1/ #IDTwitter and #IDFellows, here is another #IDboardreview question: 20F p/w pharyngitis w/fever. There is no cough. Exam: Cervical adenopathy; tonsillar exudate. Rapid Strep antigen test pos. You start to prescribe her Amoxicillin but there is an allergy alert.
2/ She reports an allergic reaction to penicillin around age 8 or 9. She had a rash but no other symptoms. It resolved following discontinuation of med. She did not receive any treatment. Which of the following would you do next?
4/ Penicillin is the most commonly reported drug allergy (followed by sulfonamides) documented in patient charts. However, most of these are documented based on patient account and not observed reactions. PMID: 26970431
5/ PCN allergy is assc w/worse outcomes. The avoidance of beta-lactams when they are the reatment of choice, has been associated with incr. risk of drug resistant infections, C difficile colitis and increased hospital LOS.
PMID: 29950489; 24188976; 27402820
PMID: 29950489; 24188976; 27402820
6/ How does penicillin cause allergy? This great review from @NEJM (PMID: 31826341) explains. The beta-lactam ring has the ability to bind lysine residues in the plasma and can form penicilloyl polylysine, which stimulates antibody production. 

7/ Following sensitization, rechallenge of penicillin can lead to IgE mediated antibody response, which leads to mast cell degranulation and the classic presentation of anaphylaxis. Source: NEJM 

8/ Penicillin, and beta-lactams in general, are also associated with other types of allergic reactions, including T Cell-mediated (Type IV), IgG-mediated (Type II), and immune complex-mediated (Type III) reactions. However, anaphylaxis is the most feared adverse effect.
9/ Penicillin allergy can be deadly, but a significant proportion of people do not have real allergy when tested or re-challenged. This equates to worsened patient outcomes for no reason. PMID: 30644987
Image (skin testing) from JAMA - PMID: 30644984
Image (skin testing) from JAMA - PMID: 30644984
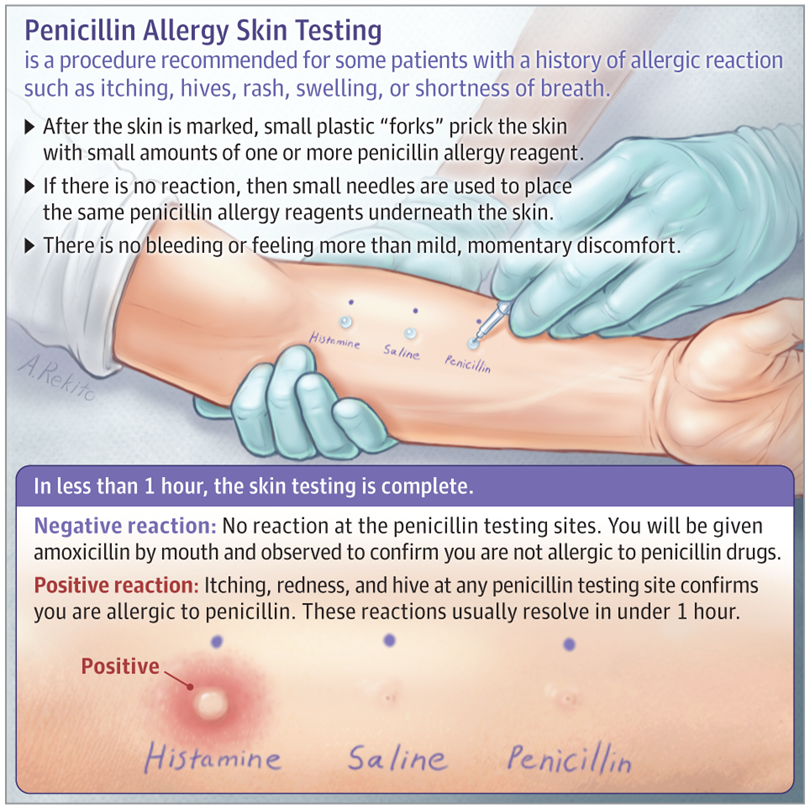
10/ How can you take PCN allergy off of pts’s charts? One way is to perform skin testing, which has been shown to be safe and effective (PMID: 24565482). Alternatively, a recently developed decision support tool called PEN-FAST can help to delabel patients (PMID: 32176248). 

11/ PEN-FAST was derived from data on > 600 pts and was validated in > 900 pts. A score < 3 equates to a NPV of 96.3% and is suggested a cutoff for possible oral challenge w/skin testing. In this scenario our patient had a score of 0, w/NPV of 99.4%. qxmd.com/calculate/calc…
12/ In our patient, the chance of any hypersensitivity response would have been approx 0.6%.
Ok #IDTwitter and #IDFellows, after this tweetorial do you feel more confident in using penicillin in low-risk patients based on the PEN-FAST score?
Ok #IDTwitter and #IDFellows, after this tweetorial do you feel more confident in using penicillin in low-risk patients based on the PEN-FAST score?
@wuIDq @BIDMC_IDFellows @Tufs_ID @IUIDfellowship @UAB_ID @yaleIDfellows @ID_musc @templeID1 @VUMC_IC @MayoclinicINFD @MGH_ID @UCLA_ID @MontefioreID @UNMC_ID @UVA_ID @OhioState_ID @UTSWinfDis @BrownIDprogram @RushCCH_ID @OHSU_ID
• • •
Missing some Tweet in this thread? You can try to
force a refresh