Images of Infectious Diseases
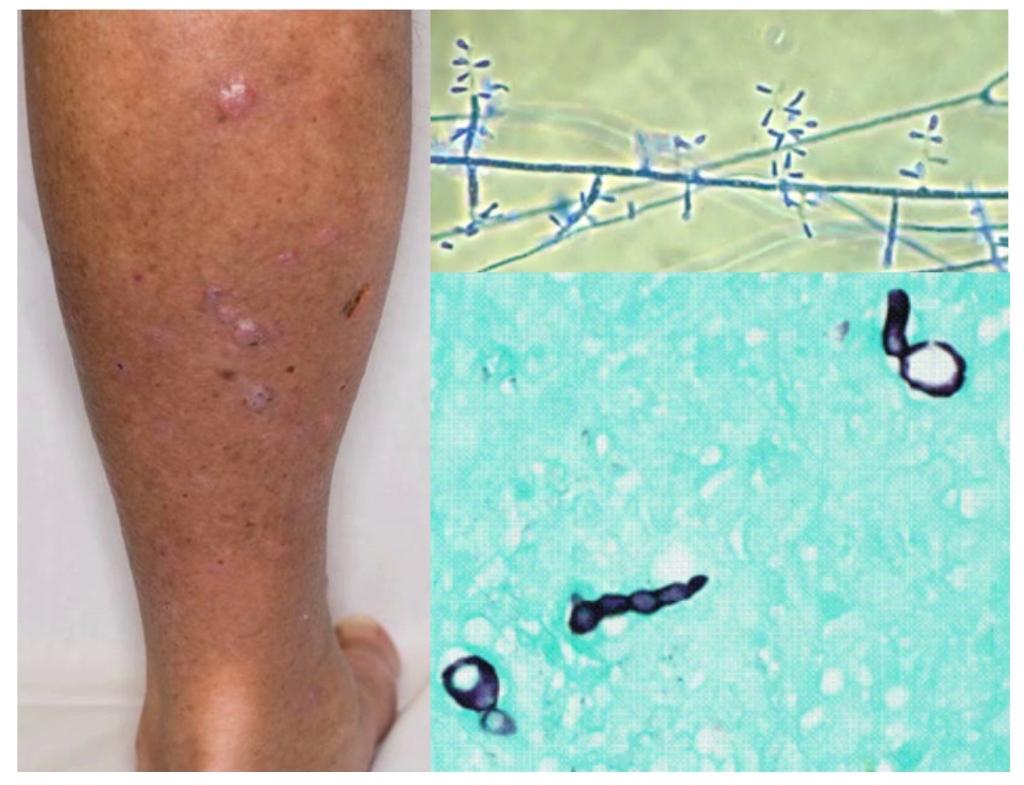
GMS of sinus tissue of 20F with no PMH. She presented with fever and sinus pain. CT pansinusitis. Labs: WBC 1.7 ANC 0. Serum BDG and GM negative.
What is your differential diagnosis and empiric therapy? #MayoIDQ to follow...
GMS of sinus tissue of 20F with no PMH. She presented with fever and sinus pain. CT pansinusitis. Labs: WBC 1.7 ANC 0. Serum BDG and GM negative.
What is your differential diagnosis and empiric therapy? #MayoIDQ to follow...

2/
Histopath of surgically resected tissue shows fungal elements. You suggested Mucor/Rhizopus, Fusarium, Trichosporon.
Lack of serum BDG suggests Mucor/Rhizopus
The patient was started on AmBisome.
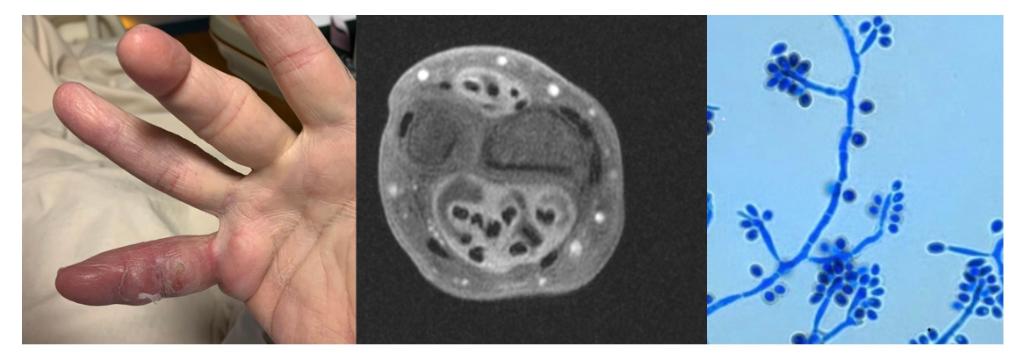
Few days later, the fungal culture of the same sinus sample shows (photo)
Histopath of surgically resected tissue shows fungal elements. You suggested Mucor/Rhizopus, Fusarium, Trichosporon.
Lack of serum BDG suggests Mucor/Rhizopus
The patient was started on AmBisome.
Few days later, the fungal culture of the same sinus sample shows (photo)

3/
#MayoIDQ Surgical debridement of the sinuses was performed plus liposomal Amphotericin B was initiated. Patient lives in rural MN and asks you if an oral option is available as step down Rx.
#MayoIDQ Surgical debridement of the sinuses was performed plus liposomal Amphotericin B was initiated. Patient lives in rural MN and asks you if an oral option is available as step down Rx.
4/
Case diagnosis: #Fusarium invasive sinusitis in a neutropenic host
Treatment:
Surgical debridement plus
Liposomal Amphotericin B + voriconazole initially then voriconazole monotherapy upon clinical improvement
Case presented by ID fellow @ZYetmar
Case diagnosis: #Fusarium invasive sinusitis in a neutropenic host
Treatment:
Surgical debridement plus
Liposomal Amphotericin B + voriconazole initially then voriconazole monotherapy upon clinical improvement
Case presented by ID fellow @ZYetmar
5/
#Fusarium #Pearls
1. Widely distributed in nature
2. Risks (photo)
3. Keratitis. Onychomycosis. Cutaneous. Allergic sinusitis. Invasive and disseminated disease.
4. Dx: culture (including blood). BDG often + in invasive/disseminated disease
5. Rx: LAmB, voriconazole
#Fusarium #Pearls
1. Widely distributed in nature
2. Risks (photo)
3. Keratitis. Onychomycosis. Cutaneous. Allergic sinusitis. Invasive and disseminated disease.
4. Dx: culture (including blood). BDG often + in invasive/disseminated disease
5. Rx: LAmB, voriconazole

6/
#Fusariosis in ICH
1. Fever not responsive to antibiotic
2. Prolonged/profound neutropenia
3. Cutaneous, sinusitis, pneumonia, fungemia, disseminated
4. Sporulates in vivo - blood cx often + if invasive; BDG+ in many; GM cross react in some
5. Rx: LAmB, azoles (V, P, Isa)
#Fusariosis in ICH
1. Fever not responsive to antibiotic
2. Prolonged/profound neutropenia
3. Cutaneous, sinusitis, pneumonia, fungemia, disseminated
4. Sporulates in vivo - blood cx often + if invasive; BDG+ in many; GM cross react in some
5. Rx: LAmB, azoles (V, P, Isa)
7/
#Fusarium treatment
Reduce risk (correct neutropenia; reduce IS)
Antifungal Rx
1. LAmB - first line Rx
2. Vori - alternative / stepdown once improvement
3. Combo LAmB + vori (empiric prior to susceptibility)
Check for susceptibility
Posaconazole, Isavuconazole: alternatives
#Fusarium treatment
Reduce risk (correct neutropenia; reduce IS)
Antifungal Rx
1. LAmB - first line Rx
2. Vori - alternative / stepdown once improvement
3. Combo LAmB + vori (empiric prior to susceptibility)
Check for susceptibility
Posaconazole, Isavuconazole: alternatives
8/
What predisposed to #fusariosis?
Neutropenia (ANC 0)
#Autoimmune #Neutropenia
Granulocyte-specific antibodies
Often an incidental finding
Infection correlates with ANC severity
Infections: URI, sinusitis, otitis media
Rx: GCSF, IVIG, prednisone, rituximab —> splenectomy
What predisposed to #fusariosis?
Neutropenia (ANC 0)
#Autoimmune #Neutropenia
Granulocyte-specific antibodies
Often an incidental finding
Infection correlates with ANC severity
Infections: URI, sinusitis, otitis media
Rx: GCSF, IVIG, prednisone, rituximab —> splenectomy
/9
Case resolution:
#Invasive #fusariosis in patient with autoimmune neutropenia
Rx: LAmB + voriconazole —> voriconazole monotherapy
GCSF, neutrophil transfusion, IVIG, prednisone.... eventually splenectomy
Thanks for participating!
Case resolution:
#Invasive #fusariosis in patient with autoimmune neutropenia
Rx: LAmB + voriconazole —> voriconazole monotherapy
GCSF, neutrophil transfusion, IVIG, prednisone.... eventually splenectomy
Thanks for participating!
• • •
Missing some Tweet in this thread? You can try to
force a refresh