We should take some of the most replicated findings in #MECFS and study them in #longCOVID patients. Some of these findings, if also present in #longCOVID, *could* potentially imply avenues for symptom management or therapeutic treatment.
Here are a few that might be interesting:
1️⃣Low serum carnitine: me-pedia.org/wiki/Carnitine
2️⃣ Low natural killer cell function: me-pedia.org/wiki/Natural_k…
3️⃣ Elevated lactate (blood, brain): me-pedia.org/wiki/Lactic_ac…
4️⃣ Cerebral hypoperfusion: me-pedia.org/wiki/Brain#Blo…
1️⃣Low serum carnitine: me-pedia.org/wiki/Carnitine
2️⃣ Low natural killer cell function: me-pedia.org/wiki/Natural_k…
3️⃣ Elevated lactate (blood, brain): me-pedia.org/wiki/Lactic_ac…
4️⃣ Cerebral hypoperfusion: me-pedia.org/wiki/Brain#Blo…
5️⃣ Low AMPK activation: me-pedia.org/wiki/List_of_a…
https://twitter.com/SimonBreidert/status/1353766519826763776?s=20
6️⃣ Increased mast cell populations: pubmed.ncbi.nlm.nih.gov/27362406/
7️⃣ Elevated muscarinic and B2-adrenergic receptor autoantibodies (also found in #POTS): me-pedia.org/wiki/Acetylcho…
8️⃣ Intestinal dysbiosis: me-pedia.org/wiki/List_of_a…
7️⃣ Elevated muscarinic and B2-adrenergic receptor autoantibodies (also found in #POTS): me-pedia.org/wiki/Acetylcho…
8️⃣ Intestinal dysbiosis: me-pedia.org/wiki/List_of_a…
9️⃣ Peripheral endothelial dysfunction: onlinelibrary.wiley.com/doi/full/10.10…
🔟 Low cardiac output/pre-load failure: me-pedia.org/wiki/List_of_a…
11. Small heart syndrome: me-pedia.org/wiki/Small_hea…
🔟 Low cardiac output/pre-load failure: me-pedia.org/wiki/List_of_a…
11. Small heart syndrome: me-pedia.org/wiki/Small_hea…
12. Elevated IgA (corresponds to illness severity): me-pedia.org/wiki/Immunoglo…
13. Low red blood cell magnesium: me-pedia.org/wiki/Magnesium
14. Impaired pyruvate dehydrogenase expression: me-pedia.org/wiki/Pyruvate_…
15. Increased glycolysis (anaerobic respiration): me-pedia.org/wiki/Glycolysi…
13. Low red blood cell magnesium: me-pedia.org/wiki/Magnesium
14. Impaired pyruvate dehydrogenase expression: me-pedia.org/wiki/Pyruvate_…
15. Increased glycolysis (anaerobic respiration): me-pedia.org/wiki/Glycolysi…
16. Reduced liver volume: tandfonline.com/doi/abs/10.108…
17. Increased risk of death from heart failure (average age, 58.7, conditional on having heart failure): pubmed.ncbi.nlm.nih.gov/16844674/
18. Cytokine dysregulation: me-pedia.org/wiki/Cytokine
17. Increased risk of death from heart failure (average age, 58.7, conditional on having heart failure): pubmed.ncbi.nlm.nih.gov/16844674/
18. Cytokine dysregulation: me-pedia.org/wiki/Cytokine
19. Persistent infection (enteroviral): me-pedia.org/wiki/Enterovir…
20. Neuroinflammation: me-pedia.org/wiki/Brain#Inf…
20. Neuroinflammation: me-pedia.org/wiki/Brain#Inf…
There is so much more than this. Here is a partial list: me-pedia.org/wiki/List_of_a… (many findings aren’t even on MEpedia yet, let alone this page—but anyone can contribute, so have a go!)
I want to underline the importance of #longCOVID researchers doing thorough reviews of the #MECFS, #POTS, #EDS, #MCAS, #fibromyalgia and #PTLD literatures so they can cite relevant research and compare and contrast their findings, embedding them within 50+ years of context.
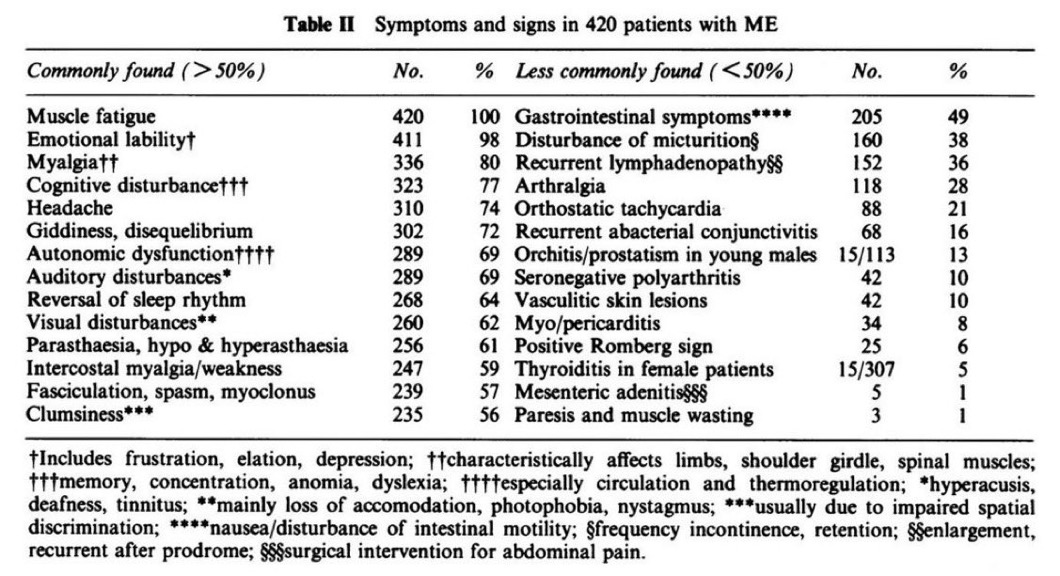
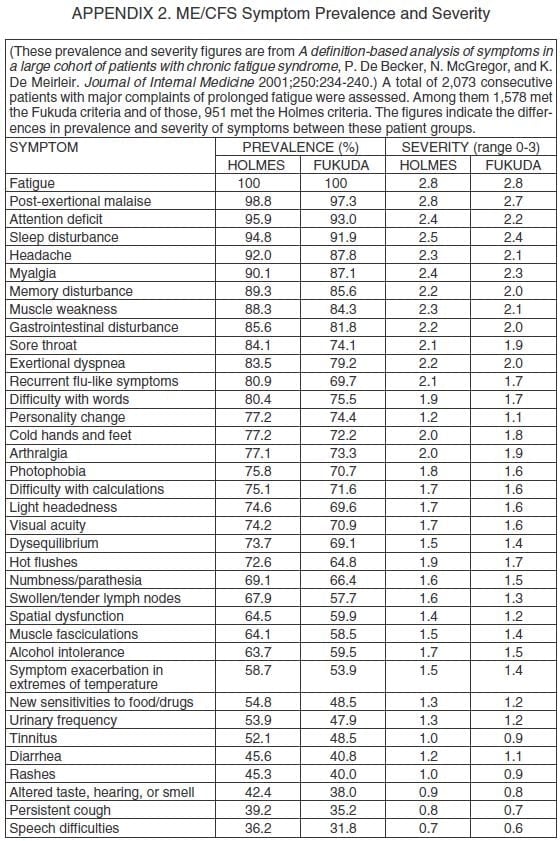
I also want to underline the history of 75+ outbreaks (me-pedia.org/wiki/Epidemic_…), which resulted in a % of those infected developing the attached symptoms, many of which should look...awfully familiar to anyone who has #longCOVID or treats people who do. 

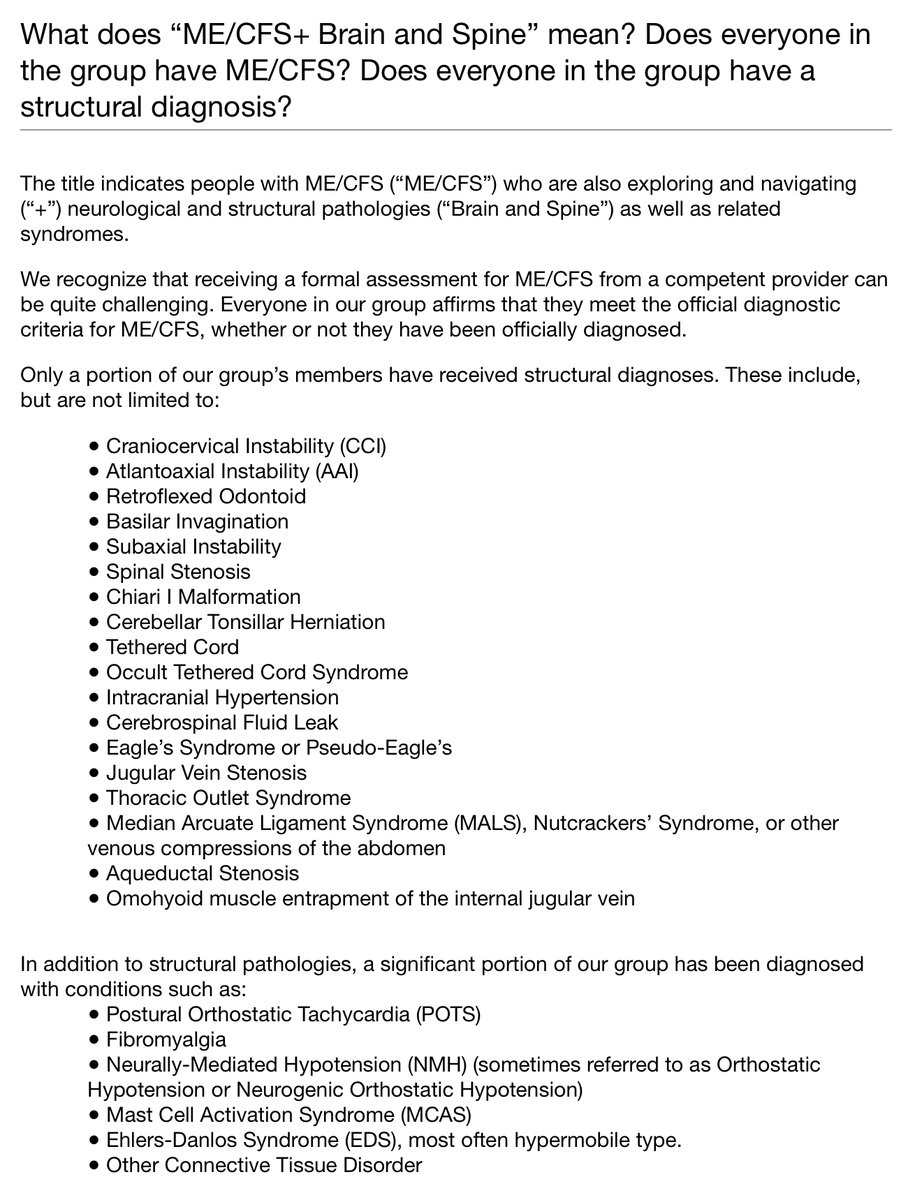
As well as the importance of recognizing the many possible comorbidities and overlapping syndromes that #longCOVID patients may be developing or are at risk for. me-pedia.org/wiki/Comorbidi…
Here’s how I think about this in the context of #MECFS:
https://twitter.com/jenbrea/status/1352675184038166529?s=20
Here’s how I think about this in the context of #longCOVID (as well as #MECFS):
https://twitter.com/jenbrea/status/1353372183456702467?s=20
Almost completely unstudied in #MECFS, but I believe of eminent importance, are mast cells (me-pedia.org/wiki/Mast_cell) and connective tissue (me-pedia.org/wiki/Collagen).
I think they help explain the “multi hit” hypothesis of #MECFS, which should be a hypothesis in #longCOVID, too.
I think they help explain the “multi hit” hypothesis of #MECFS, which should be a hypothesis in #longCOVID, too.
Here’s a bit more on the multi-hit hypothesis/equifinality: medium.com/@jenbrea/onset… (skip to the second half or read Parts I & 2).
Finally, it is estimated that 50% of #MECFS patients meet criteria for #hEDS or #HSD, me-pedia.org/wiki/Ehlers-Da…
Enough physicians are seeing connective tissue disease in #longCOVID, there’s a new ICD code for it:
Enough physicians are seeing connective tissue disease in #longCOVID, there’s a new ICD code for it:
https://twitter.com/AlisonSbrana/status/1350273115285147650?s=20
Inflammatory connective tissue damage, at multiple sites, causing a dizzying array of possible pathologies unique to each patient, that some patients *will ‘spontaneously’ heal from with time, but others will not, with an overlay of #MCAS, might just be was pathogens can do...
If you got to the end, congrats!! What are other major findings/areas of inquiry in #MECFS #POTS #EDS #MCAS #fibro #PTLD that you think #longCOVID researchers and clinicians should know about?
Also gonna leave these links here...
1️⃣US ME/CFS Clinician Coalition: mecfscliniciancoalition.org
2️⃣#longCOVID and #MECFS: Understanding the connection: meaction.net/long-covid-me-…
1️⃣US ME/CFS Clinician Coalition: mecfscliniciancoalition.org
2️⃣#longCOVID and #MECFS: Understanding the connection: meaction.net/long-covid-me-…
...and copy in some cool folks in research & medicine. Please share with any colleagues who might be interested. I think engaging with this literature is so important. @evolutionarypsy @ahandvanish @YoniFreedhoff @ScottGottliebMD @ShannonOMac @Dr2NisreenAlwan @trishgreenhalgh
@MatthewMarkert @WesElyMD @acweyand @arghavan_salles @VirusesImmunity @ErinSandersNP @choo_ek @janevandis @DocElovitz @uche_blackstock @meganranney @RanaAwdish @Cleavon_MD
@AlanLevinovitz @AlanaKinrich @EricTopol @BendyBrain @DrOniBee @drjessigold @amarkelkar @LeahNTorres @sczerwas @AdvocacyMD @drnatalietv @daniel_kraft @NINDSdirector @DrEReinhold
Do any of these findings surprise you?
• • •
Missing some Tweet in this thread? You can try to
force a refresh