1/ "Don't forget to correct that phosphate so that the it can help the patient recover from acute respiratory failure !" This concept triggered a lot of questions on rounds.
It's worth taking a quick look at this association !
#medtwitter #MedStudentTwitter #FOAMed #phosphate
It's worth taking a quick look at this association !
#medtwitter #MedStudentTwitter #FOAMed #phosphate

2/⬇️Phosphate leads to ⬇️red cell 2,3-DPG and a reduction in ATP.
⬇️Phosphate diverts glucose -> 1,3-DPG into the Rapoport-Leubering pathway away from ATP generation towards producing 2,3-DPG so that the oxygen affinity of RBC's does not increase and the tissues receive O2.
⬇️Phosphate diverts glucose -> 1,3-DPG into the Rapoport-Leubering pathway away from ATP generation towards producing 2,3-DPG so that the oxygen affinity of RBC's does not increase and the tissues receive O2.
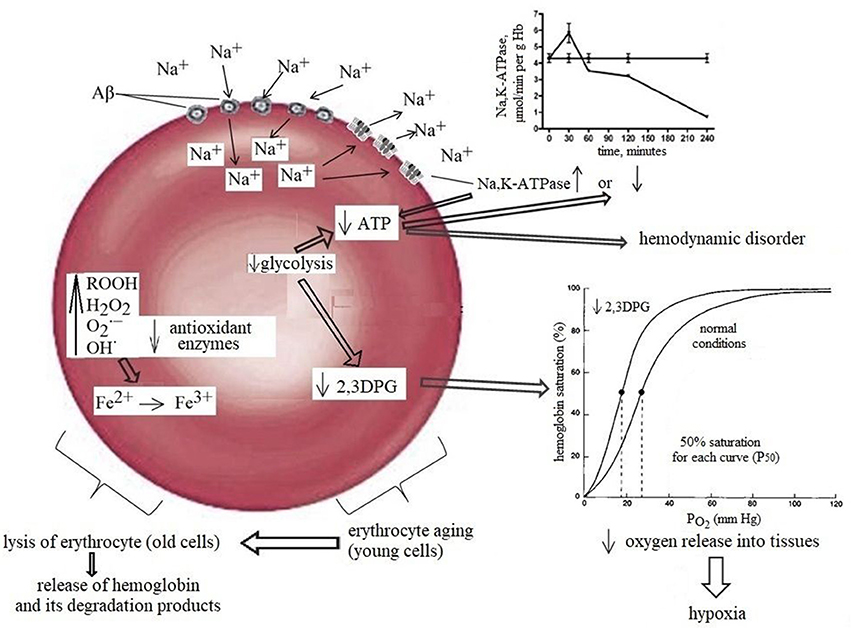
3/⬇️Phosphate does also impact RBC survivability with a
⬆️hemolysis, ⬇️in RBC deformability, ⬇️ capillary transit and ⬇️GSH.
⬆️hemolysis, ⬇️in RBC deformability, ⬇️ capillary transit and ⬇️GSH.

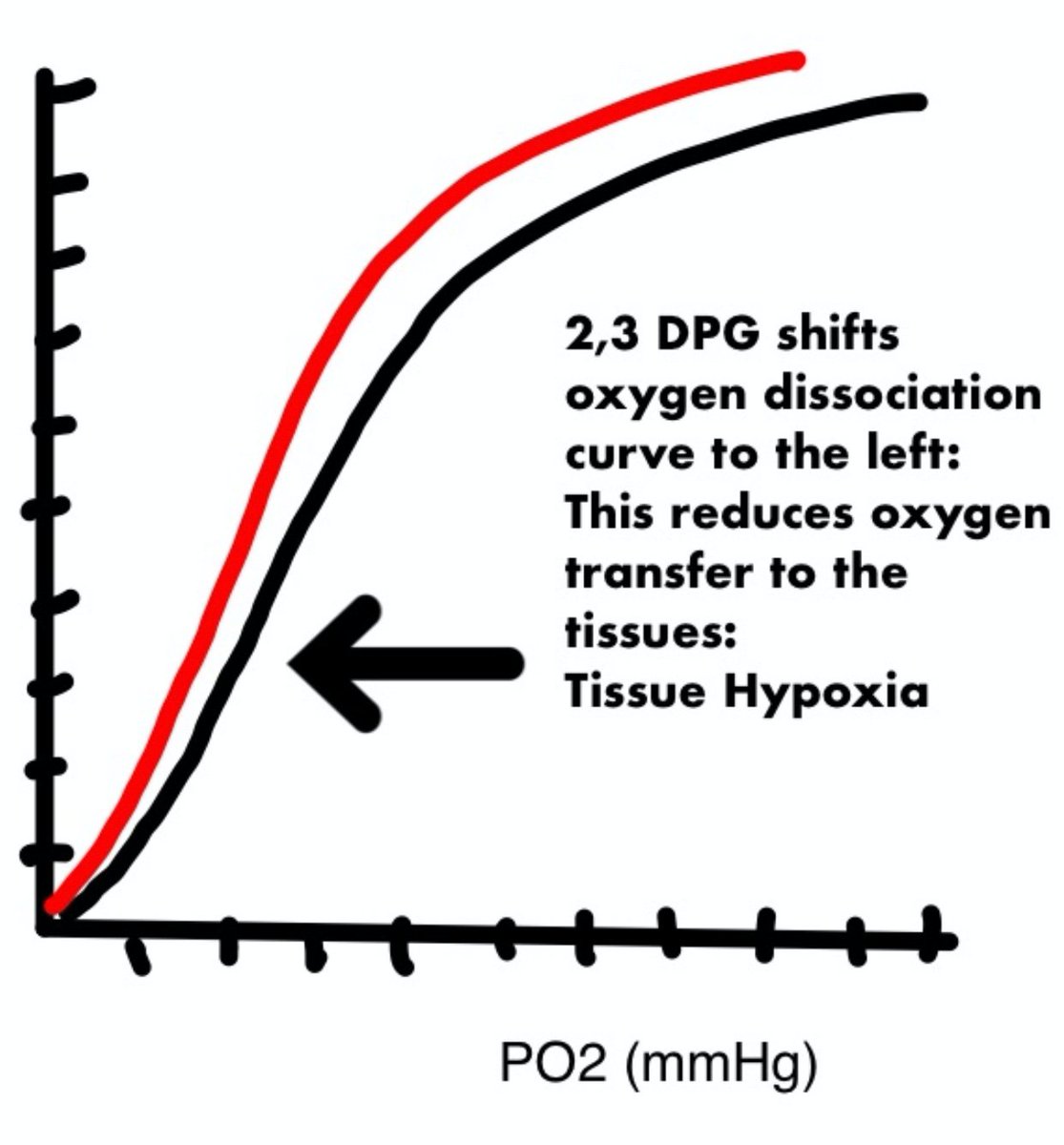
4/⬇️Phosphate leads to a ⬇️red cell 2,3-DPG which shifts the oxygen dissociation curve to the left and makes oxygen less available to the tissues--> Tissue hypoxia. 
5/Another mechanism where⬇️Phosphate impacts respiratory function is respiratory muscle weakness and can contribute to respiratory acidosis.
nejm.org/doi/full/10.10…
pubmed.ncbi.nlm.nih.gov/3364446/
nejm.org/doi/full/10.10…
pubmed.ncbi.nlm.nih.gov/3364446/

6/ Maximal inspiratory & expiratory pressures in pts with⬇️Phosphate was studied and correlated with respiratory muscle weakness (defined as low maximal inspiratory pressure or low maximal expiratory pressure). Respiratory muscle strength improved after phosphate repletion. 

7/Hypophosphatemia also impairs the contractile properties of the diaphragm during acute respiratory failure. In this study, transdiaphragmatic pressure increased in all eight patients and the increase correlated with the change in serum phosphorus concentration 

8/Also⬇️Phosphate is a cause of refractory weaning from the ventilator. In one study, most patients had severe hypophosphatemia (≤1.0 mg/dl [0.3 mmol/l]). Weaning from the ventilator was achieved following correction of hypophosphatemia.
annclinlabsci.org/content/40/2/1…
annclinlabsci.org/content/40/2/1…
9/⬇️ phosphorus is seen in COPD.
It is severe in respiratory and peripheral muscles and maybe due to
-malnutrition
-condition of renal phosphorus wasting possibly linked to some drugs commonly used in patients with COPD (xanthine derivatives etc)
pubmed.ncbi.nlm.nih.gov/8181325/
It is severe in respiratory and peripheral muscles and maybe due to
-malnutrition
-condition of renal phosphorus wasting possibly linked to some drugs commonly used in patients with COPD (xanthine derivatives etc)
pubmed.ncbi.nlm.nih.gov/8181325/
10/In summary
Respiratory insufficiency and failure-to-wean may well be due to ⬇️ 2,3-DPG causing a shift in the hemoglobin dissociation curve to the left.
Respiratory muscles may be weakened by ⬇️production of ATP or creatine phosphate and this⬇️diaphragmatic contractility
Respiratory insufficiency and failure-to-wean may well be due to ⬇️ 2,3-DPG causing a shift in the hemoglobin dissociation curve to the left.
Respiratory muscles may be weakened by ⬇️production of ATP or creatine phosphate and this⬇️diaphragmatic contractility
11/Respiratory muscle weakness is common amongst hypophosphatemic patients especially in hospitalized patients and improves with phosphate repletion.
amjmed.com/article/0002-9…
amjmed.com/article/0002-9…
• • •
Missing some Tweet in this thread? You can try to
force a refresh