
#ACR20 Evaluation and Treatment of Systemic Sclerosis-ILD in the New Decade with Dr. Anna Hoffmann-Vold
(a live-tweet)
(a live-tweet)
Some background facts all rheumatologists need to know:
👉ILD often arises early in the course of SSc
👉Not just in dcSSc, or just with Scl70 Ab
👉MAJOR cause of morbidity and mortality, even when degree of fibrosis is not severe
👉ILD often arises early in the course of SSc
👉Not just in dcSSc, or just with Scl70 Ab
👉MAJOR cause of morbidity and mortality, even when degree of fibrosis is not severe

Screen for this with HRCT. PFTs alone will miss most cases of SSc-ILD!
Many SSc-ILD patients are stable over time. But about a quarter of patients have moderate or significant decline. 

How do you know when you patient with SSc-ILD is getting worse? It's not just PFTs! Combine PFT changes with CT changes, 6MWT, and symptoms. 

Dr. Hoffman-Vold's summary of identifying and monitoring SSc-ILD below.
Key point--there's no exit from the algorithm! You should always continue monitoring for development of ILD.
Key point--there's no exit from the algorithm! You should always continue monitoring for development of ILD.

And now on to the treatment of SSc-ILD with Dr. Richard Silver.
Some major RCTs:
Scleroderma Lung Study I: The OG! Cyclophosphamide vs placebo. CYC improved FVC, TLC, dyspnea, and skin score.
Unfortunately not necessarily a durable treatment--by 24 months after treatment, most improvements had been lost again.
Scleroderma Lung Study I: The OG! Cyclophosphamide vs placebo. CYC improved FVC, TLC, dyspnea, and skin score.
Unfortunately not necessarily a durable treatment--by 24 months after treatment, most improvements had been lost again.
Scleroderma Lung Study II: MMF vs CYC. MMF non-inferior and better tolerated.
SENSCIS: Nintedanib vs placebo. About half of patients in both groups got MMF. Nintedanib (an antifibrotic) reduced rate of FVC decline--especially when combined with MMF. Lots of diarrhea+weight loss
SENSCIS: Nintedanib vs placebo. About half of patients in both groups got MMF. Nintedanib (an antifibrotic) reduced rate of FVC decline--especially when combined with MMF. Lots of diarrhea+weight loss
Scleroderma Lung Study III: MMF or up-front treatment with MMF + pirfenidone. Results to come!
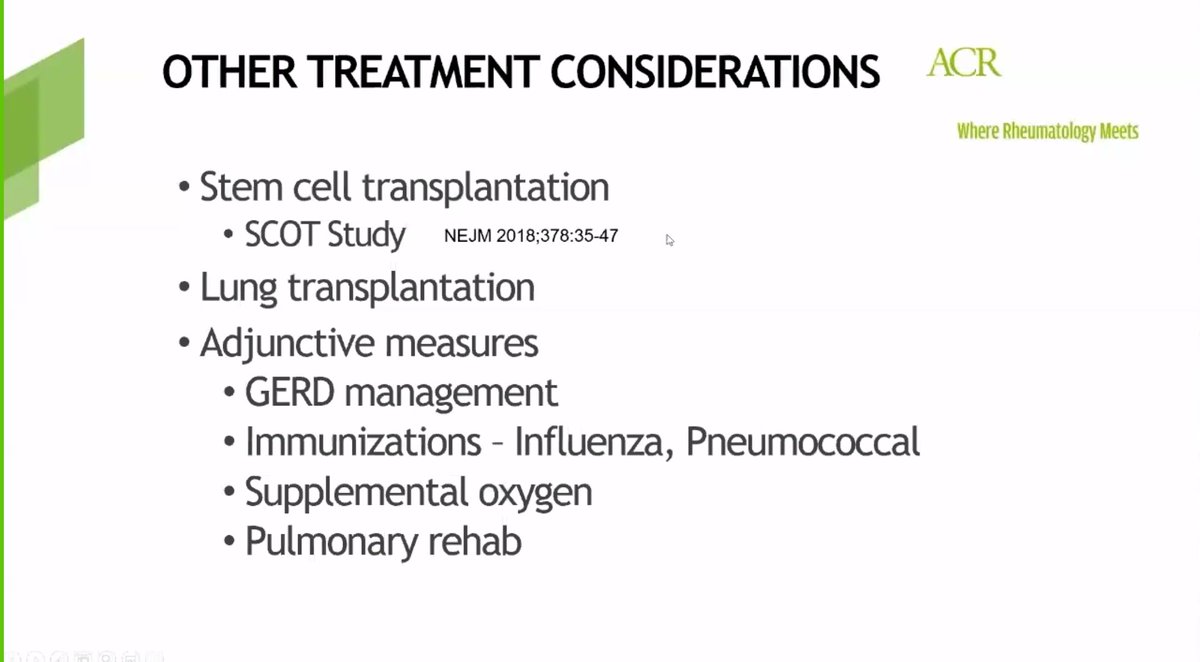
Other options: stem cell transplant, lung transplant.
Don't forget adjunct measures: GERD treatment, vaccines, pulmonary rehab!
Don't forget adjunct measures: GERD treatment, vaccines, pulmonary rehab!
Dr. Silver's treatment algorithm for SSc-ILD.
Often start with monotherapy but can consider combination therapy up front. He favors immunosuppression if GGO are present (GGO=inflammation, not fibrosis), and nintedanib if fibrosis only on HRCT.
#ACR20 #ACRambassador
Often start with monotherapy but can consider combination therapy up front. He favors immunosuppression if GGO are present (GGO=inflammation, not fibrosis), and nintedanib if fibrosis only on HRCT.
#ACR20 #ACRambassador

So many exciting advances in SSc-ILD!
-Increased awareness leading to earlier diagnosis
-Improving monitoring for patients with SSc-ILD
-More RCTs are coming and may expand our treatment algorithm
#ACR20 #SSc #rheumtwitter #ILDtwitter
-Increased awareness leading to earlier diagnosis
-Improving monitoring for patients with SSc-ILD
-More RCTs are coming and may expand our treatment algorithm
#ACR20 #SSc #rheumtwitter #ILDtwitter
• • •
Missing some Tweet in this thread? You can try to
force a refresh





