
Optimistic news: National data on new coronavirus infections data do now show we have passed the peak. Good news but really this is just the end of the beginning for the NHS response. 1/7 
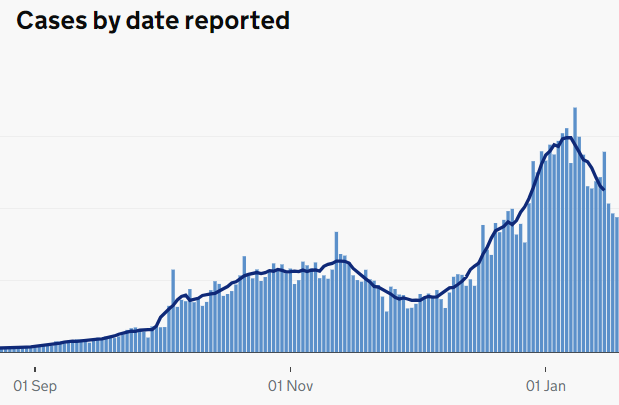
Firstly, the national data hide regional differences. New infections are still increasing in many parts of the UK. NHS hospitals in different areas will need to support each other for some time to come. 2/7 
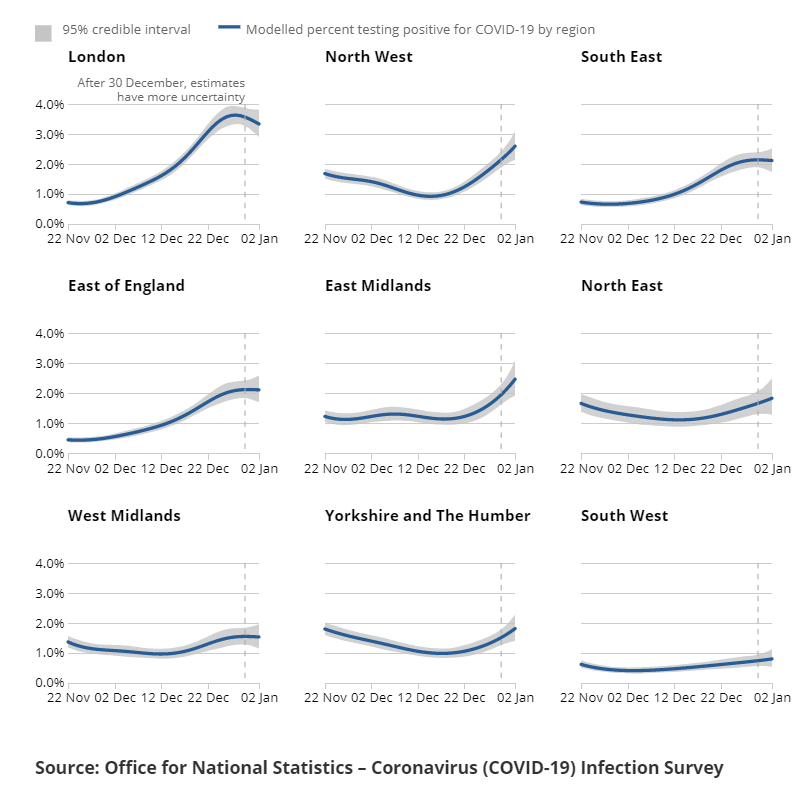
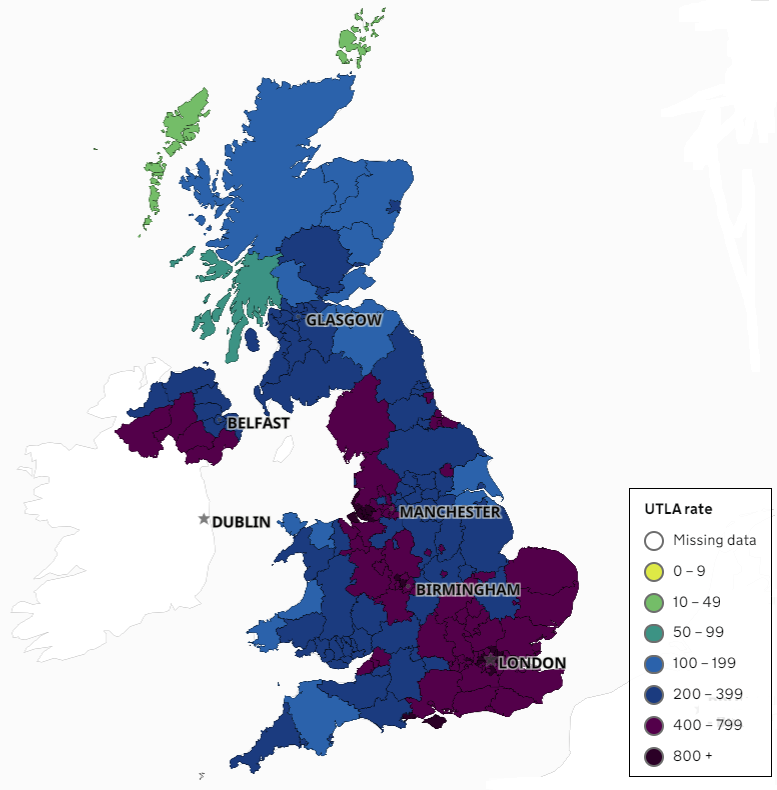
This map illustrates this much more clearly. Many areas of the country still very badly affected by new infections. This affects NHS healthcare in pretty much every part of the UK. 3/7 
Hospital admissions are still rising although we hope they will peak within 7 days. BUT the second wave has already lasted much longer than the first, with far more hospital admissions. These patients will take a long time to recover and go home. We have a long way to go. 4/7 
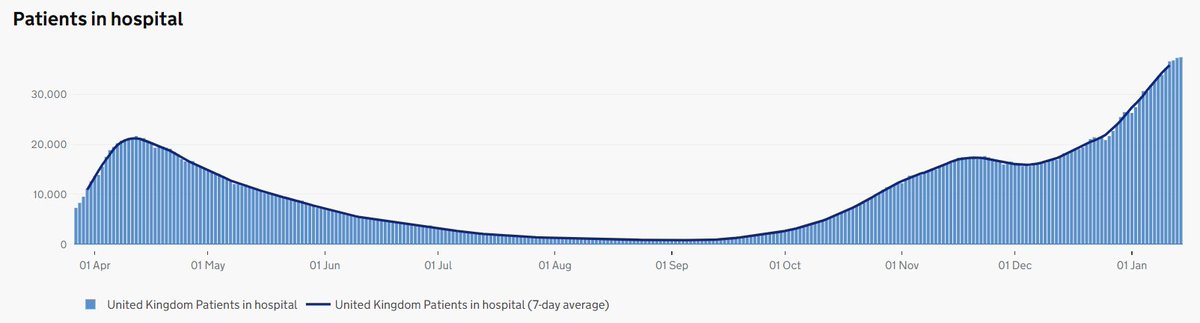
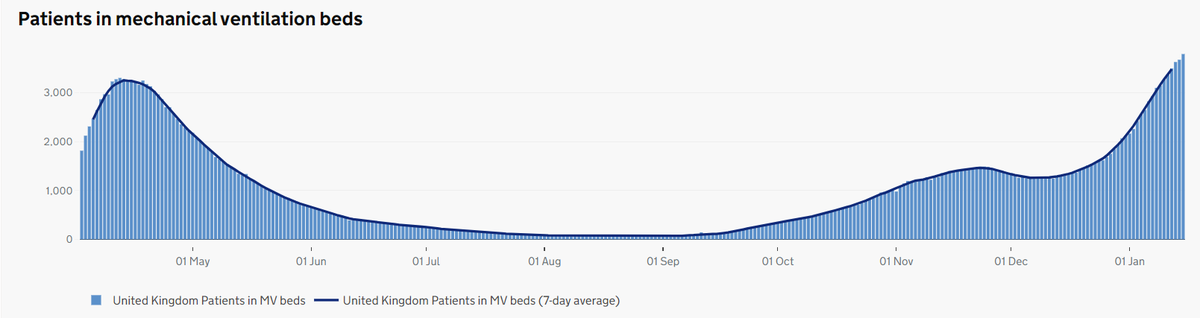
A similar pattern in intensive care. The demand for ICU beds is far greater than the first wave - something which was hard to imagine until a few weeks ago. It now seems inevitable that hospitals will still have a large COVID workload as Summer begins. 5/7 
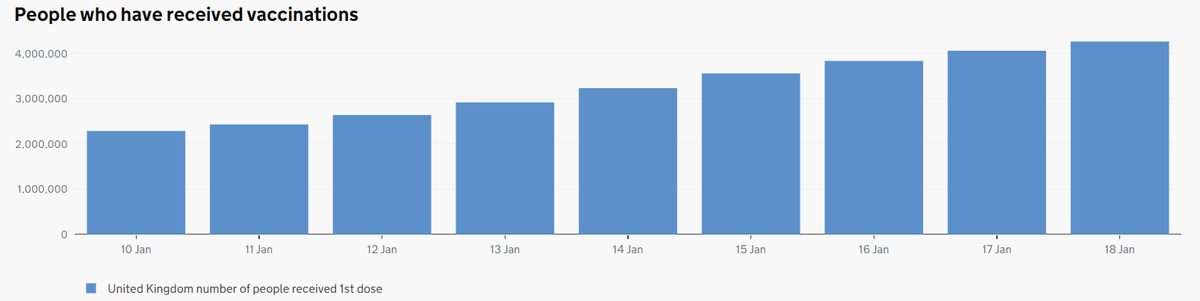
BUT vaccination roll out is impressive - 4 million people have now received their first dose. This is vital to preventing virus spread and protecting people from the disease COVID-19 (don't @ me about 2nd dose delay, I'm waiting for my 2nd while most have not had their 1st). 6/7 
Take home messages: 1) Infections may have peaked but pressure on hospitals is still rising; 2) Things may still be getting worse in your area; 3) #HandsFaceSpace remains vital; 4) The NHS will still be doing a lot of COVID care beyond June; 5) Have the vaccine when offered! 7/7
• • •
Missing some Tweet in this thread? You can try to
force a refresh











