Preprint: COVID-19 screening and surveillance are critical, but molecular tests haven't come close to meeting needs, and temperature checks fail. We modeled the epidemiological impacts of using loss of smell as a screening symptom. Here's what we found. 1/ medrxiv.org/content/10.110…
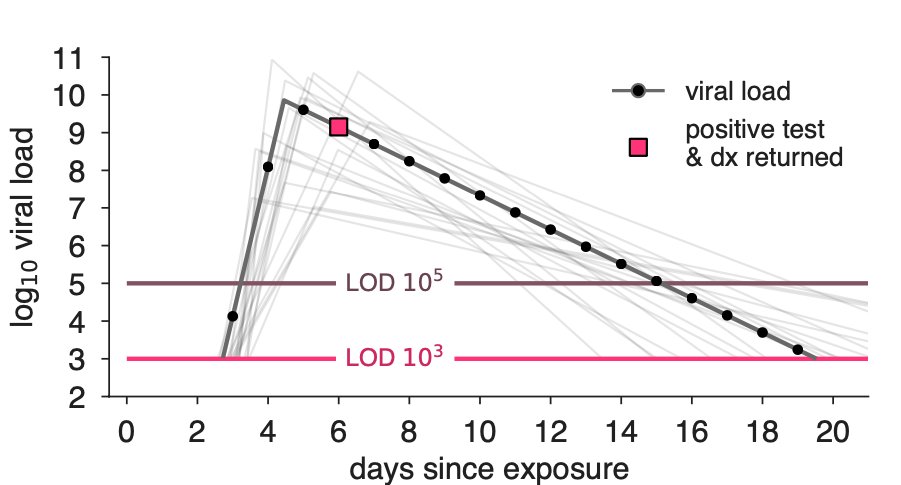
Loss of smell is an interesting screening symptom because it's highly specific to COVID, precedes most other overt symptoms, and typically lasts ~1 week. Critically, its prevalence goes from ~45% when self-reported up to ~80% when a test is used. 2/
Contrast this with fever: ~20% prevalence, not specific to COVID, and lasts 1.5 days on average. So why do we still screen for fever? You can look for it in seconds with a contactless thermometer.
Could rapid, contactless, cheap tests for anosmia, impact transmission? 3/
Could rapid, contactless, cheap tests for anosmia, impact transmission? 3/
Our main finding is that screening for olfactory dysfunction could break enough transmission chains to decrease R and mitigate outbreaks. (Fig R0=1.6)
Just like our work on PCR/antigen screening, impact increases with test frequency (see thread).

Just like our work on PCR/antigen screening, impact increases with test frequency (see thread).
https://twitter.com/DanLarremore/status/1329867941479809024?s=20

In the paper, we examine whether our results hold for different assumptions about (1) the timing of olfactory dysfunction's onset, (2) its duration, and (3) its prevalence. We find that biweekly OD screening is similar or superior to weekly PCR, unless OD onset time is late. 5/ 

Just as @StephenKissler et al did for the early stages of viral load trajectories in the @NBA study, prospective longitudinal screening for anosmia would be of GREAT benefit to tighten up estimates of the critical parameter of anosmia's typical onset time.
https://twitter.com/yhgrad/status/1319733829205217282
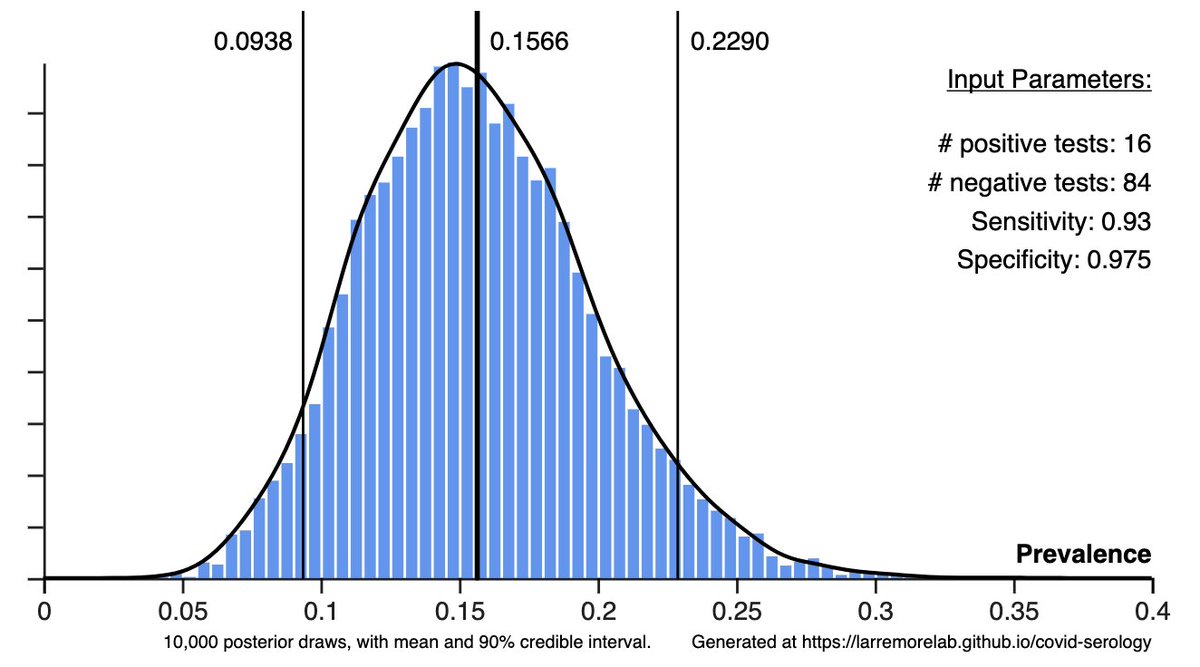
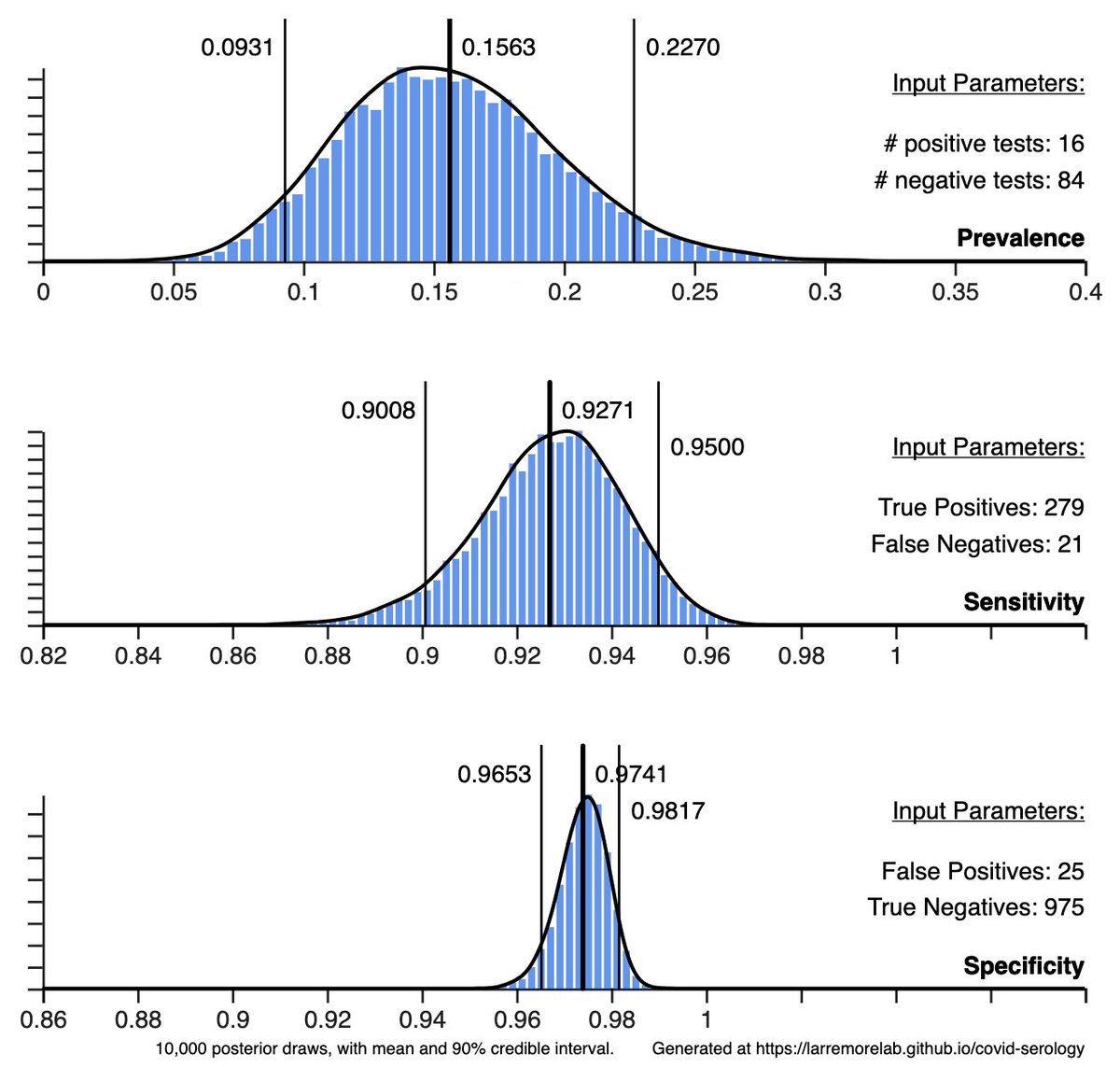
We also considered whether olfaction tests could be used at point-of-entry (e.g. airport, restaurant). 3-5% of people have non-COVID anosmia, so we modeled a rapid antigen test to avoid turning away false positives. This 2-shot screening cost ~$1/person and was >70% effective. 7/
The tech that could realize our modeling looks like an index card with 5 scratch/sniff panels on it. A QR code opens a multiple choice quiz on your phone, which tests your ability to discern the smells.
It takes 60 seconds, costs $0.50, and these are easy to print at scale. 7/
It takes 60 seconds, costs $0.50, and these are easy to print at scale. 7/
Low costs mean that repeated olfactory screening could be highly cost effective, even w/ followup PCR. This plot shows epidemic mitigation simulations & estimated costs.
Even if PCR costs only $20/test, we estimate OD screening would work better & be an order of mag cheaper. 8/
Even if PCR costs only $20/test, we estimate OD screening would work better & be an order of mag cheaper. 8/

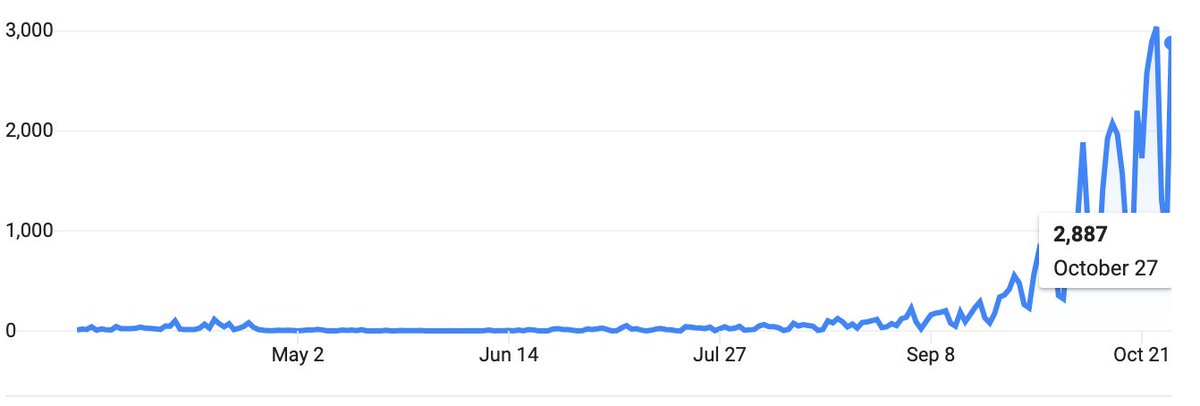
Importantly, OD testing is scalable. People can self-test, there is no need for a central laboratory, and a single commercial printing facility could produce tens of millions of OD tests daily—staggering outputs when total U.S. testing is ~2 million/day, per @COVID19Tracking 9/
Still, modeling studies have limitations. Our model assumes that tests would remain sensitive over regular use—that people wouldn't adapt or memorize patterns. We also assumed no one would intentionally fail a test. Humans are complicated, and these are strong assumptions. 10/
We also assumed that a positive test would lead to isolation, but this is unlikely to be valid for essential workers, those who cannot afford to isolate, or those who just refuse.
A comprehensive testing plan means making sure anyone who wants to isolate can do so safely! 11/
A comprehensive testing plan means making sure anyone who wants to isolate can do so safely! 11/
Finally, let me disclose a COI here because open science is important. Toomre (2nd author), is the founder of an olfactory test company, and has filed an EUA for applications to COVID-19. Still, all of our modeling assumptions rest firmly in the established literature. 12/
With coauthors Roy Parker & Derek Toomre, we hope that olfactory dysfunction testing may be more broadly considered for COVID-19 screening & mitigation.
Our modeling strongly suggests that we should not continue to ignore this symptom of COVID-19.
medrxiv.org/content/10.110…
Our modeling strongly suggests that we should not continue to ignore this symptom of COVID-19.
medrxiv.org/content/10.110…
Finally, this is a preprint, and feedback on the paper would be valuable. There's no point in this work if it's not useful. Our email addresses are on the front page of the paper.
• • •
Missing some Tweet in this thread? You can try to
force a refresh