You asked. So here are my thoughts on how osteopathic medical students should respond to the NBOME.
(thread)
(thread)
https://twitter.com/jberg521/status/1354917879116947465
Look, even before the Step 2 CS cancellation, my DMs and email were flooded with messages from osteopathic medical students who are fed up with the NBOME.
There is *real* anger toward this organization. Honestly, more than I even heard about from MD students and the NBME.
There is *real* anger toward this organization. Honestly, more than I even heard about from MD students and the NBME.
The question is, will that sentiment translate into action?
Amorphous anger on social media is easy to ignore. But if that anger gets channeled into organized efforts to facilitate change, then improvements are possible.
Amorphous anger on social media is easy to ignore. But if that anger gets channeled into organized efforts to facilitate change, then improvements are possible.
This much should be clear: begging the NBOME to reconsider their Level 2-PE exam is a waste of your time.
Best case scenario, you’ll get another “town hall” meeting, a handful of platitudes, and some thoughtful beard stroking before being told that they’re keeping the exam.
Best case scenario, you’ll get another “town hall” meeting, a handful of platitudes, and some thoughtful beard stroking before being told that they’re keeping the exam.
Instead of complaining to the NBOME, here are a few things that are more likely to bring about real change.
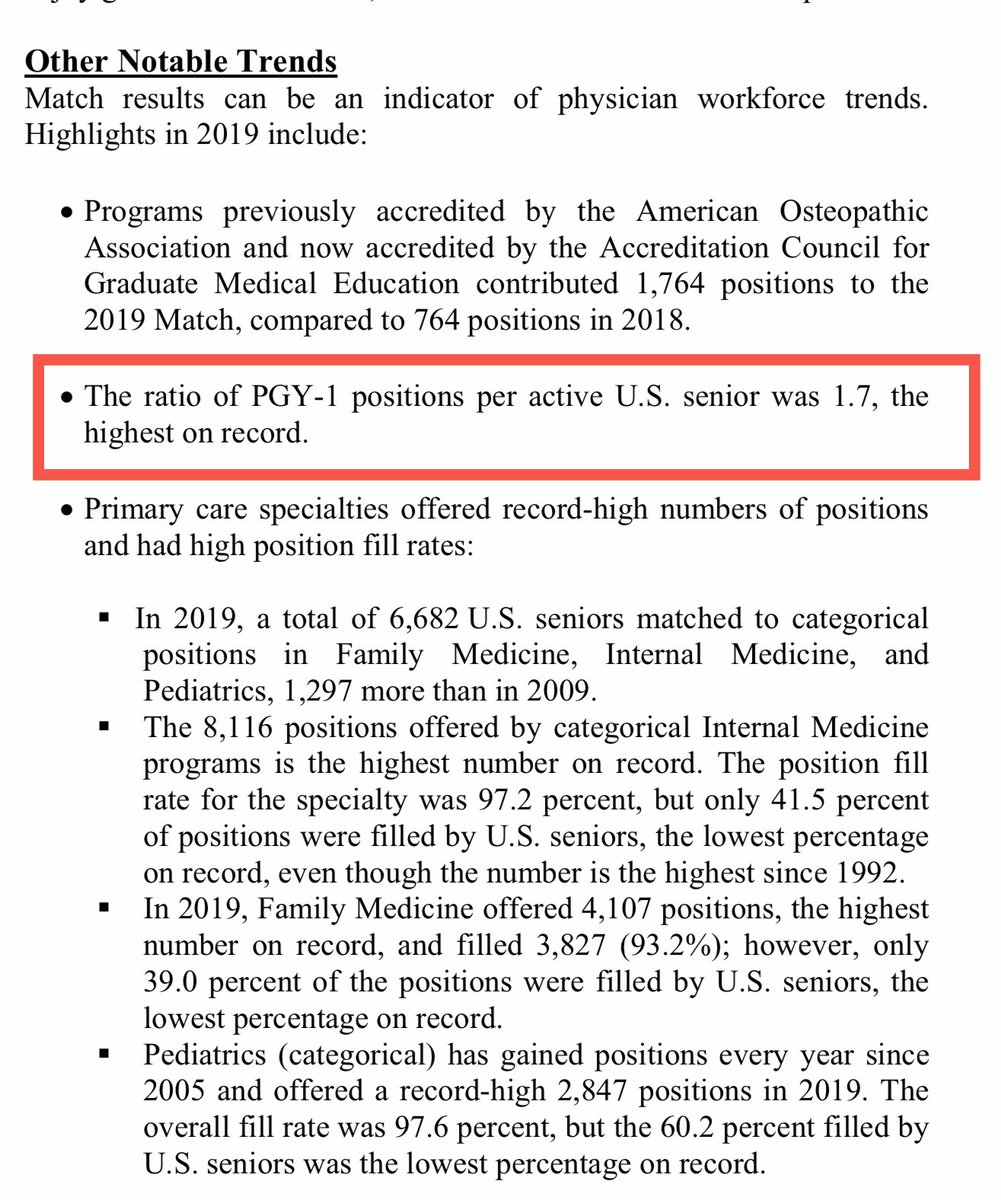
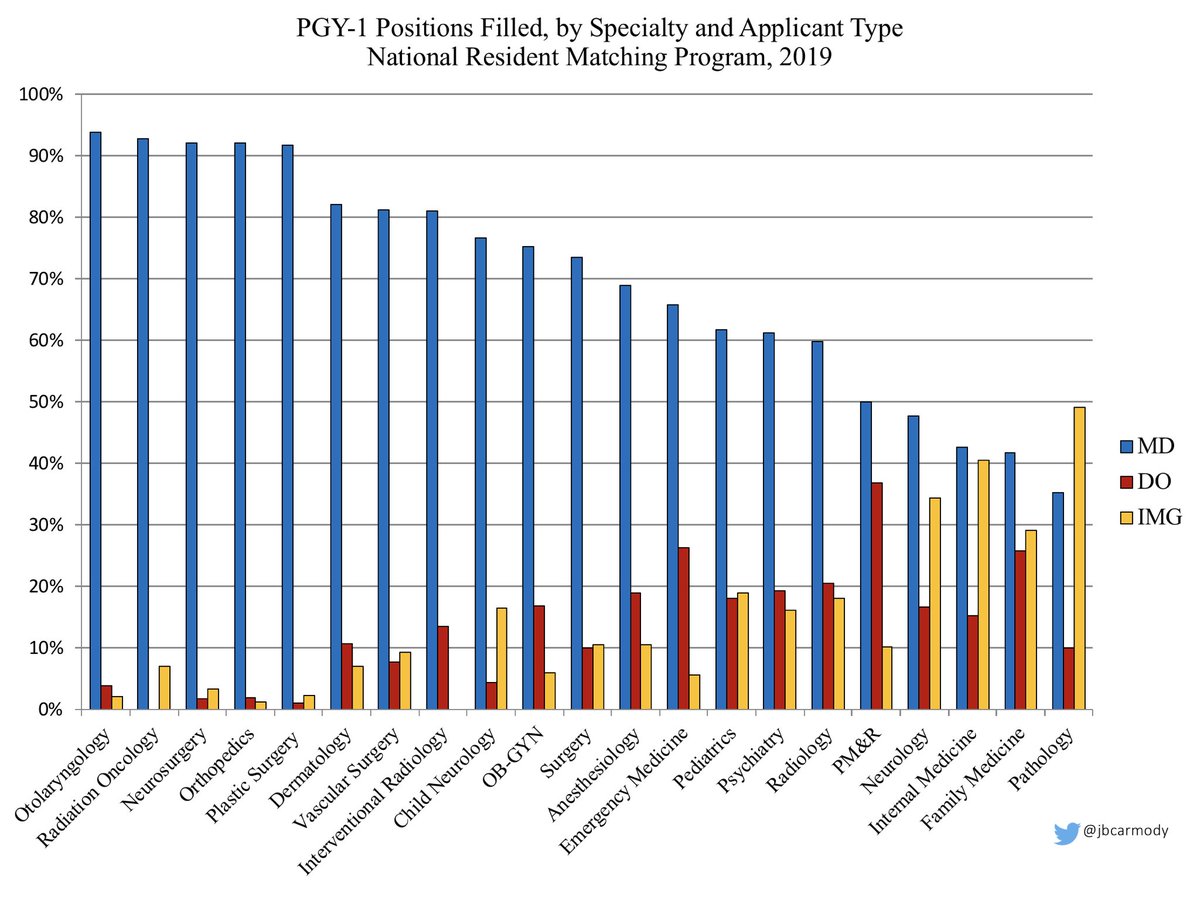
1) Vote with your wallets: take USMLE Step 3.
Almost all states allow DO licensure by completing the USMLE series. If you aren’t required to engage with the NBOME, don’t.
Almost all states allow DO licensure by completing the USMLE series. If you aren’t required to engage with the NBOME, don’t.
2) Lobby the state boards that don’t allow the USMLE.
As an MD who has passed the USMLE, I could practice in any state. Why shouldn’t a DO who passed the USMLE be able to do the same?
(State boards that prop up the NBOME with a COMLEX requirement are listed in the Tweet below.)
As an MD who has passed the USMLE, I could practice in any state. Why shouldn’t a DO who passed the USMLE be able to do the same?
(State boards that prop up the NBOME with a COMLEX requirement are listed in the Tweet below.)
https://twitter.com/mustafabasree/status/1354156848522403842
If you intend to practice in one of these states, talk to your state representative. Explain how the medical board is providing a deterrent to DOs serving patients in their state.
The board may be friendly with the NBOME, but they’re still accountable to the legislature.
The board may be friendly with the NBOME, but they’re still accountable to the legislature.
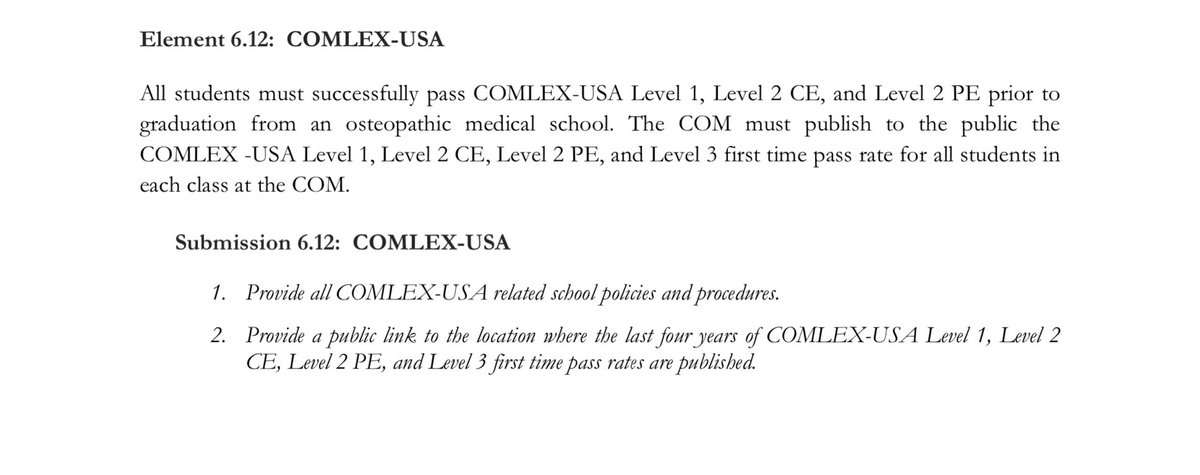
3) Lobby the AOA to change the COCA accreditation requirements that compel schools to require COMLEX-USA.
It’s ultimately the COCA requirement that keeps the NBOME in business.
It’s ultimately the COCA requirement that keeps the NBOME in business.
The AOA is the professional body ultimately responsible for securing the success of the osteopathic profession.
They should think carefully about whether, at this point in history, a “separate but equal” licensing exam hurts DOs more than it helps.
thesheriffofsodium.com/2020/10/24/the…
They should think carefully about whether, at this point in history, a “separate but equal” licensing exam hurts DOs more than it helps.
thesheriffofsodium.com/2020/10/24/the…
As a sidenote:
The LCME’s accreditation standards for MD schools are more stringent than COCA’s for COMs - and even they never mandated the USMLE.
(Still, most schools did - since the requirement gave access to student loans to cover registration fees).
Let the schools decide.
The LCME’s accreditation standards for MD schools are more stringent than COCA’s for COMs - and even they never mandated the USMLE.
(Still, most schools did - since the requirement gave access to student loans to cover registration fees).
Let the schools decide.

Last thing:
Don’t feel guilty about pursuing these tactics. None of them are underhanded. Market forces and political action are how things are supposed to work in America - and they’ll be needed to move an entrenched, monopolistic bureaucracy that ignores its constituents.
Don’t feel guilty about pursuing these tactics. None of them are underhanded. Market forces and political action are how things are supposed to work in America - and they’ll be needed to move an entrenched, monopolistic bureaucracy that ignores its constituents.
• • •
Missing some Tweet in this thread? You can try to
force a refresh