
@LiangGQu, Vaisnavi Thirugnanasundralingam, @damien_bolton, @UroOncMD & @lawrentschuk reviewed the role of tissue-based immunohistochemical markers for diagnosis and classification of #RCC in this 1st edition of #SIUJ!
#OpenAccess #UroSoMe
siuj.org/index.php/siuj…
1/n
#OpenAccess #UroSoMe
siuj.org/index.php/siuj…
1/n

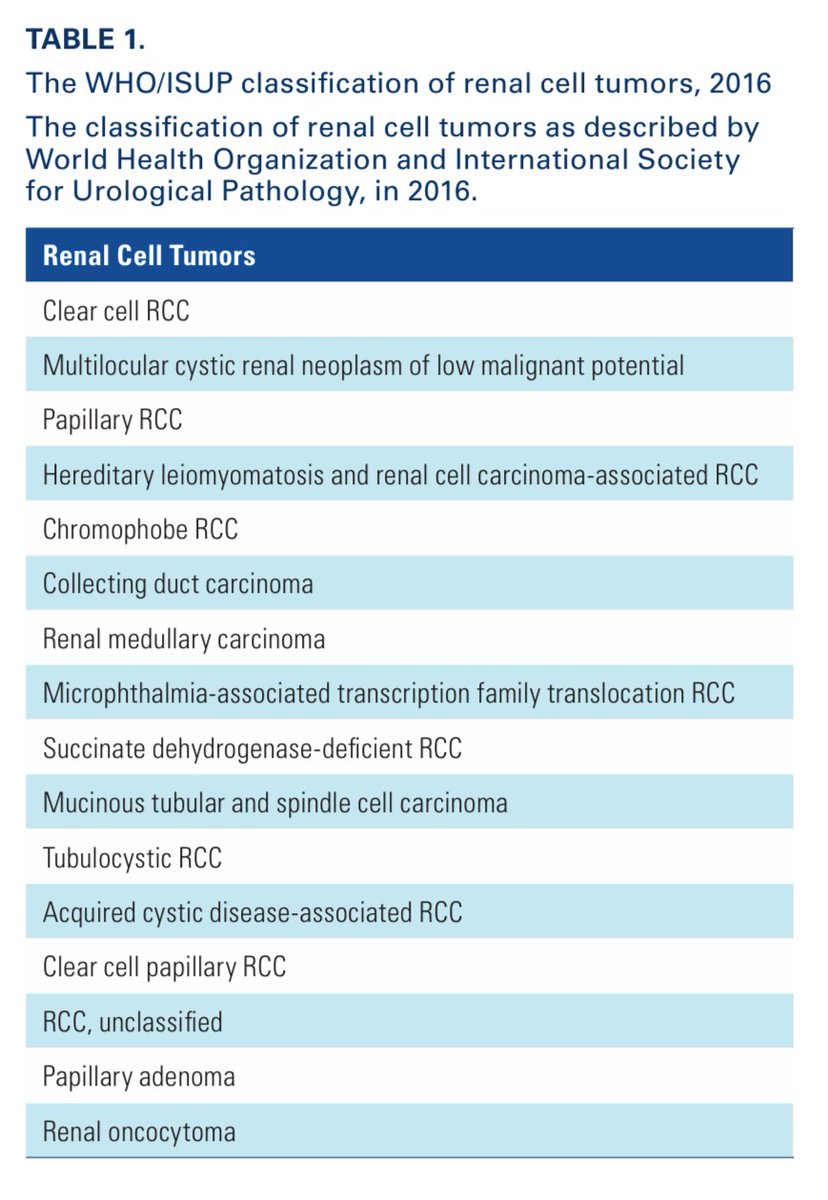
#RCC presents various subtypes, classified according to anatomical, morphological, immunohistochemical (#IHC) & molecular features. Even after '16 reclassification, tissue biomarkers differentiate RCC subtypes & distinguish them from non-renal neoplasms or metastatic disease
2/n
2/n
Despite advances in #IHC staining, challenges are:
- Staining heterogeneity across and within tumors
- Variations in processing may = inconsistencies
- Revisions by @WHO & @ISUPorg = misinterpretation of older literature
- Smaller samples (biopsies) needing to be analyzed
3/n
- Staining heterogeneity across and within tumors
- Variations in processing may = inconsistencies
- Revisions by @WHO & @ISUPorg = misinterpretation of older literature
- Smaller samples (biopsies) needing to be analyzed
3/n
Clear cell #RCC (#ccRCC) is responsible for 75% of RCCs. Its staining profile has been widely characterized, but marker that may aid differentiation are still being described. A suggested panel of #IHC markers includes vimentin, RCCM, CAIX, Ksp-cadherin, CD117 & parvalbumin. 4/n 

Papillary RCC (#pRCC) is the second most common #RCC subtype, representing 15% of diagnosed #RCCs. To assist with classifying a RCC with papillary features, a #IHC marker panel should consist of CK7, AMACR, CD10, RCCM, TFE3, and CD57.
5/n
5/n
Chromophobe RCC (#chRCC) represents up to 11% of diagnosed RCCs and it remains challenging to diagnose because they share morphological and #IHC features with renal oncocytomas (#ROs). Several markers to distinguish between ROs and chRCCs have been investigated.
6/n
6/n

Also, other #IHC markers useful in work-up for ruling out non-renal neoplasms include PAX2, PAX8, RCCM, CD10, vimentin and CKs. And GATA3, CA-125 and CK20 consistently stain negative in RCC specimens.
7/7
7/7
• • •
Missing some Tweet in this thread? You can try to
force a refresh



