
Will do a thread today explaining the different types of covid tests, how they work, and what this means for false positives/negatives. fortune.com/2020/11/13/elo…
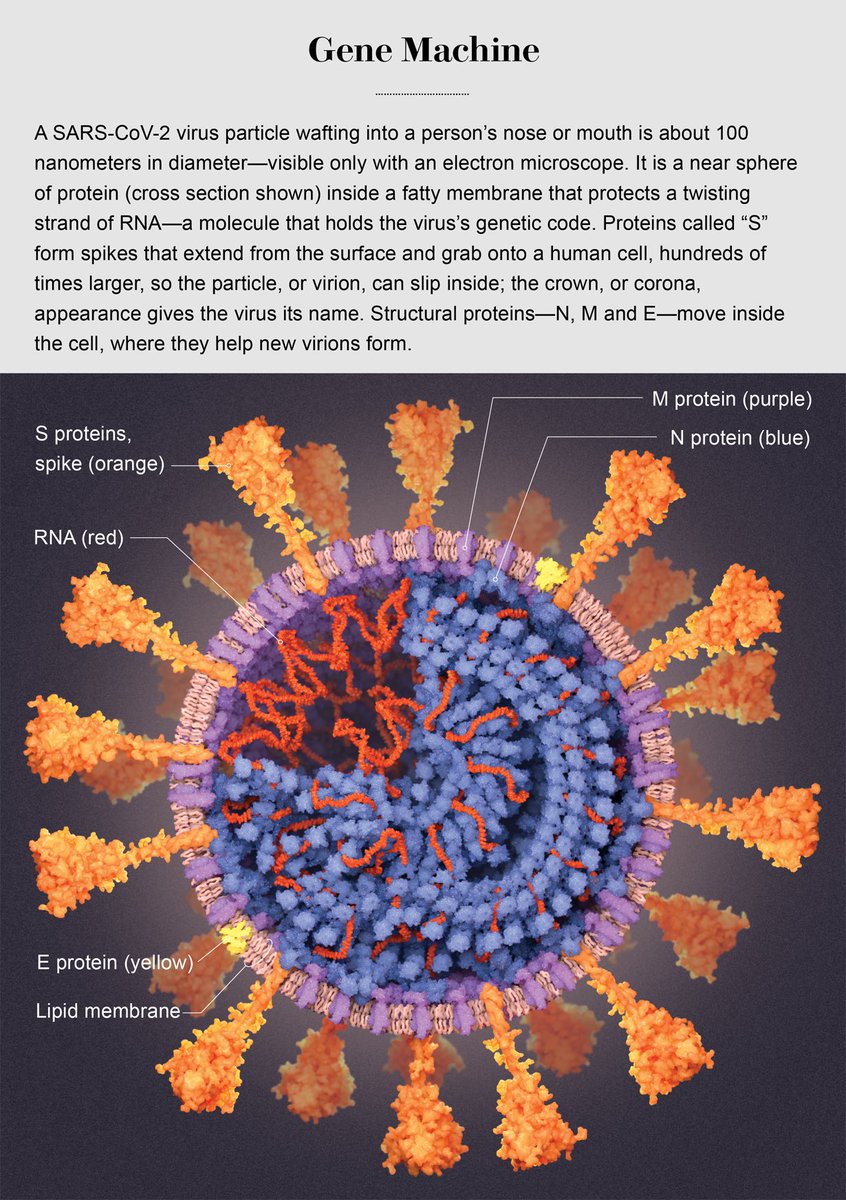
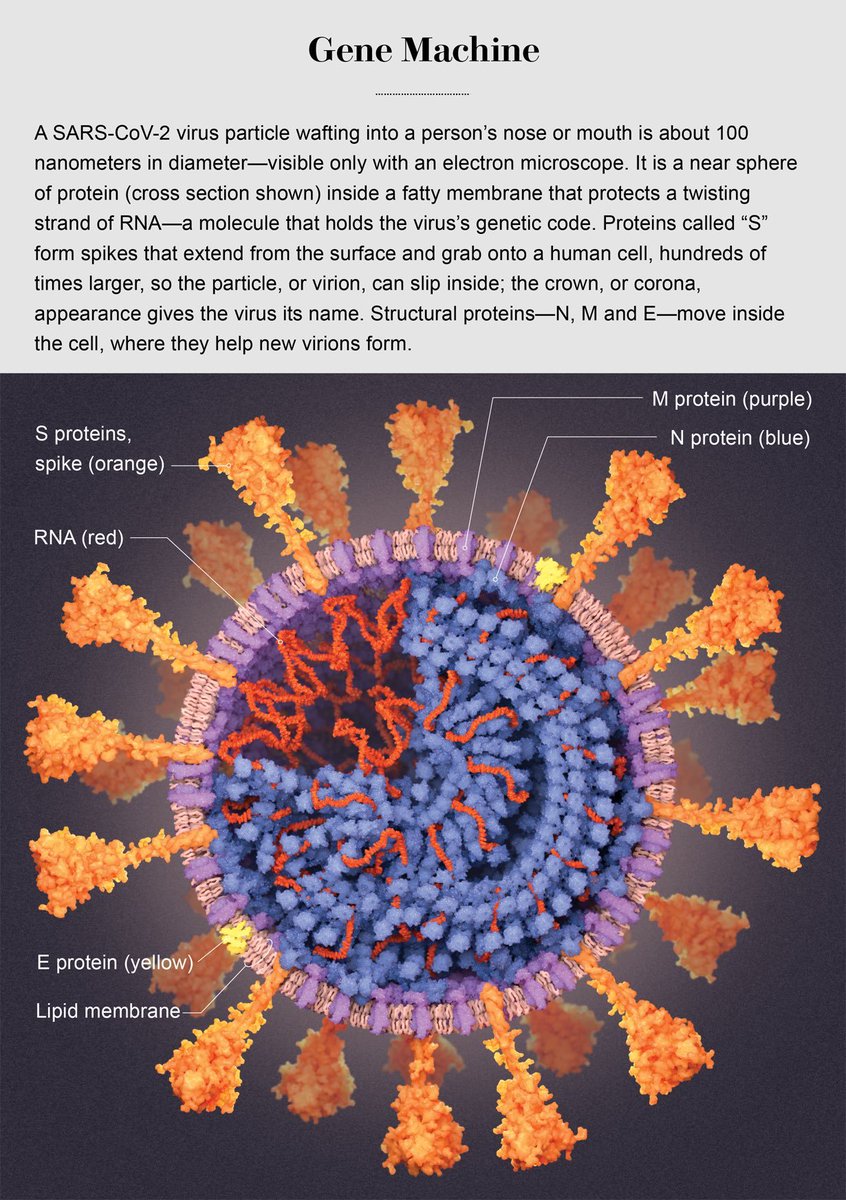
The first thing is to see what this virus is- at its core, it stores its genetic material, RNA (no DNA). This RNA is the blueprint for all of the proteins shown in this picture: N which wraps the RNA, the spike which sticks out from the virus and binds host cells, M, E etc. 
Sorry, quick caffeine break. I overestimated my Saturday morning energy levels.
The most commonly and widely used diagnostic test is the PCR nasal swab/spit test, and it takes about 1 day to get your results.
This checks: does this patient have the virus RNA?
Nice video showing the protocol here:
This checks: does this patient have the virus RNA?
Nice video showing the protocol here:
One challenge is that each testing center in the country (and globally) is not using the same PCR test.
What this means is that, out of the ~30,000 nt large SARS-CoV-2 RNA genome, different PCR tests target different genes/regions.
What this means is that, out of the ~30,000 nt large SARS-CoV-2 RNA genome, different PCR tests target different genes/regions.
There are literally hundreds of different diagnostic PCR primers and probes that target different parts of the SARS2 RNA - developed by different countries, companies, and CDCs.
It is also up to each testing center how many sets of primers+probes they use in their PCR tests.
It is also up to each testing center how many sets of primers+probes they use in their PCR tests.
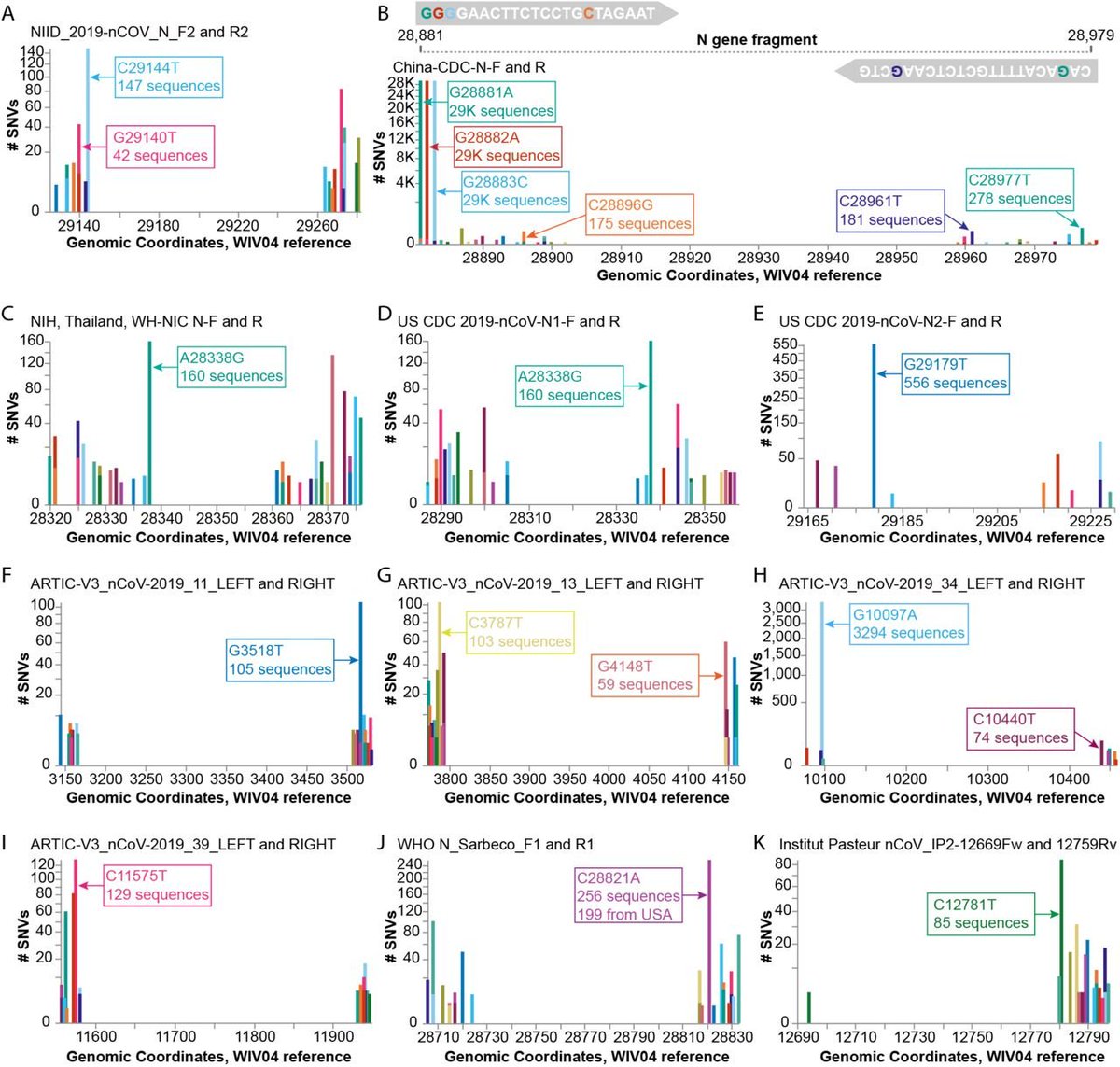
Here, using @covidcg covidcg.org I have selected the 9 US CDC primers+probes targeting the N gene (the RNA that encodes the N protein) - and I can see all of the mutations detected in North America isolates of the virus, mapped onto the targeted part of the genome. 

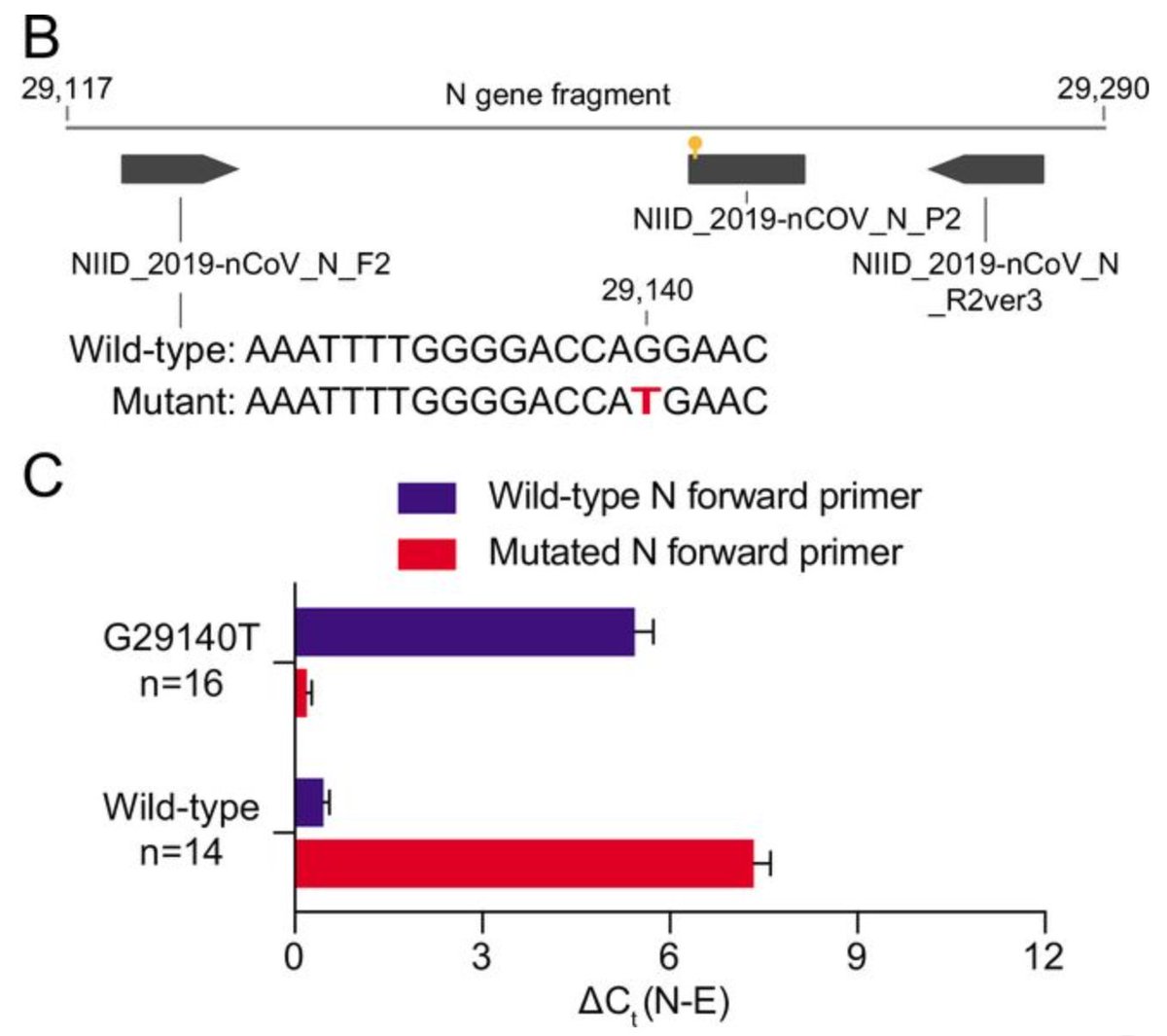
A recent preprint showed that a common G29140T mutation found in 22.3% of their samples from Madera County, California, adversely affected SARS-CoV-2 detection (~30-fold drop) by the diagnostic primer used at their sequencing center. biorxiv.org/content/10.110…
What this means is that if the SARS-CoV-2 variant(s) circulating in your community is sufficiently different from the original Dec 2019 Wuhan variant that many companies have based their PCR test design on - the false negative rate could rise.
Vanaerschot et al. show that a single mutation (that red T) in one of their primers could lead to a Ct change of +5 (compare the purple bars in their figure 1C).
biorxiv.org/content/10.110…
biorxiv.org/content/10.110…
So the risk here is, if there are testing centers that are only using 1 set of diagnostic PCR primers+probes (targeting 1 region in the genome), they could have increasing false negatives as the virus naturally mutates over time and transmission.
In our @covidcg preprint, we point out that "at least ten other primer pairs could potentially be at risk in different geographical regions due to SNVs that appear proximal to the 3’ ends of primers" (see figure 3) biorxiv.org/content/10.110… 
This is why it is super important for diagnostic developers to closely watch emerging mutations in SARS-CoV-2 in both a date range and geographical location specific manner.
They need to continuously QC their diagnostic on currently circulating variants of SARS2 in their area.
They need to continuously QC their diagnostic on currently circulating variants of SARS2 in their area.
What do people mean by false positive or false negative? And why are false negatives much more risky?
A false positive = someone who is not infected but tests positive for covid
A false negative = someone who is infected but tests negative for covid
A false positive = someone who is not infected but tests positive for covid
A false negative = someone who is infected but tests negative for covid
A false positive is less risky (imo) because many clinics will do a second test to confirm the positive result - before isolating the individual and doing laborious contact tracing to test+isolate everyone else that has been in contact with this person.
A false negative is very risky because many places do not do a second test (a second sampling of the same person) to confirm a negative result.
As a result, this infected person would continue life as normal, possibly infecting dozens of other people.
As a result, this infected person would continue life as normal, possibly infecting dozens of other people.
That is why most diagnostics aim at as low a false negative rate as possible, and a certain level of false positives (estimated <1-4%) is tolerable because you can always do a second test on a SARS2+ person to double check that the first test was accurate.
There's an idea that's been going around a while now that there are too many false positives - remember that most people are getting tested using the highly accurate ~24h PCR diagnostic test (not the rapid antigen test that @elonmusk took 4 times in one day)...
And that these PCR test false positives are somehow massively inflating the reported number of COVID-19 cases in the USA.
I think this is very unlikely because positive cases are usually confirmed again after their first positive test result.
I think this is very unlikely because positive cases are usually confirmed again after their first positive test result.
So, if the PCR tests are so great, why are companies developing and deploying these rapid antigen tests?
What are rapid antigen tests?
These target the protein parts of the virus, and not the RNA. See pic again:
scientificamerican.com/article/a-visu…
What are rapid antigen tests?
These target the protein parts of the virus, and not the RNA. See pic again:
scientificamerican.com/article/a-visu…
Unlike PCR tests, antigen tests do not require expensive infrastructure+personnel and can often produce results in minutes.
However, because these tests are quick and easy, they are not as accurate and suffer from higher false positive AND negatives.
medical.mit.edu/covid-19-updat…
However, because these tests are quick and easy, they are not as accurate and suffer from higher false positive AND negatives.
medical.mit.edu/covid-19-updat…
For people who are familiar with pregnancy tests - this is quite similar. You don't buy 1 pregnancy test stick. Pregnancy test kits are almost always sold as 2 or 3 sticks. You have to double check if your +/- is reproducible.
Faster than testing in clinic, but less accurate.
Faster than testing in clinic, but less accurate.
COVID-19 antigen tests are still in optimization. Just a reminder that companies only started making these tests this year. Several tests are on EUA.
However, if the false positive/negative rate is 50%, that's very troubling, and could suggest that at-home use is not practical.
However, if the false positive/negative rate is 50%, that's very troubling, and could suggest that at-home use is not practical.
Doing these diagnostic tests repeatedly in the same day could also be futile, even if administered by a trained nurse. Imagine swabbing your nose repeatedly, you could have less and less of the virus in the final rounds of swabbing.
The last type of test I'll cover is the antibody test. It doesn't check for the virus RNA or protein.
It checks for the patient immune response (antibodies) against a previous or ongoing SARS-CoV-2 infection.
Antibodies explanation here: livescience.com/antibodies.html
It checks for the patient immune response (antibodies) against a previous or ongoing SARS-CoV-2 infection.
Antibodies explanation here: livescience.com/antibodies.html
Why do these tests target IgA & IgG antibodies?
IgG = the majority of your blood immunoglobulins and are the basis of long-term protection against pathogens.
IgA = in mucus; protects against infection in your respiratory and gastrointestinal tracts.
merckmanuals.com/-/media/Manual…
IgG = the majority of your blood immunoglobulins and are the basis of long-term protection against pathogens.
IgA = in mucus; protects against infection in your respiratory and gastrointestinal tracts.
merckmanuals.com/-/media/Manual…
How accurate are these antibody tests? Short answer: we don't know yet. Again, the covid antibody tests were only just developed this year.
That's why we can't feasibly do antibody passports right now. (Maybe just passports of recovered covid patients.)
medical.mit.edu/faqs/faq-testi…
That's why we can't feasibly do antibody passports right now. (Maybe just passports of recovered covid patients.)
medical.mit.edu/faqs/faq-testi…
Going to circle back to one of the biggest questions about the PCR covid test and why some testing centers look for signal even at high Ct.
First, what is Ct (threshold cycle)?
Neat retro video explaining this here:
thermofisher.com/blog/behindthe…
First, what is Ct (threshold cycle)?
Neat retro video explaining this here:
thermofisher.com/blog/behindthe…
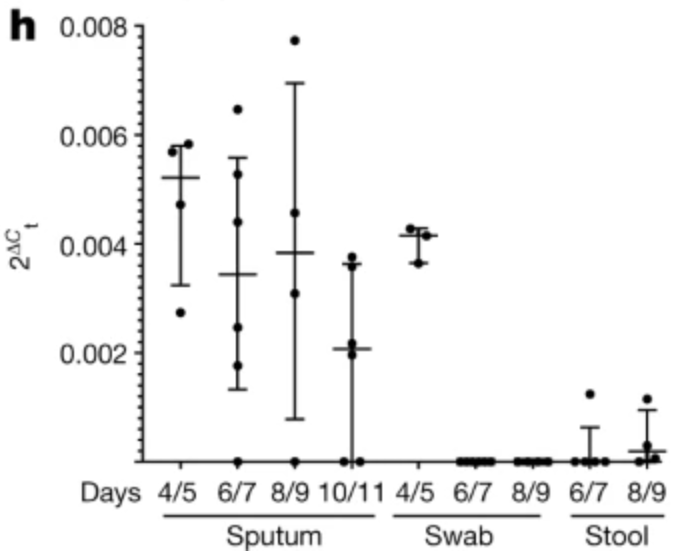
Ct inversely measures the concentration of SARS2 RNA in the patient sample, ie high Ct = low RNA.
The amount of SARS2 RNA in a person depends on a variety of factors: was the test administered properly? (did you get a good sample?) what stage of infection is this person at?
The amount of SARS2 RNA in a person depends on a variety of factors: was the test administered properly? (did you get a good sample?) what stage of infection is this person at?
"patients in the first days of infection have CT values below 30.. indicating a high level of virus; as the body clears the coronavirus, CT values rise.. viral load can profoundly impact a person’s contagiousness and reflect the severity of disease"
sciencemag.org/news/2020/09/o…
sciencemag.org/news/2020/09/o…
I agree with some of the experts interviewed above that Ct values should be added to test results but alongside a major asterisk that the number could be affected by many factors, including errors in the testing protocol and sample processing.
This new study in Rome, Italy found that about 1 in 5 recovered covid patients still had detectable SARS2 RNA, and only 1 out of 32 with detectable RNA tested positive for replicative RNA. jamanetwork.com/journals/jamai… 
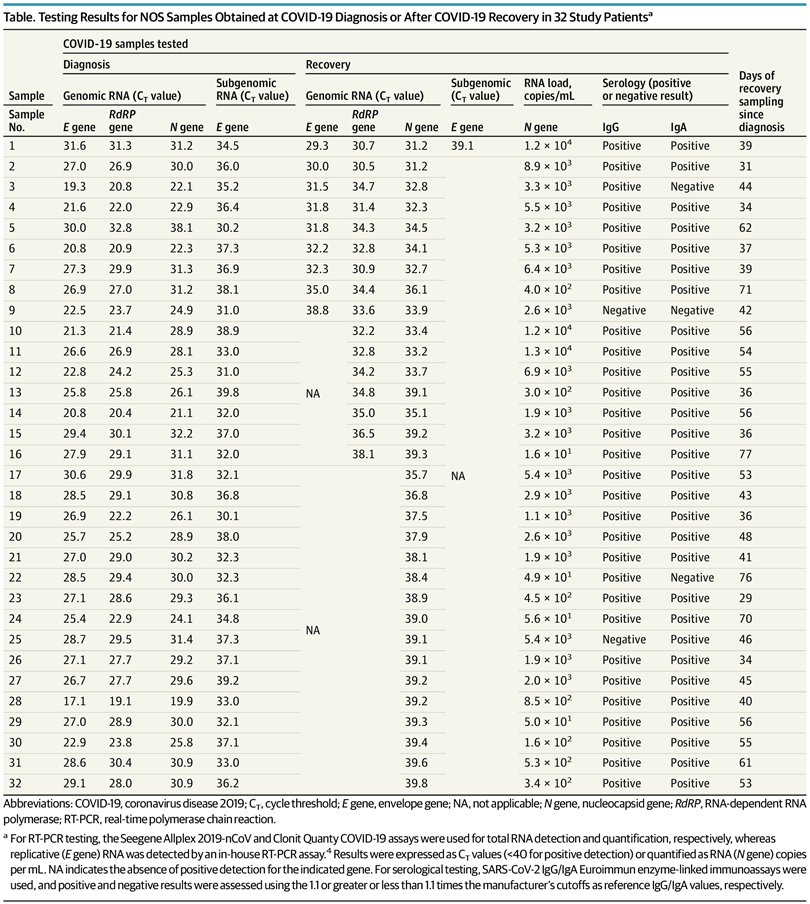
One question: why aren't we just PCR testing for replicative (subgenomic) virus RNA instead?
The answer is that these replicative RNA are at very low quantities, difficult to detect compared to straight up virus genomic RNA.
nature.com/articles/s4158…
The answer is that these replicative RNA are at very low quantities, difficult to detect compared to straight up virus genomic RNA.
nature.com/articles/s4158…
Ultimately, does the detection of SARS2 RNA in recovered cases change the number of recorded covid cases and the need to contact trace? No.
But does it affect test+isolate policy? Yes.
What can we do about this? How cautious should the test+isolate policy be?
But does it affect test+isolate policy? Yes.
What can we do about this? How cautious should the test+isolate policy be?
It's really up to each policymaker and their priorities. Balancing between totally sealing off chains of covid transmission vs having as many people in the workforce/social scene as possible.
I think remote work+social dist+outdoor dining are very important as solutions...
I think remote work+social dist+outdoor dining are very important as solutions...
Even though some infectious individuals are in your community, if they're not hopping from family, to coffee shop, to public commute, to office, to lunch place, to office, to restaurant/bar (to nightclub), back to family on repeat - you're buffered against superspreading events.
Parallel thread by @pbleic to help understand what to do if you took a covid test to decide whether to see your family & friends for Thanksgiving. The false positive rate depends on the test sensitivity and how bad the outbreak is in your area.
https://twitter.com/pbleic/status/1327640113736798209
For example @pbleic calculates that if you're asymptomatic and you get a positive covid test result, your chances of really having covid is only ~66% in Massachusetts but ~92% in Florida - due to the different prevalence of covid in each state.
https://twitter.com/pbleic/status/1327645899720429569
• • •
Missing some Tweet in this thread? You can try to
force a refresh



