
For the first question: No trials showing higher pCR w/ higher dose. Trials are actually remarkably consistent (no difference):
INTERACT pubmed.ncbi.nlm.nih.gov/31005204/
RECTAL-BOOST pubmed.ncbi.nlm.nih.gov/32565319/
Dose-Effect pubmed.ncbi.nlm.nih.gov/22592048/
#jc questions #radonc
INTERACT pubmed.ncbi.nlm.nih.gov/31005204/
RECTAL-BOOST pubmed.ncbi.nlm.nih.gov/32565319/
Dose-Effect pubmed.ncbi.nlm.nih.gov/22592048/
#jc questions #radonc
https://twitter.com/CarmeloT2681/status/1330177386592301057
❗️*However* ❗️
pCR doesn't matter to the patient! Only OS or QoL does! And pCR / tumour regression is not a surrogate for radiotherapy effects on OS, so why should we care about it? #radonc #jc
pubmed.ncbi.nlm.nih.gov/25611452/
pubmed.ncbi.nlm.nih.gov/26723110/
pCR doesn't matter to the patient! Only OS or QoL does! And pCR / tumour regression is not a surrogate for radiotherapy effects on OS, so why should we care about it? #radonc #jc
pubmed.ncbi.nlm.nih.gov/25611452/
pubmed.ncbi.nlm.nih.gov/26723110/
If you think about it, we are actually unlikely to see a dose-response relationship for rectal cancer in the (neo-)adjuvant setting: Even if there exists a dose-response relationship, it must be very shallow
https://twitter.com/cancerphysicist/status/1268839637889490945?s=20
(Side note: pCR / tumour regression / neoadjuvant rectal score *might* be a surrogate for chemotherapy effects on OS or PFS, but not validated on trial level:
pubmed.ncbi.nlm.nih.gov/29206996/
pubmed.ncbi.nlm.nih.gov/29718095/
And data are inconsistent
pubmed.ncbi.nlm.nih.gov/19759186/
#radonc #jc)
pubmed.ncbi.nlm.nih.gov/29206996/
pubmed.ncbi.nlm.nih.gov/29718095/
And data are inconsistent
pubmed.ncbi.nlm.nih.gov/19759186/
#radonc #jc)
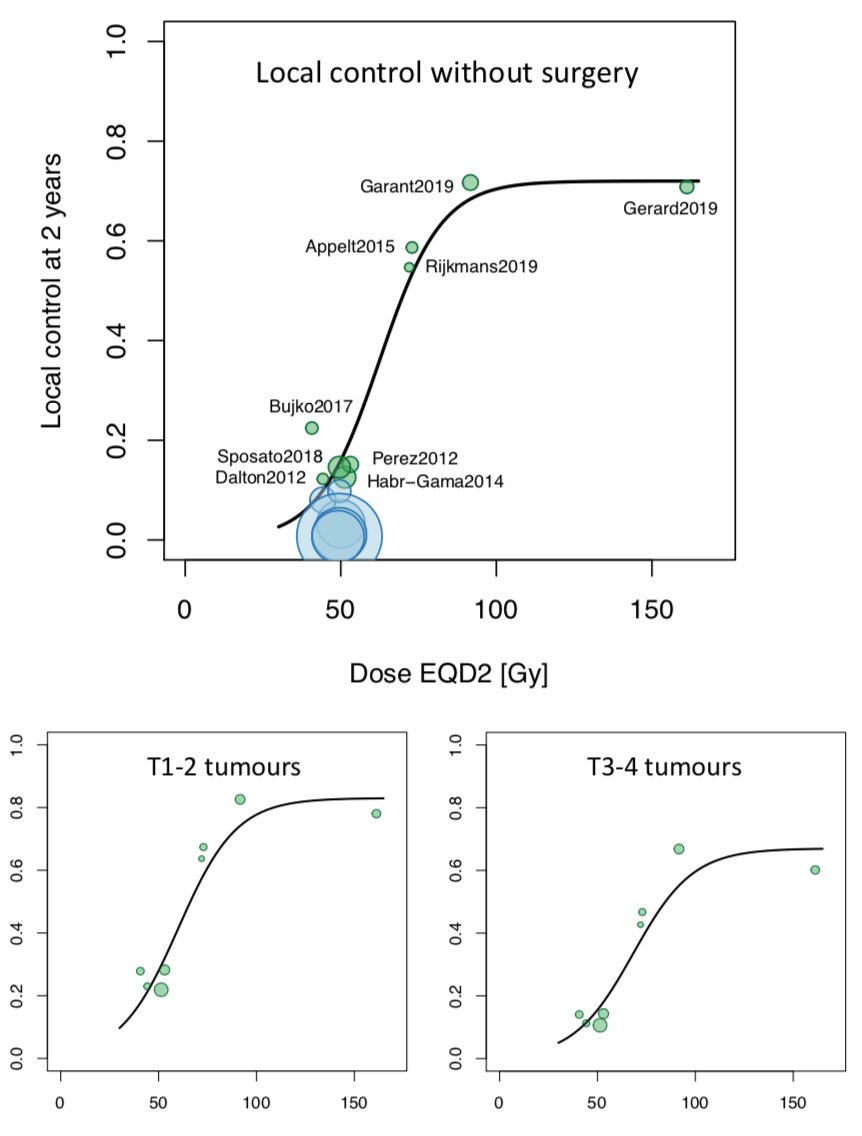
So what matters to patients? Organ preservation (NOM) would - but that depends on
1) clinical complete response (cCR), and
2) long term local control without surgery
#radonc #jc
1) clinical complete response (cCR), and
2) long term local control without surgery
#radonc #jc
Can we get more cCR with higher RT dose? pCR is different from cCR, so we can't rely just on the trials examining pCR. We only have the (old) data from Lyon R 96-02:
pubmed.ncbi.nlm.nih.gov/22579379/ #radonc #jc
pubmed.ncbi.nlm.nih.gov/22579379/ #radonc #jc
On the other hand, the trials quoted above (INTERACT, RECTAL-BOOST, Dose-Effect) are consistent in showing an effect of dose escalation on tumour regression (TRG1-2). OR=1.6, OR=2.7, OR=1.9. This is still path endpoint, though, so still doesn't matter to patients #radonc #jc
There are ongoing trials testing radiation dose escalation for organ preservation / NOM:
APHRODITE ctru.leeds.ac.uk/aphrodite/
WW3 clinicaltrials.gov/ct2/show/NCT04…
So we have to wait for the outcome of these 😊
#radonc #jc
APHRODITE ctru.leeds.ac.uk/aphrodite/
WW3 clinicaltrials.gov/ct2/show/NCT04…
So we have to wait for the outcome of these 😊
#radonc #jc
In the meantime, here are some data based on a literature-based meta-analyses #radonc #jc
estro.org/Congresses/EST…
estro.org/Congresses/EST…
This doesn't address the question of dose escalation for patients w/ risk of incomplete surgical resection: T4 tumours, pelvic side wall nodes, etc. To the best of my knowledge, we don't have firm evidence in this setting either - and I'm unsure if any ongoing trials? #radonc #jc
And here ends my tweetorial on rectal cancer dose escalation. That was probably far more than you wanted to know 😉 #radonc #jc
• • •
Missing some Tweet in this thread? You can try to
force a refresh



