @ReenaHem @ERitterMD @VCURadRes @MarkZieglerMD 

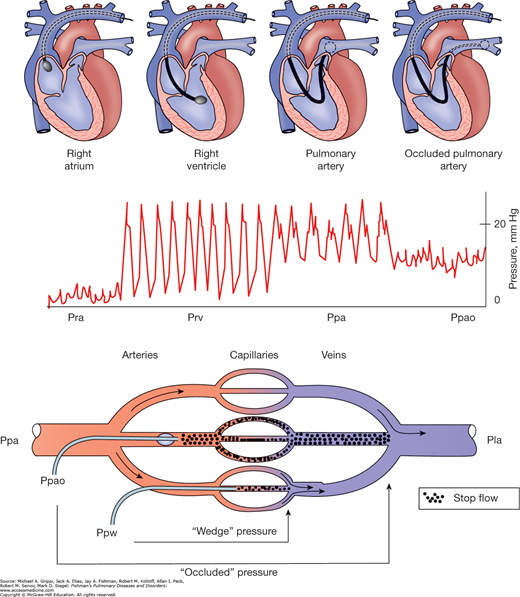
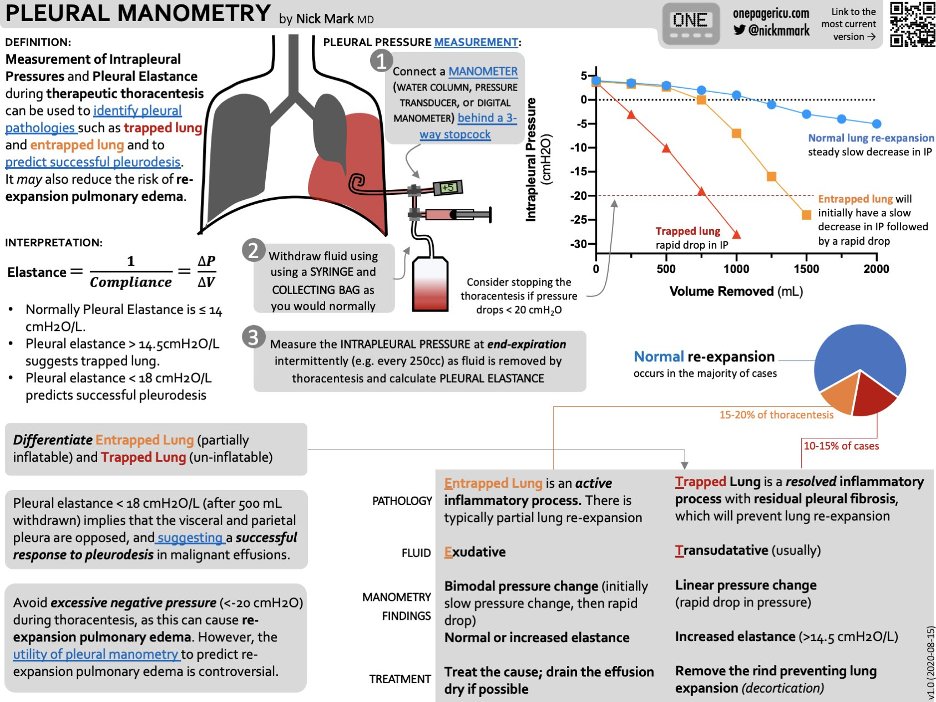
15/Another handy trick is with pleural manometry. In trapped lung you will see the pressure decrease quickly as pleural fluid is being withdrawn while in lung entrapment it will be more gradual. Check out this chart on pleural manometry by @nickmmark ! 
16/ Management of an asymptomatic trapped lung is NOT pleural drainage as the effusion will just re-accumulate. However, decortication of the visceral pleura rind with VATS is typically your treatment for symptomatic patients who are surgical candidates. @VCUIMClerkship 

17/ Trapped lung and lung entrapment should not be confused with pneumothorax ex vacuo, which is an acute bronchial obstruction that leads to lobar collapse with a marked increase in negative pleural pressure. Treatment is removal of the obstruction and NOT a chest tube. 
• • •
Missing some Tweet in this thread? You can try to
force a refresh